Echinococcosis
Clemens Gödel is a freelancer for the medical team.
More about the experts All content is checked by medical journalists.Echinococcosis is a potentially life-threatening infection with the fox or dog tapeworm. The symptoms depend on the organ affected. In most cases the liver is affected. Find out here about the symptoms, diagnosis and treatment of echinococcosis.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. B67
Echinococcosis: description
Echinococcosis is a worm disease that is usually caused by parasitic dog or fox tapeworms. A distinction is made between two very different clinical pictures: on the one hand, alveolar echinococcosis caused by the small fox tapeworm (Echinococcus multilocularis) and, on the other hand, cystic echinococcosis, which is caused by the small dog tapeworm (Echinococcus granulosus).
While the dog tapeworm is a global problem, the fox tapeworm only occurs in certain regions, including Central Europe and especially southern Germany. In 2014 there were 66 cases of cystic echinococcosis across Germany. The Robert Koch Institute reports that 16 people were affected by alveolar echinococcosis. In these regions up to 75 percent of the foxes are infested with the small fox tapeworm. The average age of onset of infection with the fox tapeworm is between 50 and 60 years. Children and adolescents are rarely affected. The echinococcosis caused by the dog tapeworm affects all age groups.
What are tapeworms?
Tapeworms (cestodes) are parasites. They consist of a head with suckers and barbs, a neck and a long, band-shaped body. This is divided into individual, similarly structured sections. Tapeworms are hermaphrodites that have no intestines and therefore absorb food through the skin.
A tapeworm goes through various stages in the course of its development. Depending on the stage, it moves to a different host. Carnivorous animals, especially foxes and dogs, and more rarely cats, ingest the larvae by consuming the meat of an infected animal. In the intestines of these final hosts, the larvae develop into tapeworms that lay eggs. It does this by always shedding the last limb of its body, which is filled with eggs. A dog tapeworm can lay around 1,500 per part of the body - a fox tapeworm around 200. The eggs are excreted in the feces and in turn taken up by an intermediate host (e.g. mice), where they form a type of cyst or encapsulation, especially in the liver. Humans can also inadvertently serve as intermediate hosts.
Echinococcosis: symptoms
Echinococcosis can remain completely normal for many years. During this time, the cysts get bigger and bigger and can affect the organs in which they are located. This can reveal echinococcosis: Echinococcosis displaces or infiltrates organs and leads to a feeling of pressure and compression of nerves, vessels or organs. The symptoms depend heavily on the organ affected. An additional infection with bacteria is also possible. Non-specific symptoms such as malaise, weight loss and allergic reactions can also occur.
liver
Echinococcosis affects the liver in around 70 percent of cases. The consequences are a feeling of pressure and pain in the right upper abdomen. If the worm infestation obstructs the flow of bile, the skin and eyes may turn yellow (jaundice). This can result in inflammation of the biliary tract (cholangitis), liver cirrhosis and a blockage of the portal vein that carries the blood to the liver (portal hypertension).
lung
Around 20 percent of dog tapeworm infections are in the lungs. In the case of fox tapeworm infections, however, the lung infestation is rare. The main symptom is a cough, sometimes with blood. In addition, those affected suffer from pain and breathing disorders.
No organ is protected from echinococcosis!
Especially in the context of cystic echinococcosis, cysts can also occasionally be found in the brain, spleen, heart, bones and other organs. The infestation can take place via the bloodstream, the lymph, but also by direct sowing in the abdominal or chest cavity.
Echinococcosis: causes and risk factors
For the fox and the dog tapeworm, humans are a false intermediate host. The larvae nest in various organs, but rarely or never develop into worms. In those affected, whose immune system is impaired by illness or therapy, the disease can be more severe.
Infection with the tapeworms occurs in the vast majority of cases through food, which contains eggs from the feces of infected animals. In particular, the consumption of unwashed berries, windfalls or fruits from low shrubs carries a high risk of infection. But it is also possible to get infected by eating raw meat.
After ingestion, the eggs usually first enter the liver through the intestinal blood vessels. From there they can reach other organs in the course of the process. In the organs, the eggs develop into larvae, which encapsulate themselves in a tumor-like manner and may take years to become noticeable.
