Lung cancer
and Martina Feichter, medical editor and biologist Updated onMarian Grosser studied human medicine in Munich. In addition, the doctor, who was interested in many things, dared to make some exciting detours: studying philosophy and art history, working on the radio and, finally, also for a Netdoctor.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Lung cancer (bronchial carcinoma) is one of the most common cancers in Europe. The main risk factor is smoking. Passive smoking can also lead to lung cancer. The malignant tumor can be treated in a number of ways, including chemotherapy and surgery. Nevertheless, lung cancer is rarely curable. Read everything you need to know about lung cancer here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. C34
Lung Cancer: Quick Reference
- Symptoms: Initially often no symptoms or only unspecific symptoms (such as persistent cough, chest pain, fatigue). Later, for example, shortness of breath, slight fever, severe weight loss, bloody sputum.
- Main types of lung cancer: The most common is non-small cell lung cancer (with subgroups). Small cell lung cancer is less common, but more aggressive.
- Causes: Mostly smoking. Other risk factors include asbestos, arsenic compounds, radon, high levels of air pollution and a diet low in vitamins.
- Examinations: X-rays, computed tomography (CT), magnetic resonance tomography (MRT), examination of tissue samples (biopsies), positron emission tomography (mostly in combination with CT), blood tests, examination of the sputum, removal and examination of the "lung water" (pleural puncture)
- Therapy: surgery, radiation therapy, chemotherapy, possibly other methods.
- Prognosis: Lung cancer is usually diagnosed late and is therefore rarely curable.
Lung cancer: signs (symptoms)
Lung cancer (lung carcinoma) often causes no symptoms or only unspecific symptoms at first. These include fatigue, coughing, or chest pain. Such complaints can also have many other causes, such as a cold or bronchitis. Therefore, lung cancer is often not detected in its early stages. This then complicates the therapy.
More pronounced signs cause lung cancer in the advanced stage. Then, for example, rapid weight loss, bloody sputum and shortness of breath can occur.
If the lung cancer has already formed daughter settlements (metastases) in other parts of the body, there are usually additional symptoms. For example, metastases in the brain can damage nerves. The possible consequences are headaches, nausea, impaired vision and balance, or even paralysis. If the cancer cells have attacked the bones, osteoarthritis-like pain can occur.
Read more about the different signs of lung cancer in the article Lung Cancer: Symptoms.
Lung cancer: stages
Lung cancer, like any cancer, occurs when cells degenerate. In this case they are cells of the lung tissue. The degenerated cells multiply in an uncontrolled manner and displace healthy tissue in their environment. Later, individual cancer cells can spread through the blood and lymph vessels in the body. Often they then form a daughter tumor (metastasis) elsewhere.
Lung cancer can therefore have progressed to different degrees. For example, one speaks of an early stage or - in the worst case - of the end-stage lung cancer. But these are not exactly defined terms. Doctors therefore mostly use the so-called TNM classification: It allows the individual stages of lung cancer to be described precisely. This is important because a patient's treatment and life expectancy depend on the stage of lung cancer.
Lung Cancer: TNM Classification
The TNM scheme is an international system for describing the spread of a tumor. It says:
- "T" for the size of the tumor
- "N" for lymph node infestation (Nodi lymphatici)
- "M" for the presence of metastases
A numerical value is assigned for each of these three categories. It shows how advanced a patient's cancer is.
