Inflammation of the salivary glands
Mareike Müller is a freelance writer in the medical department and assistant doctor for neurosurgery in Düsseldorf. She studied human medicine in Magdeburg and gained a lot of practical medical experience during her stays abroad on four different continents.
More about the experts All content is checked by medical journalists.Inflammation of the salivary glands (sialadenitis, sialoadenitis) affects the large head salivary glands. It can occur at any age and is triggered by various causes. Patients are often in pain and notice swelling in the affected gland. With the right therapy, salivary gland inflammation usually heals without consequences. Read everything you need to know about salivary gland inflammation here.
What is salivary gland inflammation?
Medical professionals understand inflammation of the salivary glands as inflammation of the large head salivary glands. These include:
- Parotid glands (glandula parotidea): They produce a watery secretion.
- Submaxillary glands (glandula submandibularis): They produce a slimy-watery secretion.
- Sublingual glands (glandula sublingualis): They produce a slimy secretion.
In addition to the large head salivary glands, there are around 1000 small glands that are distributed throughout the mouth and contribute to saliva production.
Inflammation of the parotid gland
You can find everything you need to know about inflammation of the parotid gland in the article Parotitis.
Salivary gland inflammation: symptoms
A distinction is made between acute and chronic inflammation of the salivary glands. Acute sialadenitis often manifests itself with the following sudden symptoms (especially when triggered by bacteria):
- pains
- Swelling of the gland
- Pressure sensitivity
- hard, coarse consistency
- hot, red skin over the gland
- Fever, chills
- Swelling of the lymph nodes
- general feeling of illness, fatigue
Pus may drain into the oral cavity through the ducts. The swelling and pain in the gland increase when you eat because chewing stimulates saliva production. In about 80 percent of the cases, the salivary gland inflammation occurs only on one side.
Salivary gland inflammation: symptoms of an acute viral infection
If viruses are the cause of an acute inflammation of the salivary glands, the symptoms begin about one to two weeks after infection (incubation period). In contrast to a bacterial infection, the secretion that emerges is watery and not purulent.
Inflammation of the salivary glands: signs of chronic inflammation
Chronic, recurring sialadenitis progresses slowly and in flares. The gland is painfully swollen. Purulent or milky-grainy secretion may emerge. The chronic inflammation of the salivary glands is usually unilateral. She can also switch between the pages.
Salivary gland inflammation: causes
There are many causes of salivary gland inflammation. While children are more likely to develop inflammation of the parotid gland caused by the mumps virus, older people are more likely to suffer from recurrent bacterial infections. Overall, sialadenitis can have the following causes:
- Decreased saliva production: especially in older people due to a small amount of fluids or poor appetite, alcohol abuse, salivary stones, tumors or scarred salivary ducts
- poor oral hygiene, rotten teeth, inflammation of the oral mucosa
- Medicines such as antidepressants, diuretics, antihistamines, beta blockers, calcium antagonists
- Autoimmune diseases such as Sjogren's syndrome or Heerfordt's syndrome
- Radiation therapy of the head and neck region or radio-iodine therapy for thyroid disease
- Disturbances of the salt and water balance
- chronic diseases like diabetes mellitus or AIDS
Especially when the production or flow of saliva is disturbed, bacteria can rise from the mouth into the ducts of the salivary glands. There they can multiply and cause inflammation. They include streptococci, staphylococci, Escherichia coli and Pseudomonas, among others.
Viruses usually cause inflammation of the salivary glands by getting into the gland through the blood. Typical pathogens include the Epstein-Barr virus, cytomegalovirus, mumps virus and influenza virus.
Salivary gland inflammation: diagnostics
If the swelling in the head or mouth area persists, pain is severe, and additional symptoms are present, you should consult a doctor. An ear, nose and throat doctor is the right person to talk to if you have sialadenitis. Before he examines you, he will first ask you in detail about your medical history (anamnesis). Possible questions are:
- Since when are you having those complaints?
