Inflammation of the fallopian tubes and ovaries
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Inflammation of the fallopian tubes (salpingitis) and inflammation of the ovaries (oophoritis) often occur together. In summary, doctors then speak of adnexitis. It is not uncommon: around one in eight sexually active women is affected. The triggers are usually bacteria such as chlamydia or gonococci. Read more about the causes of fallopian tube inflammation and ovarian inflammation as well as the symptoms, diagnosis and treatment here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. N70
Brief overview
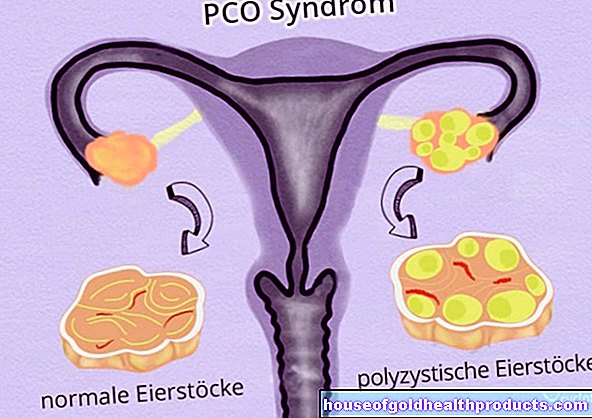
- Description: Unilateral or bilateral inflammation of the fallopian tubes (salpingitis) or ovaries (oophoritis). Salpingitis sometimes occurs on its own, while oophoritis almost only develops together with an inflammation of the fallopian tubes. The combination of salpingitis and oophoritis is called adnexitis.
- Causes & risk factors: mostly bacteria such as chlamydia or gonococci (pathogens causing gonorrhea), more rarely viruses (such as flu or mumps viruses). Risk factors are e.g. young age, frequently changing sexual partners, IUDs, smoking, vaginal douching.
- Symptoms: in the case of acute inflammation, usually sudden, severe abdominal pain, fever, severe feeling of illness, possibly foul smelling discharge, nausea and vomiting. With chronic inflammation, dull lower abdominal pain, back or pelvic floor pain, pain during sex, tiredness, possiblyConstipation, gas, irregular cycles.
- Complications & long-term effects: encapsulated accumulation of pus (abscess), impairment of fertility up to infertility, ectopic pregnancy, peritonitis, intestinal obstruction, blood poisoning (sepsis)
- Diagnostics: taking the medical history (anamnesis), gynecological examination, smear from the cervix, blood test, ultrasound, laparoscopy
- Treatment: mostly conservative with medication (antibiotics, anti-inflammatory pain relievers such as diclofenac) and physical measures (such as application of the cold). In certain cases, surgery.
Fallopian tube inflammation & ovarian inflammation: symptoms
An isolated fallopian tube inflammation or a combined fallopian tube and ovarian inflammation (adnexitis) can be acute or chronic (isolated ovarian inflammation is extremely rare).
Acute fallopian tube and ovarian inflammation
Symptoms do not occur with every inflammation of the fallopian tubes and ovaries, or at least none that are noticeable. For example, salpingitis caused by chlamydia often causes little discomfort.
Most of the time, however, acute fallopian tube inflammation or adnexitis causes the following symptoms:
- sudden severe abdominal pain (one or both sides)
- fever
- severe feeling of illness
- Nausea and vomiting
- bulging, tense, hard abdominal wall
- possibly yellowish-green, foul-smelling vaginal discharge (fluorine)
- you may have unusual vaginal bleeding
A hard, bloated, painful abdominal wall, nausea and vomiting, fever and severe acute abdominal pain together form the image of the "acute abdomen" (acute abdomen). This can occur in various abdominal diseases. In the case of adnexitis, the "acute abdomen" indicates that the inflammation has spread to neighboring organs such as the peritoneum (see below: complications). Then call the emergency doctor immediately!
