WPW syndrome
Florian Tiefenböck studied human medicine at the LMU Munich. In March 2014, he joined as a student and has supported the editorial team with medical articles ever since. After receiving his medical license and practical work in internal medicine at the University Hospital Augsburg, he has been a permanent member of the team since December 2019 and, among other things, ensures the medical quality of the tools.
More posts by Florian Tiefenböck All content is checked by medical journalists.In WPW syndrome (Wolff-Parkinson-White syndrome), one or more additional conduction pathways incorrectly excite the heart. As a result, it strikes too quickly in a seizure manner. This form of cardiac arrhythmia can be treated by sclerotherapy of the superfluous conduction pathways. Learn all about the symptoms and treatment options for WPW syndrome.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. R00I48I46I47I49I45I44

WPW syndrome: description
WPW syndrome is a heart rhythm disorder. The name comes from the American cardiologist L. Wolff, P.D. White and J. Parkinson back (Wolf-Parkinson-White). In 1930 they described the signs of WPW syndrome in young patients. These include attacks of sudden palpitations (tachycardia) and changes in what is known as the electrocardiogram, which records the electrical activity of the heart.
The heartbeat has a clock, the so-called sinus node. It sits in the right atrium of the heart and dictates how fast the heart beats. To do this, it sends electrical signals to what is known as the atrioventricular node (AV node), which is located between the atria and the ventricles. Many electrical excitations are filtered out at this point. About sixty to eighty excitations reach the AV node per minute. The AV node forwards the excitations to the left and right ventricles via two conduction pathways.
Additional excitation conduction
In the WPW syndrome, those affected have an additional (accessory) pathway between the atrium and ventricle. The conduction pathway can lead from the atrium into the ventricle or vice versa. The excitations from the sinus node, but also excitations from the ventricles, meet this additional conduction path. In contrast to the AV node, the excitations are not filtered and all electrical signals are passed on to the muscle cells of the heart chambers.
Since the additional conduction path can also lead in the "wrong" direction, the electrical signals from the muscle cells in the heart chambers run back into the atrium. A so-called circular excitation arises, which makes the heart beat very quickly but in a steady rhythm.
The additional pathway of the WPW syndrome is innate. Symptoms such as palpitations usually occur in adolescence. WPW syndrome is more common in men than women.
WPW syndrome: symptoms
WPW syndrome does not always cause symptoms. Sometimes the extra pathway is only discovered by the changes in the electrocardiogram.
One of the most common symptoms is a sudden rapid heartbeat (tachycardia). The heart beats between 150 and 240 times per minute. 60 to 80 beats per minute are normal when sitting quietly. The pulse is very regular in WPW tachycardia.
Some patients experience the racing heart as an intensified heartbeat. In medicine one speaks of "palpitations". Other sufferers feel a "heart stumbling". These discomforts usually disappear just as abruptly as they came. In addition, those affected may suffer from dizziness, chest pain and shortness of breath. After a racing heart, they are often tired and have a strong need to urinate.
Fear and fainting
The racing heart causes fear in many patients. Dizziness and shortness of breath can make this feeling worse. Due to the high heart rate, the heart can sometimes no longer pump enough blood to the organs of the body. As a result, some patients lose consciousness.
WPW syndrome in newborns
Symptoms of WPW syndrome very rarely occur in babies. Babies are noticeably pale and breathe quickly during tachycardia. They may refuse to eat or drink, be easily irritable, or cry a lot. In some cases they get a fever. Due to the immature structure of the heart, WPW syndrome can be more dangerous for children than for adults.
WPW syndrome: causes and risk factors
The cause of WPW syndrome is unknown. It is assumed, however, that the additional conduction path originated from a defect in the embryonic development of the heart. Researchers also found that WPW syndrome occurs with other congenital heart defects. These include defects in the dividing walls between the right and left sides of the heart (ventricular septal defects).
A WPW syndrome is also often found in the rare Ebstein anomaly, in which the heart valve between the right atrium and the right ventricle is malformed. Since certain genetic changes have been linked to WPW syndrome, the predisposition for WPW syndrome is very likely hereditary.
WPW Syndrome: Investigations and Diagnosis
When diagnosing WPW syndrome, the additional pathway must be proven.
First, the doctor will ask a few questions about the symptoms:
- Do you have a racing heart that starts suddenly and ends abruptly?
- How often do you have these seizures?
- How long do they last?
- Can you still feel and count your pulse?
- Do you feel like your heart is "tripping"?
- Do you get dizzy?
- Have you ever lost consciousness?
- Can you stop the seizures by holding your breath, pressing your stomach, or drinking cold water?
- Do you have a known heart defect?
- Has WPW syndrome already occurred in your family?