The exact TNM classification in lung cancer is complex. The following table is intended to give a rough overview:
|
TNM |
Tumor character at diagnosis |
Remarks |
|
Tis |
Carcinoma in situ ("tumor in place") |
Early cancer form: the tumor is still limited to its origin, i.e. it has not yet grown into the surrounding tissue. |
|
T1 |
The maximum diameter of the tumor is 3 cm, surrounded by lung tissue or pulmonary membrane, and the main bronchus is not affected. |
The main bronchi are the first branches of the windpipe in the lungs. T1 can be specified even more precisely and is therefore subdivided into:
|
|
T2
|
The largest diameter of the tumor is more than 3 and max. 5 cm OR the main bronchus is affected OR the lung membrane is affected OR the tumor has partially collapsed (atelectasis) or partially or completely inflamed |
Further breakdown into:
|
|
T3 |
The largest diameter of the tumor is at least 5 cm and max. 7 cm OR the inner chest wall (including the pulmonary membrane), the phrenic nerve or the pericardium is affected OR there is an additional tumor nodule in the same lung lobe as the primary tumor | |
|
T4 |
The largest diameter of the tumor is> 7 cm OR other organs are affected (e.g. diaphragm, heart, blood vessels, trachea, esophagus, vertebral body) OR there is an additional tumor nodule in another lobe of the lung | |
|
N0 |
no lymph node involvement | |
|
N1 |
Involvement of lymph nodes on the same (body) side as the tumor (ipsilateral), of lymph nodes around the bronchi (peribronchial) and / or of lymph nodes on the root of the lung on the same side |
Lung root = entry point of the pulmonary vessels and main bronchi into the lungs |
|
N2 |
Involvement of lymph nodes in the mediastinum and / or at the exit of the two main bronchi on the same side |
Mediastinum = space between the two lungs |
|
N3 |
Involvement of lymph nodes in the mediastinum or at the exit of the two main bronchi on the opposite side (contralateral), involvement of lymph nodes on the neck or above the collarbone on the same side or the opposite side | |
|
M0 |
No distant metastasis (s) | |
|
M1 |
Distant metastasis (s) present |
Depending on the degree of metastasis, further breakdown into 3 (non-small-cell lung cancer) or 2 (small-cell lung cancer) categories: M1a, M1b, (M1c) |
After T and N there can be an "X" instead of a number (TX, NX). This means that the respective aspect (T = tumor size, N = lymph node involvement) cannot be assessed.
The different stages of lung cancer
As mentioned above, the TNM classification determines the stage of lung cancer. A distinction is made between the following stages, whereby the following applies: The higher the stage, the more advanced the disease:
Lung cancer stage 0
This stage corresponds to the classification Tis N0 Mo. This means: There is an early form of cancer that is still limited to its original tissue (carcinoma in situ). Lymph nodes are not involved and there are no distant metastases either.
Stage I lung cancer
This stage is divided into A and B:
Stage IA corresponds to a classification of T1 N0 M0. This means that the malignant lung tumor has a maximum diameter of three centimeters, is surrounded by lung tissue or pulmonary membrane, and the main bronchus is not affected. There are also no lymph node involvement and no distant metastases.
Depending on the more precise classification of the tumor size - such as T1a (mi) or T1c - stage IA is further subdivided into IA1, IA2 and IA3.
In stage IB, the tumor has a classification of T2a N0 M0: it is more than three to a maximum of four centimeters in diameter, has neither affected lymph nodes nor spread to other organs or tissue.
In stage I, lung cancer has the best prognosis and is often still curable.
Stage II lung cancer
Here, too, a distinction is made between A and B:
Stage IIA includes lung tumors of the classification T2b N0 M0: The tumor is more than four and a maximum of five centimeters in diameter. No lymph nodes are involved and no distant metastases can be detected.
Stage IIB includes tumors of size classification T1 (a to c) with lymph node involvement of type N1, but no distant metastases (M0).
Tumors of the size classification T2 (a or b) with lymph node involvement of type N1 and without distant metastases (M0) are also assigned to this tumor stage.
The same applies to larger tumors of classification T3 if no lymph nodes have yet been affected (N0) and no distant metastases have formed (M0).
Even in stage II, lung cancer is still curable in some cases. The treatment is a bit more complex and the statistical life expectancy of the patient is already lower than in stage I.
Lung cancer stage III
Stage III is further subdivided into A, B and C:
In stage IIIA tumors have the following classifications:
- T1 a to c N2 M0
- T2 a or b N2 M0
- T3 N1 M0
- T4 N0 M0
- T4 N1 M0
Stage IIIB includes the following tumor classifications:
- T1 a to c N3 M0
- T2 a or b N3 M0
- T3 N2 M0
- T4 N2 M0
Stage IIIC includes tumors of the following classification:
- T3 N3 M0
- T4 N3 M0
Put simply, tumors of any size belong to stage III lung cancer as soon as lymph nodes are affected (to varying degrees) but no distant metastases have yet formed. With regard to lymph node involvement, there is one exception: very large tumors are assigned to this stage even without lymph node involvement (T4 N0 M0) - more precisely to stage IIIA.
In stage III, lung cancer is so advanced that patients can only be cured in rare cases.
Stage IV lung cancer
Life expectancy and chances of recovery are very low at this stage, because the disease is already very advanced: the tumor has already metastasized (M1). Tumor size and lymph node involvement then no longer play a role - they can vary (every T, every N). Depending on the extent of the metastasis (M1 a to c), a distinction is made between stages IVA and IVB.