Chronic fallopian tube and ovarian inflammation
If an acute inflammation is not treated (adequately) or leads to scarred tissue changes, chronic adnexitis or chronic fallopian tube inflammation often develops. Symptoms are then typically:
- chronic, dull, alternatingly severe pelvic pain (one or both sides), which may increase when sitting down or doing physical activity
- uncharacteristic back pain or pelvic floor pain
- frequent fatigue
- Tendency to be depressed
- sometimes: pain during sex
- less often: constipation, gas, pain or menstrual irregularities
Complications and long-term consequences
If adnexitis remains untreated for a long time, accumulations of pus (abscesses) can form. For example, a Douglas abscess can develop. This is an encapsulated pus in the so-called Douglas space (area between the back of the uterus and the rectum). Affected women often have severe pain when defecating.
In addition, acute adnexitis can lead to an abscess between the fallopian tube and ovary (tubo-ovarian abscess), as the tissue between the fallopian tube and ovary fuses in an inflammatory manner. As a result, extensive adhesions (brides) can form between the uterus, intestines, pelvic wall and ligaments. As a result, the fallopian tube can have problems collecting egg cells from the ovary and forwarding them to the uterus. The result is sterility.
However, fertility can also be impaired in another way - namely if a lot of inflammatory secretion forms in an acute fallopian tube inflammation or adnexitis, which clogs the fallopian tubes. Even after a single fallopian tube inflammation, 12 out of 100 women have problems conceiving a child. After the second salpingitis, the sterility rate is 25 percent, after the third even 50 percent. The risk of sterility is particularly high in chronic fallopian tube and ovarian inflammation.
Sometimes fallopian tube adhesions in the course of acute or chronic fallopian tube inflammation do not hinder fertilization, but the further transport of the egg cell to the uterus: The fertilized egg cell can get stuck to the adhesions and then implant directly in the fallopian tube - the result is an ectopic pregnancy (tubal pregnancy) .
The adhesions in the abdominal cavity (brides), which can form as a result of adnexitis (or other inflammation in the abdominal cavity), later cause a mechanical intestinal obstruction (ileus) in some women, more precisely a so-called briden ileus. This is an emergency that needs immediate surgery.
If the germ-containing, inflammatory secretion formed in adnexitis passes into the free abdominal cavity, dangerous peritonitis can develop. It is mostly limited to the small pelvis and is then called pelveoperitonitis. If the inflammation spreads to the entire peritoneum, one speaks of diffuse peritonitis. This emergency also calls for quick medical help!
The germs responsible for inflammation of the abdomen can spread throughout the body via the bloodstream and thus cause "blood poisoning" (sepsis). There may be danger to life! Call an emergency doctor immediately if you have signs of sepsis (such as fever, rapid pulse / heartbeat, accelerated breathing, pale or gray skin color, poor general condition).
Fallopian tube inflammation & ovarian inflammation: causes
Inflammation of the fallopian tubes and ovaries are mostly caused by bacteria. Most often, chlamydia or gonococci (pathogens of gonorrhea = gonorrhea) are responsible for the inflammation. Often the cause is also a mixed infection from different bacteria, including staphylococci, streptococci, E. coli (coli bacteria) and clostridia.
Viruses rarely cause fallopian tube inflammation / ovarian inflammation, for example flu viruses.
How can you get infected?
The triggering germs can reach the fallopian tubes and ovaries in different ways. According to this, doctors differentiate:
- Ascending (ascending) infection: The bacteria usually reach the fallopian tubes and ovaries via the vagina and uterus. This risk arises especially in the case of a bacterial vaginal infection (bacterial vaginosis) and / or if the cervix at the entrance to the uterus is slightly (during menstruation) or wide (during childbirth) open. Interventions via the vagina (e.g. inserting a coil, scraping) also encourage bacteria to rise.
- Descending infection: Doctors speak of a descending infection in adnexitis when the triggering germs from neighboring organs attack the fallopian tubes or ovaries - either through direct contact with the organs or via the lymphatic system. In this way, appendicitis, for example, can trigger inflammation of the fallopian tubes and ovaries.