This is followed by a physical examination. If the patient has a palpitations, an electrocardiogram can be written first so that he can be treated as quickly as possible.
electrocardiogram
An important examination for suspicion of WPW syndrome is the electrocardiogram (EKG). A writer records the electrical activity of the heart. In some cases, the doctor will diagnose WPW syndrome. EKG and long-term EKG are only preliminary examinations for the actual electrophysiological examination. After the EKG, the doctor can administer a drug that stops the heart racing.
Long-term ECG
Sometimes a long-term ECG must also be performed. The EKG machine is connected to electrodes that are attached to the chest. It records the heartbeat for 24 hours. Sometimes tachycardia is detected.
If this is not possible, a so-called event recorder can also be used. It is smaller than a long-term ECG device and is worn over a longer period of time. When patients experience a racing heart, they must press a button on the recorder that records the heart's action. There are also recorders (LOOP recorders) that are implanted under the skin in the left breast area. The advantage is that the patient does not have to pay attention to his heartbeat and does not have to noticeably carry a device with him.
Exercise ECG
Sometimes an exercise ECG is also done. To do this, the patient has to exercise himself physically on an exercise bike while he is connected to an EKG recorder. Exercise can in some cases trigger tachycardia.
Electrophysiological examination
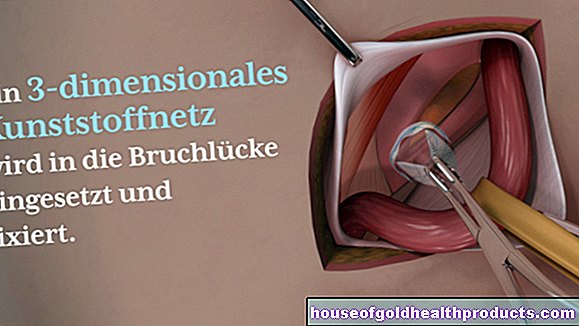
In order to reliably diagnose the WPW syndrome, a so-called electrophysiological examination (EPU) must be carried out. This is a special type of cardiac catheter examination. Two thin wires (catheters) are inserted into the patient's large vena cava via the inguinal veins, and these are advanced to the heart. There the catheters measure electrical signals at various points on the heart muscle wall. The syndrome can be treated at the same time during the examination.
WPW syndrome: treatment
The only, but very effective, way to cure WPW syndrome patients is through ablation. Medication only provides temporary relief from symptoms. In addition, there are certain maneuvers that can slow the heartbeat in tachycardia.When the person takes a deep breath, holds it, and presses against it, the heartbeat often drops. You can also massage the carotid artery, drink ice-cold water or put a bag of ice on your face. The heartbeat is throttled in a reflective manner.
EPU and ablation
The EPU has the greatest importance in the treatment of WPW syndrome. At the EPU it is possible to look for the additional conduction path and to obliterate it directly (catheter ablation). In this way, the faulty conduction in the heart is permanently interrupted. Ablation can cure WPW syndrome almost 99 percent of the time. People of certain professional groups such as pilots or train drivers with a diagnosed WPW syndrome are only allowed to continue their profession if they have successfully undergone an ablation.
Medication
Certain medications can stop the racing heart in WPW syndrome. They are usually injected into the vein. Examples are adenosine or ajmaline. There are also drugs that are taken permanently to prevent the heart racing. An example of this are ß-blockers. The only treatment that can cure those affected by WPW syndrome is ablation.
Electrocardioversion
Sometimes a so-called electrocardioversion is necessary with tachycardia. The patient's heart is stimulated with electricity via two electrodes (“paddles”) on the chest, as in resuscitation. The patient is briefly anesthetized for this purpose. The heart sometimes falls into its normal rhythm as a result of the electrical surge.
WPW syndrome: disease course and prognosis
WPW syndrome is very rarely dangerous. The racing heart is often very uncomfortable. Since it can sometimes last for hours, those affected are exhausted after a tachycardia.
Some people suffer from cardiac arrhythmias because they have a special job, such as competitive sports. However, ablation is a very effective therapy that can cure sufferers in most cases.
In people with frequent palpitations, however, there is a risk of a malignant arrhythmia being triggered. A sustained electrical excitation occurs in the atrium, a so-called atrial fibrillation. The additional conduction path transmits the impulses unfiltered to the chambers. Ventricular fibrillation can occur. Men between the ages of 30 and 50 are particularly at risk of developing such a cardiac arrhythmia.
Affected people can influence their heart rate themselves by performing the mentioned maneuvers. Sometimes influences that often trigger tachycardia should be avoided. These include alcohol or intense exercise.
Since the WPW syndrome most likely also has a hereditary component, family members should also be informed about the disease and examined if necessary. If the WPW syndrome is diagnosed at an early stage, complications can be avoided.
Tags: unfulfilled wish to have children book tip alcohol