In any case, only palliative therapy is possible for stage IV lung cancer - treatment with the aim of alleviating the symptoms and extending survival time.
The four stages of lung cancer
Small cell lung cancer: alternative classification
Doctors differentiate between two large groups of lung cancer: small-cell lung cancer and non-small-cell lung cancer (see below). Both can be divided into stages according to the above-mentioned TNM classification and treated on the basis of this classification.
However, the TNM system shown above was primarily developed for the (much more common) non-small cell lung cancer. For small cell lung cancer, however, there are hardly any studies on tumor treatment based on the TNM system.
Instead, most of the available studies examined treatment strategies that were based on a different classification of small cell lung cancer:
- "very limited disease": This category corresponds to the TNM classifications T1 / 2 with N0 / 1 and M0. Only about five percent of patients have this early stage of the disease at the time of diagnosis.
- "limited disease": Corresponds to T3 / 4 with N0 / 1 and M0 or T1 to T4 with N2 / N3 and M0. About 25 to 35 percent of all small cell lung cancer cases are detected at this stage.
- "Extensive disease": This includes all small cell lung carcinomas that have already formed distant metastases (M1) - regardless of the tumor size (each T) and the lymph node involvement (each N). In the vast majority of patients (60 to 70 percent), the tumor is already in this advanced stage at the time of diagnosis.
Lung cancer: treatment
The treatment of lung cancer is very complicated. It is individually adapted to each patient: Above all, it depends on the type and spread of lung cancer. The age and general state of health of the patient also play an important role in therapy planning.
If a treatment aims to cure lung cancer, it is called curative therapy. Patients who can no longer cure receive palliative therapy. It should extend the life of the patient as much as possible and alleviate his symptoms.
Doctors from different specialties in a hospital advise each other on the final treatment strategy. These include, for example, radiologists, surgeons, internists, radiation specialists and pathologists. In regular meetings ("tumor boards") they try to find the best lung cancer therapy for a patient.
There are essentially three therapeutic approaches that can be used individually or in combination:
- Surgery to remove the tumor
- Chemotherapy with special drugs against rapidly growing cells (such as cancer cells)
- Radiation of the tumor (radiation therapy)
There are also some new therapeutic approaches, for example with targeted drugs that attack cancer cells directly. Such new procedures are only possible for certain patients.
Lung cancer: surgery
Lung cancer usually only has a real chance of cure as long as it can be operated on.The surgeon tries to completely remove the cancerous lung tissue. He also cuts a border out of healthy tissue. In this way he wants to make sure that no cancer cells are left behind. Depending on the extent of the bronchial carcinoma, either one or two lung lobes (lobectomy, bilobectomy) or even an entire lung (pneumonectomy) are removed.
In some cases it would be useful to remove an entire lung. However, the poor state of health of the patient does not allow this. Then the surgeon removes as much as necessary, but as little as possible.
During the operation, the surrounding lymph nodes are also cut out (mediastinal lymph node dissection). You can do this even if the preliminary examinations did not reveal any evidence of cancer of the lymph nodes. Often these are the first station for resettlement, which cannot be recognized at the beginning.
Unfortunately, in many patients there is no longer any prospect of surgery to cure lung cancer: the tumor is too advanced at the time of diagnosis. In other patients, the tumor would in principle be operable. However, the patient's lung function is so poor that he would not be able to cope with removing parts of the lungs. Doctors therefore conduct special examinations in advance to determine whether an operation would make sense on a patient.
Lung cancer: chemotherapy
Lung cancer, like many other types of cancer, can also be treated with chemotherapy. The patient receives drugs that inhibit the division of rapidly growing cells - such as cancer cells. This can inhibit tumor growth. These active ingredients are called chemotherapy drugs or cytostatics.
Chemotherapy alone is not enough to cure lung cancer. They are therefore mostly used in combination with other treatments. For example, it can be done in advance of an operation to shrink the tumor (neoadjuvant chemotherapy). Then the surgeon has to cut out less tissue afterwards.
In other cases, chemotherapy is carried out after the operation: It is intended to destroy any cancer cells that may still be in the body (adjuvant chemotherapy).
Chemotherapy for lung cancer usually consists of several treatment courses. So there are certain days when the doctor gives the patient the cytostatics. In between, there are two to three week breaks in treatment. The patient usually receives the active ingredients as an infusion through a vein. Sometimes the preparations are also given in tablet form (orally).