- Haematogenic infection: The pathogens of various infectious diseases can reach the fallopian tubes and ovaries via the blood and cause inflammatory processes there. Such a hematogenous adnexitis is observed particularly often in tuberculosis (pathogen: tubercle bacteria). Sometimes, however, other infectious diseases (such as flu, mumps, scarlet fever) also trigger inflammation of the fallopian tubes / ovaries in the bloodstream.
Risk factors
Various factors favor an inflammation of the fallopian tubes / ovaries. These include:
- Young age: Adnexitis mainly affects girls or women between the ages of 15 and 25 - i.e. in the first years of their sexual activity.
- Frequently changing sexual partners: The higher the number of sexual partners, the greater the risk of contracting a sexually transmitted disease (chlamydial infection, gonorrhea, etc.). The pathogens of these diseases can rise in the genital tract and cause salpingitis or oophoritis (adnexitis).
- IUD: Women who use the IUD are more prone to developing fallopian tubes or ovaries. Especially in the first few months after inserting the IUD, bacteria can easily rise from the vagina to the fallopian tubes / ovaries and trigger inflammation.
- Smoking: nicotine consumption changes the composition of the uterine mucus. As a result, it can no longer function as well as a barrier against rising germs.
- Vaginal douching: It can easily happen that bacteria from the external genital area are washed deep into the vagina. From there, the ascent via the uterus to the fallopian tubes and ovaries is no longer that far.
- Interventions in the abdomen: There is an increased risk of adnexitis after scraping (curettage) or an abortion by surgery, for example. With such interventions there is a risk of germs getting into the vagina and uterus. From there they can ascend to the fallopian tubes and even ovaries.
- Previous fallopian tube inflammation: Anyone who has ever had salpingitis is more prone to re-inflammation of the fallopian tubes.
Pelvic inflammatory disease (PID)
Inflammation of various organs and structures in the female abdomen often occurs in combination. In this complex inflammatory process, the individual inflammations can usually hardly be distinguished from one another. In the English-speaking world, all these inflammations in the upper genital tract and their complications are therefore summarized under the term "pelvic inflammatory disease" (PID). Above all, these include:
- Adnexitis (inflammation of the fallopian tubes plus inflammation of the ovaries)
- Inflammation of the cervix (cervicitis)
- Inflammation of the lining of the womb (endometritis)
- Inflammation of the connective tissue structures in the pelvic area (parametritis)
- Inflammation of the peritoneum confined to the pelvis (pelveoperitonitis)
- Abscess between fallopian tubes and ovary (tubo-ovarian abscess)
Fallopian tube inflammation & ovarian inflammation: therapy
Inflammation of the fallopian tubes and ovaries are primarily treated conservatively: medication and physical treatment measures such as the application of cold are available. Physical rest or bed rest in the acute phase are also advisable. In addition, the patient should ensure that they are drinking enough fluids (unless this has to be restricted for medical reasons, such as cardiac insufficiency).
Surgery is only necessary in certain cases for adnexitis (such as complications such as peritonitis).
In the event of an operation, hospitalization is definitely necessary. Many women are also hospitalized for the conservative treatment of fallopian tube and ovarian inflammation.
Medication
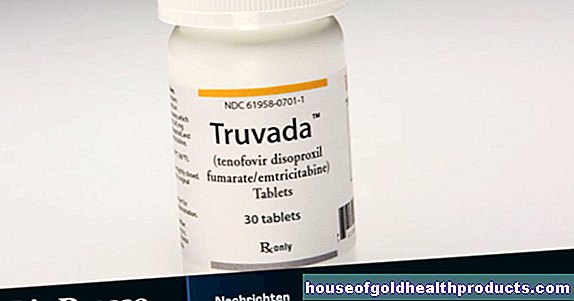
Acute fallopian tube inflammation and ovarian inflammation are treated with antibiotics (since bacteria are almost always the trigger): Usually the doctor prescribes one or more antibiotics immediately after the diagnosis, which are generally effective against the most common adnexitis pathogens (broad spectrum antibiotics). As soon as the exact type of pathogen has been identified in the patient's genital swab, the antibiotic therapy can be adjusted. This means that the doctor can switch the treatment to one or more antibiotics that target the pathogen in question.
