Torticollis
Marian Grosser studied human medicine in Munich. In addition, the doctor, who was interested in many things, dared to make some exciting detours: studying philosophy and art history, working on the radio and, finally, also for a Netdoctor.
More about the experts All content is checked by medical journalists.The term torticollis comes from Latin and means something like "twisted" or "curved" neck. Another name for torticollis is therefore torticollis. Affected people actually have a crooked neck and can only move their head to a limited extent. There are many possible causes for this. Treatment and prognosis are also variable. Read more about the torticollis symptom, its causes and treatment options here.

Brief description
- What is torticollis? Fixed inclination of the head, which can be differently pronounced
- Causes of torticollis: e.g. congenital muscle shortening, malformation or misalignment of cervical vertebrae, infections, inflammation in the neck area, larger scars on the neck, vision or hearing problems
- Therapy of a torticollis: depending on the cause, e.g. B. with medication, physiotherapy or surgery
- When to the doctor Always - there can be a serious cause behind a torticollis that should be treated!
Torticollis: definition
The term “torticollis” generally describes a tilted position of the head, which happens involuntarily. Affected people can either not lift it at all or only with pain for a short time. The extent of the bad posture varies and depends on the cause.
Forms of torticollis
Depending on the position of the fixed malposition, doctors differentiate between different types of torticollis:
- rotatory torticollis: the head is turned.
- Laterocollis: The head is inclined towards the shoulder.
- Anterocollis: the head is tilted forward.
- Retrocollis: The head is tilted backwards.
With muscular involvement in the fixed deformity, a torticollis can be subdivided even more precisely. Strictly speaking, it is only a torticollis if the oblique posture is caused by the muscles that act on the cervical spine. However, those neck muscles that attach directly to the skull can also be the cause of the incorrect posture. One speaks then, for example, of a torticaput or a laterocaput.
Different types of torticollis can also occur in combination. The neck can be rotated and inclined towards the shoulder at about the same time.
A torticollis can also be defined by its cause. There are then other types of torticollis such as torticollis osseus (osseous torticollis), which are described in more detail below in the section "Causes and possible diseases".
Because there are so many different varieties of torticollis, it is difficult to pinpoint the exact frequency of this symptom. Overall, torticollis is rare.
Torticollis: causes and possible diseases
As mentioned, there are many different triggers for torticollis. Some of them exist from birth. In other cases, a torticollis does not develop until later in life (in middle adulthood). Some variants are only temporary, others cannot be permanently cured.
Torticollis muscularis congenitus
The term can be translated as "congenital muscular torticollis". This form of torticollis occurs in newborns. Immediately after birth, the crooked head position can be recognized in the affected babies. The reason is the shortening of the muscles - more precisely, a shortening of the sternocleidomastoid (also known as the "nodding muscle" or "large head turner").
This muscle arises from the sternum and collarbone and starts just behind and below the ear. Everyone has one such muscle on the left and right side of the neck. If both are activated at the same time, the head is pulled towards the chest; with one-sided activation, on the other hand, the head tilts towards the shoulder and simultaneously rotates towards the opposite side.
In rare cases, the nodding muscle on one side of the body (usually the right) does not develop properly during pregnancy. Instead of muscle fibers, connective tissue is created and the muscle is too short. Accordingly, this imbalance pulls the baby's head to one side - a torticollis is created.
It is not yet clear why the muscle in question is not properly developed. Sometimes the muscle is also damaged during labor. Then a muscular torticollis can also result.
In many infants with such a torticollis, swelling also occurs in the lower third of the affected nod after one to two weeks. It initially increases, but usually disappears again after six months.
Torticollis osseus
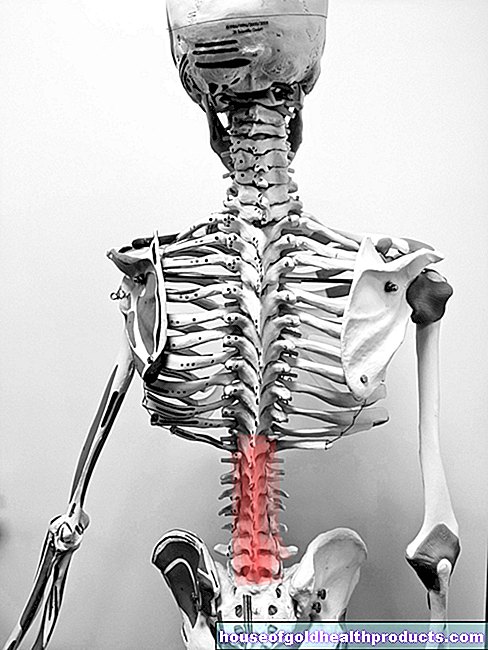
The cause of the osseous torticollis is not in the area of the muscles, but in the cervical spine. If the individual vertebrae are deformed or incorrectly positioned, this can result in a crooked head position. The bony malformations or positions can be congenital (hemivertebra, Klippel-Feil syndrome) or arise in the course of life, for example through incorrectly healed bone fractures (fractures) in the cervical spine.
Torticollis rheumaticus
If the vertebral joints of the cervical spine are painful as a result of a rheumatic disease and in this way cause a torticollis, this torticollis rheumaticus is called.
Torticollis spasticus
This variant of torticollis is also called "cervical dystonia" and has a neurological background, that is, it originates from the nervous system. Dystonias are movement disorders with uncontrollable contraction of the muscles. They are based on malfunctions in the centers of the brain that are responsible for movement.