To check the effect of chemotherapy, the patient is regularly examined using computed tomography (CT). In this way, the doctor can see whether he may need to adjust the chemotherapy. He can, for example, increase the dose of active ingredient or prescribe another cytostatic agent.
Lung cancer: radiation
Another approach to lung cancer treatment is radiation. Lung cancer patients usually receive radiation therapy in addition to another form of treatment. Similar to chemotherapy, radiation can take place before or after an operation, for example. They are often used in addition to chemotherapy. This is called chemoradiotherapy.
Some lung cancer patients also receive what is known as prophylactic skull radiation. That means: The skull is irradiated as a precaution to prevent brain metastases from developing.
New therapeutic approaches for lung cancer
For several years now, scientists have been researching new methods of (lung) cancer therapy:
In targeted therapies, drugs are administered that attack cancer cells directly (in contrast to this, cytostatics = chemotherapeutic agents generally work against rapidly growing cells, which include, for example, hair root cells in addition to cancer cells). The targeted drugs disrupt mechanisms that control cancer cell growth, for example. However, they only work if the cancer cells have suitable points of attack for the respective drug - and this is not the case with every lung cancer tumor.
Another new development is immunotherapies. This is where drugs are administered that help the immune system fight cancer more effectively. As with the targeted therapies, this does not work for all patients. You can read more on the subject in the article Immunotherapy in cancer.
Some of these new therapies are already approved for the treatment of advanced non-small cell lung cancer. In the case of small cell lung cancer, there has so far only been one approval for one immunotherapeutic drug. Further new therapeutic approaches are still being tested in studies.
Other treatment measures
The therapies mentioned are aimed directly at the primary tumor and possible lung cancer metastases. In the course of the disease, however, various complaints and complications can arise that must also be treated:
- Fluid between the pleura and pleura (pleural effusion): It is sucked off through a cannula (pleural puncture). If the effusion continues, you can insert a small tube between the pleura and the pleura, through which the fluid flows off. It stays longer in the body (thoracic drainage).
- Bleeding in the bronchi: Such tumor-related bleeding can be stopped, for example, by specifically closing the blood vessel in question, for example as part of a bronchoscopy.
- Closure of blood vessels or airways by the tumor: If the tumor closes blood vessels or airways, they can be made open again by inserting a stent (stabilizing tube). Or you can remove the tumor tissue from the affected area, for example with a laser.
- Tumor pain: Advanced lung cancer can cause severe pain. The patient then receives appropriate pain therapy, for example painkillers in the form of a tablet or injection. In the case of painful bone metastases, radiation can provide relief.
- Shortness of breath: It can be relieved with medication and the administration of oxygen. Special breathing techniques and the correct positioning of the patient are also helpful.
- severe weight loss: Affected patients may have to be fed artificially.
- Side effects of chemotherapy such as nausea and anemia: They can be treated with suitable medication.
In addition to treating the physical complaints, it is also very important that the patient is well cared for mentally. Psychologists, social services and self-help groups help with disease coping. This increases the patient's quality of life. The relatives can and should be included in the therapy concepts.
-
Lung cancer: "Focus fully on the treatment"
Three questions for
Priv.-Doz. Dr. med. Benedikt Gahn,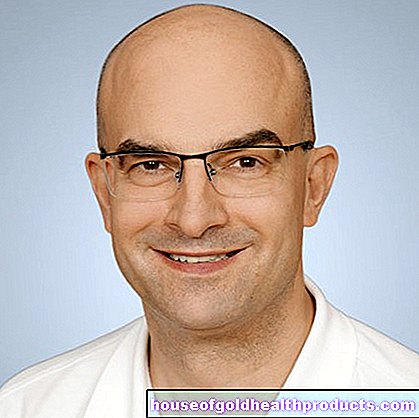
Specialist in internal medicine, hematology, oncology -
1
Why is lung cancer often diagnosed so late?
Priv.-Doz. Dr. med. Benedikt Gahn
In the early stages, lung cancer is often asymptomatic or unspecific. For example, you may experience a persistent cough or feel exhausted. Complications such as pneumonia can occur later - but then lung cancer is usually already in an advanced stage.
-
2
How can I support the treatment of lung cancer?
Priv.-Doz. Dr. med. Benedikt Gahn
Lung cancer is an aggressive disease that very often leads to death. This process can only be stopped if you, the patient, put diagnostics and therapy first. This means: Avoid delays, for example due to weekend activities, vacations or stays in rehabilitation clinics. This can have fatal consequences. Concentrate fully on your treatment.