No human-to-human transmission
The disease is not transmitted from person to person. There is usually no risk of infection from sick people. The operated material is also considered non-infectious.
Dog and fox tapeworms have very different growth patterns, which are decisive for the different courses of the two worm diseases:
The dog tapeworm forms cysts in the organs. Cysts are fluid-filled cavities. Cysts caused by the dog tapeworm displace the surrounding tissue and are usually single. The cysts cause the body's own tissue to form a wall around them.
The alveolar echinococcosis caused by the fox tapeworm leads to infiltration of the organs - similar to a cancerous ulcer. In addition, they are sponge-like and built up like chambers when they are stored together.
Echinococcosis: examinations and diagnosis
First of all, if you suspect a worm infestation, you should contact an infectiologist. However, care and treatment for echinococcosis should be done in a specialized center for worm infections. Since a third of all cases are incidental, most of those affected will be referred to a specialist immediately after the findings have been made. The doctor will ask these questions, among others:
- Have you ever been diagnosed with worms or other parasites?
- Have any inexplicable abnormalities been found in previous examinations?
- Do you feel pain or pressure in the right upper abdomen?
- Do you suffer from (inexplicable) diseases of the lungs (e.g. cough)?
- Do you have any previous illnesses?
- What medications are you taking?
The most important diagnostic tool for echinococcosis is imaging. Ultrasound, MRI and CT technology can be used to locate the affected organs. Due to the frequent calcification of the cysts, they are easily visible. So foci of a cystic echinococcosis are smoothly demarcated and calcified especially at the edge. Their daughter cysts typically have a double contour in the wall and a honeycomb structure. Usually an ultrasound examination is carried out first. Already with the help of this examination abnormalities in the liver can be determined. Imaging is important because a cyst should never be punctured if echinococcosis is suspected, as it could spread eggs throughout the body.
Further investigations
A blood test is also part of the clarification of echinococcosis. In the standard blood test, an increase in a subgroup of white blood cells (eosinophils) can be noticed in around ten percent of the cases. It is believed that the eosinophils have a role in the defense against worms. The doctor should send the drawn blood to a laboratory that specializes in echinococcosis. Shipping can take a little longer than local laboratory tests, but specialized laboratories can deliver better quality results. There, worm-specific antibodies and antigens can be identified and examined. A negative blood test does not rule out echinococcosis.
However, neither image nor blood tests cannot make a definitive diagnosis. A report to the Robert Koch Institute is always necessary if the findings are clear. For this reason, if there is justified suspicion, the final diagnosis should be carried out at an experienced center, for example at the University Hospital Würzburg, the consulting laboratory of the Robert Koch Institute.
The definitive diagnosis can be made by a pathological examination of material removed after an operation. With the help of the PNM classification, fox tapeworm infestation in particular can be assessed. This classification takes into account the involvement of the liver (P), the neighboring organs (N) and existing metastases (M).
A special imaging examination, the FDG-PET, can be used to monitor therapy. This technique can be used to test the activity of the worm hydatids.
More common than echinococcosis are liver tumors, which can look very similar on imaging. A number of other alternative diagnoses are conceivable. These include various benign and malignant tumors, other types of cysts, abscesses or even tuberculosis.
Echinococcosis: treatment
The treatment of echinococcosis is reserved for specialized centers. Sometimes it has to be carried out over a period of years or even for a lifetime.
Operative removal
The only curative therapy for echinococcosis according to the current state of science is a total surgical removal of the affected areas. This possibility should always be checked. On the other hand, in rare cases, a wait-and-see strategy can be considered under close observation.