In the case of torticollis spasticus, dystonia is present, which affects the neck and especially the head nodding muscle. This leads to involuntary muscle tension (spasms) with abnormal head positions and head movements. Often it is also associated with pain. People between the ages of 30 and 50 are particularly affected.
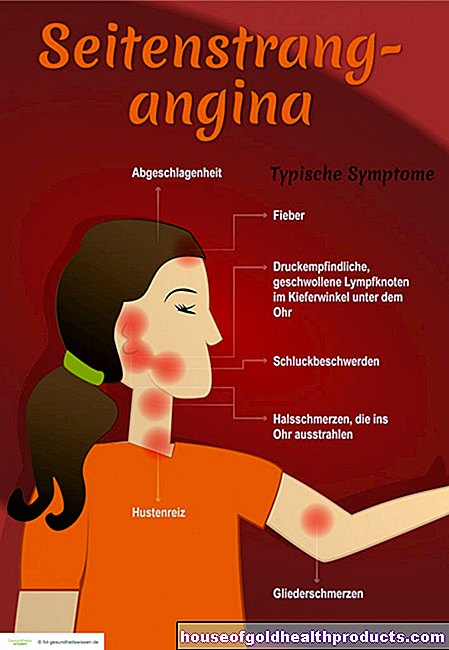
Torticollis infectiosus
Infectious torticollis is an indirect sign of inflammation in the neck area. Especially if, for example, a laryngitis or tonsillitis is not adequately treated with antibiotics, complications can arise and the symptoms worsen. Because of the sometimes severe pain, those affected take a gentle posture on the inflamed side - they have a crooked neck.
Torticollis infectiosus can also develop in abscesses caused by tonsillitis or acute inflammation of the lymph nodes in the neck area.
Torticollis acutus
The acute torticollis can be traced back to a cervical spine syndrome - a collective term for various complaints, all of which can be traced back to a damaged cervical spine (cervical spine). The damage is based, for example, on wear and tear or an accident. Under certain circumstances, the intervertebral discs shift and irritate certain nerves, which leads to a relieving posture with a crooked neck.
Cutaneous torticollis
If larger scars develop on the neck as a result of surgery or injuries, this can shorten the skin (Latin: cutis) and the muscles on one side, causing the head to lean towards it. This is why this type of torticollis is also known as the torticollis.
Torticollis ocularis
This form of the torticollis is actually an exception, because in contrast to the other variants, the tilted position of the head is not mandatory here. Rather, those affected tend to tilt their heads to compensate for a visual impairment.
For example, an ocular torticollis can develop when one of the eye muscles is paralyzed. Because of this paralysis, patients see double vision as soon as they look in the direction of the damaged muscle. By turning your head in such a way that the failure of the muscle is no longer significant, you avoid the double vision.
Torticollis acousticus
The situation is similar with torticollis acousticus (otogenic torticollis). Here, too, the tilt of the head is only a compensatory movement, in this case because of a one-sided hearing impairment. It is therefore important in children with torticollis to consider the possibility of hearing loss when looking for the cause.
Other causes
In addition to the causes mentioned, tumors in the neck or brain area can also trigger a torticollis, as well as a stroke and some metabolic disorders. In rare cases, certain drugs that act on the brain can trigger a torticollis.
Torticollis: what does the doctor do?
The torticollis can be identified by eye diagnosis. In order to be able to clarify the exact cause, however, various examinations are usually necessary.
Investigations
In a conversation with the patient, the doctor first collects the patient's medical history (anamnesis): He asks the patient precisely about their complaints, any accompanying symptoms as well as previous illnesses or accidents. Based on this information, the medical professional can narrow down the possible triggers.
This is followed by various examinations depending on the suspicion. These include imaging processes such as x-rays, computed tomography (CT) or magnetic resonance tomography (magnetic resonance tomography, MRT). Measuring electrical muscle activity using electromyography (EMG) can also be informative. If there is a suspicion, hearing and eyesight are also tested.
Once it is clear what is causing the torticollis, the doctor can suggest appropriate treatment.
treatment
Unfortunately, many varieties of torticollis cannot be definitively cured. With the right treatment, however, the symptoms can be alleviated and everyday life can be made significantly easier.
A muscular torticollis must be treated as early as possible so that the misalignment does not persist permanently. For most children, conservative therapy already helps. This includes correct positioning while lying down (on the back) and physiotherapy with targeted stretching of the shortened muscles. If this does not improve, the doctor can operate. In about 90 percent of cases, the muscular torticollis can be successfully treated with it.
The muscle contractions in torticollis spasticus can be stopped with botoline toxin (Botox). In more severe cases, surgery is often carried out or what is known as deep brain stimulation is carried out. Certain areas of the brain are specifically stimulated electrically.
In the case of an infectious cause (torticollis infectiosus), the focus is on combating the infection. Antibiotics, for example, are used for bacterial infections.
Some forms of osseous torticollis can possibly be improved by surgical interventions, but usually not completely corrected.
Doctors treat acute torticollis by pulling the head mechanically and putting on a necktie.
If pain accompanies the torticollis, the doctor may prescribe a suitable pain reliever (such as ibuprofen or paracetamol).
When should you see a doctor?
Regardless of the underlying cause - you should always have a doctor clarify a torticollis. The medical professional can determine what type of torticollis is present and what the correct treatment is.
Torticollis: You can do that yourself
Warmth or over-the-counter pain relievers (such as ibuprofen, paracetamol) can help against possible tension pain. But: Behind a torticollis there can be a serious illness. Therefore, always have a doctor clarify the causes of a torticollis.
Tags: Menstruation eyes Diseases






.jpg)









-und-auflagen.jpg)