The antibiotics are often given as an infusion for acute fallopian tube and ovarian inflammation, but sometimes also in tablet form. The drugs are given for at least ten days. If a certain infection such as gonorrhea is the cause of salpingitis or adnexitis, the partner must also be treated.
Antibiotics fight the cause of the inflammation (bacterial infection). In addition, medication can be given to alleviate the symptoms. This can be achieved with anti-inflammatory and pain-relieving drugs from the group of NSAIDs (non-steroidal anti-inflammatory drugs) such as diclofenac.
"Cortisone" (a colloquial term for corticosteroids such as prednisolone) also has a strong anti-inflammatory effect. Its use in adnexitis is controversial.
For chronic adnexitis, antibiotic therapy is carried out when acute signs of inflammation are present.
Physical therapy
For acute fallopian tube inflammation and ovarian inflammation, cold treatment is recommended: An ice pack is placed on the lower abdomen. This will relieve the pain and prevent the inflammation from spreading (by stopping the increase in blood flow caused by the inflammation).
As soon as the acute phase of the illness has subsided, heat treatment makes more sense: Warm, moist compresses on the lower abdomen now stimulate blood circulation. This can support the breakdown of inflamed tissue and prevent scarring. Other methods of heat treatment also serve this purpose, for example warm hip baths, mud packs or high-frequency heat radiation (short-wave diathermy).
The switch from cold to heat treatment must not take place too early, otherwise there is a risk of relapse. Therefore, the doctor uses the body temperature and the rate of sedimentation to check whether the acute inflammatory processes have subsided or not.
Warmth applications are also recommended for chronic adnexitis: With warm, moist compresses, mud packs or heat radiation, the blood circulation around the lower abdomen can be increased. This can relieve the persistent pain and loosen adhesions. A spa stay (with mud packs, mud baths, etc.) may also be useful.
surgery
In acute adnexitis, an operation is necessary if another inflammation in the abdomen has spread to the fallopian tubes and ovaries via a descending infection (such as appendicitis). On the other hand, surgery is performed if the acute adnexitis has caused complications that cannot be treated conservatively. Two examples:
If the entire peritoneum is also inflamed, the abdominal cavity must be opened (laparotomy) and rinsed.
If a tubo-ovarian abscess has formed, the acute inflammation is first treated with medication (antibiotics, anti-inflammatory drugs). This is followed by an operation: If the patient still has a desire to have children, one tries, if possible, to surgically loosen the adhesions (adhesiolysis) and to make the fallopian tubes open again (tube recanalization). This is usually done as part of a laparoscopy.
If, on the other hand, family planning has already been completed or the conservative measures are not working, the doctor can recommend a major intervention to the patient - surgical cleansing of the inflammation area (focal treatment) and the complete removal of the organs involved. This means that the Chrirug cuts out the affected fallopian tube or fallopian tubes. Other organs may have to be removed (ovaries, uterus).
This radical intervention is more often considered in women with chronic adnexitis when conservative treatment is unsuccessful. The removal of the fallopian tubes and possibly also the ovaries and uterus (hysterectomy) is then often the only way to completely eliminate the chronic inflammation and get rid of the pain that has often lasted for years.
Tip: Before a patient decides to remove the fallopian tubes and possibly ovaries and uterus, the doctor should explain in detail the benefits and risks of the procedure. The consequences must also be considered. If, for example, both fallopian tubes and ovaries are removed, the woman must then permanently take sex hormones (estrogens and progestins).
Fallopian tube inflammation & ovarian inflammation: investigations
The gynecologist is the right contact for suspected adnexitis. He will first talk to the patient in detail in order to collect her medical history (anamnesis). Possible questions in this conversation are, for example:
- Which complaints do you have exactly?