- Are there triggers that make symptoms worse?
- Do you suffer from a chronic illness such as AIDS, diabetes mellitus or rheumatism?
- Do you regularly take medication?
- Have you had radiation treatment of your head or neck?
Salivary gland inflammation: physical examination
Your doctor will then examine you. First he looks at the affected area. He looks to see if there is any swelling or if the skin over the gland is red. He then searches the oral cavity for redness in the ducts or pus. He also scans the salivary glands to detect any swelling or hardening. He can also try massaging pus.
In the next step, your doctor can take a swab of the saliva and examine it for pathogens. A blood sample can also be helpful. The so-called inflammation parameters are determined in the laboratory. These include the C-reactive protein, the rate of sedimentation and the number of white blood cells (leukocytes). Your doctor can use these values to determine if there is inflammation in your body.
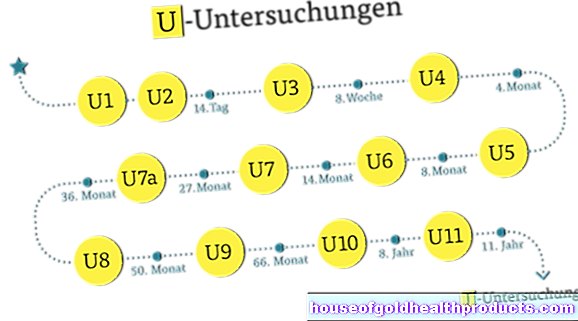
Salivary gland inflammation: further studies
The diagnosis of mumps and acute purulent inflammation of the salivary gland can usually be easily made on the basis of the symptoms and medical history. In order to differentiate between other causes, further examinations may be necessary, such as an ultrasound examination (sonography), magnetic resonance imaging (MRT), computed tomography (CT) or endoscopy. In endoscopy, a tiny camera is pushed through the ducts of the glands. The pathways and glands can be visualized, tissue samples can be taken and irrigation can be carried out.
Salivary gland inflammation: therapy
The therapy of salivary gland inflammation depends on the cause. Bacterial infections are treated with antibiotics. They kill bacteria or prevent them from multiplying. The active ingredients cefuroxime or clindamycin are often used for inflammation of the salivary glands. In order to treat the bacteria specifically, an antibiogram can be made that shows which antibiotics are best.
Antibiotics do not help against viruses. In the case of a virus-related salivary gland inflammation, only the symptoms can be treated (symptomatic therapy). For example, the doctor may prescribe painkillers that also have anti-inflammatory or fever-lowering effects, such as ibuprofen or paracetamol. Also, cool compresses can help relieve pain.
It is also advisable to consume saliva-stimulating foods such as candy, chewing gum or lemon. You should also observe good oral hygiene, drink plenty of fluids and prefer soft foods.
If an autoimmune disease is causing the salivary gland inflammation, your doctor may prescribe glucocorticoids (cortisone). They suppress the immune system and thus inhibit the inflammatory reaction.
If drugs are suspected of causing inflammation of the salivary glands in you, their use should be interrupted if possible.
Salivary gland inflammation: prognosis
If the salivary gland inflammation is treated correctly in good time, it will usually heal within a few days without any consequences.
Without suitable therapy, however, sialadenitis can recur again and again. In such cases, surgical removal of the gland may be the only treatment option. This is usually possible without any problems because the other salivary glands produce enough saliva. However, there is a great risk that the facial nerve will be injured during the procedure and that the affected half of the face can no longer be moved or only partially moved.
If a bacterial purulent inflammation of the salivary gland is not treated, a purulent encapsulation (abscess) can form. This can break through into the mouth, ear canal or through the neck tissue to the outside. If the triggering bacteria get into the bloodstream, potentially life-threatening sepsis ("blood poisoning") develops.
If chronic inflammation of the salivary gland is left untreated, the glandular tissue can scar or recede.
Tags: healthy workplace diet menopause














.jpg)