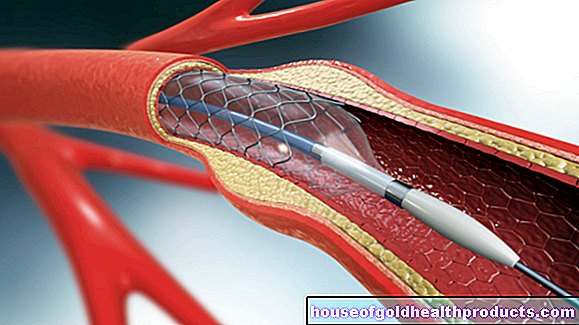
For cystic echinococcosis, radical cyst removal is attempted or the PAIR procedure is used. In this procedure, 95 percent alcohol is injected into the cyst through the skin. The PAIR procedure may only be performed after excluding a connection between the cyst and the biliary tract and in combination with chemotherapy with albendazole. If echinococcal cysts burst during the procedure, the worm's brood capsules can be sown. These can cause a severe allergic reaction. To avoid this, there should be a sufficient distance of about two centimeters between the cysts and the surface of the liver. In over 50 percent of the cases, the cysts can be completely removed.
Alveolar echinococcosis is also treated by removing the worm foci. However, complete removal is only possible in around a quarter of all cases. In alveolar echinococcosis, drug therapy is more important than in cystic echinococcosis.
In exceptional cases, a liver transplant can be considered.
Medication
In addition or as an alternative to the operation, a benzimidazole such as albendazole or mebendazole is used for a longer period of time. Drug therapy alone may be necessary if surgery is not possible. These drugs belong to the group of anti-worm drugs (antihelmetics) and inhibit the progression of echinococcosis, but do not kill it. The good absorption of these drugs is only ensured when fat is consumed at the same time. Regular blood tests with differential blood counts and determination of liver values and creatinine must be carried out during therapy.
Contraindications to drug therapy are the risk of a cyst rupture. In the case of liver disease and bone marrow depression, it must be weighed whether the administration of medication makes sense. Therapy should be paused, especially in early pregnancy, as the medication can damage the fruit.
For cystic echinococcosis, antihelmetic therapy is given for at least six months if the cysts are inoperable or if complications occur during the operation. In the case of sowing cystic echinococcosis in the abdominal cavity, for example after an operation, albendazole therapy should be carried out for six months.
Due to the generally poor prognosis, the treatment plans for alveolar echinococcosis are longer. If surgery is not possible, life-long anti-worm therapy is necessary. In the event of a successful operation, drug treatment for two years is recommended.
Echinococcosis: prevention
Every echinococcosis must be reported to the RKI in order to monitor the infection situation.
To protect yourself from echinococcosis, contact with (dead) foxes and unfamiliar dogs in risk areas should be reduced. Own dogs should be dewormed regularly. Dogs imported from southern countries should also be urgently dewormed. Depending on the risk of infection, this should be done in consultation with the veterinarian. Meat inspection and the proper disposal of slaughterhouse waste in risk areas are also important basic measures. Raw meat can contain echinococci.
Fruits from low shrubs and windfalls must be washed thoroughly. There is a possibility that these are contaminated with tapeworms from fecal residues. Collecting mushrooms and plants in the forest carries a similar risk. The echinococci can remain infectious for months under good conditions. However, brief boiling will kill them. It is also useful to dry fruits. Cooling does not harm them, however, temperatures below 80 degrees over several days would kill them - at least that is certain for alveolar echinococcosis.
After contact with infected animals, checks should be carried out routinely after four weeks and after six, twelve and 24 months. Antibodies should also be searched for in the blood. This means that therapy can be initiated early if necessary.If the risk of infection is permanent, a check should be carried out every six months. Fox tapeworm disease is an occupational disease among farmers.
Echinococcosis: disease course and prognosis
Echinococcosis can be fatal. If left untreated, the majority of those affected die. However, the prognosis of properly treated echinococcosis caused by the canine and fox tapeworm are very different.
While only 30 percent of the people infected with the fox tapeworm are still alive after ten years, the probability of survival from a dog tapeworm is good. This is because fox tapeworm cysts are usually much easier to operate. The complete removal of the fox tapeworm infestation is seldom possible. However, lifelong drug therapy for alveolar echinococcosis can prevent a fatal course. Relapses are always possible. In around 15 percent of all cystic echinococcoses, the disease reappears after an initially successful therapy. The success of the therapy and the course of the disease should be monitored regularly with an imaging method, e.g. ultrasound, and by measuring the antibody level.
An acutely life-threatening complication of echinococcosis is the sowing of the larvae, for example through a cyst rupture. The sowing can, among other things, lead to peritonitis.
Tags: drugs alcohol toadstool poison plants