- How long have the complaints existed?
- Have you ever had an inflammation in your abdomen?
- Do you have changing sexual partners?
- Do you use the IUD to prevent contraception? If so, when was it used?
This is followed by a gynecological examination. Typical of adnexitis is the so-called portio-sliding pain: if the gynecologist moves the cervix a little back and forth while palpating the internal genital organs, pain occurs. In addition, inflamed fallopian tubes and ovaries are usually swollen and tender.
An unusual discharge from the vagina and the cervix is also typical of acute adnexitis - the latter is also usually inflamed if the fallopian tubes are inflamed (cervicitis). The doctor therefore takes a smear from the vagina or the cervix to have it examined for bacteria. The exact identification of the germs then helps in planning the antibiotic therapy.
The gynecologist also takes a blood sample from the patient. When there is inflammation in the body, certain blood values are generally increased, such as the rate of sedimentation and the number of white blood cells (leukocytes).
The ultrasound can show the doctor signs of advanced adnexitis. These include thickened fallopian tubes and a build-up of fluid inside the fallopian tubes. An abscess will also be visible on the ultrasound image. The examination is usually carried out through the vagina (transvaginal endosonography).This method gives better images of the inside of the abdomen than the conventional ultrasound examination of the abdominal wall.
Fallopian tubes & Co. can be assessed even more precisely using a laparoscopy. This is mainly done in unclear cases. The doctor inserts an endoscope into the abdominal cavity through small incisions in the abdomen. This is a thin, tubular instrument with a small camera and a light source on the tip (laparoscope). This allows the doctor to examine the internal genital organs directly and, if necessary, take a smear (e.g. from the fallopian tubes).
In addition to diagnosing adnexitis, laparoscopy can sometimes help treat it. In this way, fine medical instruments can also be introduced via the small abdominal incisions, with which, for example, adhesions can be surgically loosened and the fallopian tubes reopened.
Differential diagnoses
Different diseases can cause symptoms similar to adnexitis. In the course of the examinations, the doctor must therefore rule out these differential diagnoses. These include ectopic pregnancy, endometriosis, appendicitis, urinary tract infection and an ovarian cyst twisted around its stem.
Fallopian tube inflammation & ovarian inflammation: course & prognosis
Acute fallopian tube inflammation and ovarian inflammation should be treated as early and consistently as possible. Then the chances of recovery are good and the acute inflammation usually heals within one to two weeks. In most cases, conservative measures such as medication and physical therapy are sufficient. With severe inflammation and adhesions, the woman's fertility is often impaired.
Chronic adnexitis is difficult to treat. Conservative therapeutic measures can in many cases alleviate the symptoms and sometimes even eliminate the chronic inflammation itself. Nevertheless, many women continue to have problems getting pregnant or are prone to ectopic pregnancies (due to permanent adhesions in the fallopian tube). In some cases, there is also complete infertility as a result of chronic inflammation in the abdomen.
In severe cases, conservative treatment remains unsuccessful. Then the chronic fallopian tube inflammation and ovarian inflammation can only be brought under control by completely removing the fallopian tubes and possibly also the ovaries and uterus.
Fallopian tube inflammation & ovarian inflammation: prevention
Acute adnexitis can be prevented if you always use a condom during sexual intercourse. In addition to pregnancy, the mechanical contraceptive can also prevent infection with pathogens that can cause pelvic inflammation (such as chlamydia).
You should also ensure proper intimate hygiene. The motto here is: neither too little hygiene nor too much! Wash your private parts regularly. Clear water is sufficient for this. You can also use pH-neutral, gentle washing lotions for intimate hygiene. But don't use aggressive soap! It can unbalance the natural vaginal flora and thus promote the spread of pathogens. If these rise above the vagina and uterus, there is a risk of adnexitis. Caution is also advised with vaginal douching. They can also lead to inflammation of the fallopian tubes and ovaries.
Tags: desire to have children anatomy pregnancy birth













.jpg)