-
3
Do you have a special tip for those affected?
Priv.-Doz. Dr. med. Benedikt Gahn
Lung cancer therapy has made significant progress in recent years. Modern, molecular methods enable "targeted therapies" - that is, a targeted cancer therapy that is directed only against the cancer cells and is therefore more tolerable and effective. Find a practice or clinic that uses these modern methods in diagnostics and therapy.
-
Priv.-Doz. Dr. med. Benedikt Gahn,
Specialist in internal medicine, hematology, oncologyDr. Gahn is the chief physician of oncology at the Paracelsus Clinic Henstedt-Ulzberg, specializing in hematology and internal oncology.
Small cell lung cancer
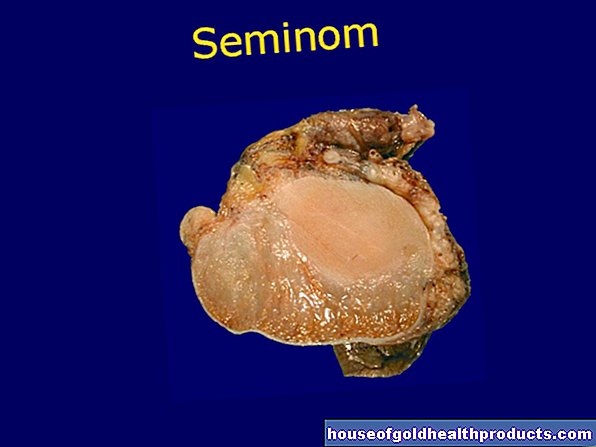
Treatment for lung cancer is influenced by what type of tumor it is. Depending on which cells of the lung tissue become cancer cells, doctors differentiate between two large groups of lung cancer: One of them is small cell lung cancer (SCLC).
This form of lung cancer grows very quickly and forms daughter tumors (metastases) in other parts of the body at an early stage. At the time of diagnosis, the disease is therefore usually well advanced.
The most important treatment method is chemotherapy. Some patients also receive radiation or immunotherapy. If the tumor is still very small, an operation can still make sense.
You can read more about the development, treatment and prognosis of this form of lung cancer in the article SCLC: Small Cell Lung Carcinoma.
Non-small cell lung cancer
Non-small cell lung cancer is the most common type of lung cancer. It is often abbreviated as NSCLC ("non small cell lung cancer"). Strictly speaking, the term "non-small cell lung cancer" encompasses various types of tumors. These include adenocarcinoma and squamous cell carcinoma.
The following applies to all non-small-cell lung cancer: They grow more slowly than small-cell lung cancer and only later form metastases. Instead, they don't respond so well to chemotherapy.
The treatment of choice is therefore an operation whenever possible: The surgeon tries to completely remove the tumor. In more advanced stages, radiation and / or chemotherapy is usually chosen (as a supplement or alternative to surgery). For certain patients, new therapeutic approaches (targeted therapies, immunotherapy) can also be considered.
You can learn more about this widespread form of lung cancer in the post NSCLC: Non-Small Cell Lung Cancer.
Lung cancer: causes and risk factors
Lung cancer occurs when cells in the bronchial system begin to grow in an uncontrolled manner, presumably due to a genetic change. Doctors refer to the large and small airways of the lungs as the bronchial system (bronchi and bronchioles). The medical name for lung cancer is therefore bronchial carcinoma. The word "carcinoma" stands for a malignant tumor made up of so-called epithelial cells. They form the cover fabric that lines the airways.
The uncontrolled growing cells multiply very quickly. In doing so, they increasingly displace healthy lung tissue. In addition, the cancer cells can spread via blood and lymph vessels and form a daughter tumor elsewhere. Such settlements are called lung cancer metastases.
Lung cancer metastases should not be confused with lung metastases: These are daughter tumors in the lungs that originate from cancerous tumors elsewhere in the body. For example, colon cancer and kidney cell cancer often cause lung metastases.
The genetic changes that lead to the development of lung cancer can arise completely randomly as part of normal cell division (without any recognizable trigger) or can be triggered by risk factors.
Smoking: the main risk factor
The most important risk factor for uncontrolled and malignant cell growth in the lungs is smoking. Around 90 percent of all men with lung cancer have actively smoked or are still doing it. In the case of women, this applies to at least 60 percent of the patients. The risk of illness is all the higher:
- the longer someone smokes
- the earlier you started smoking
- the more you smoke
- the more you passively smoke
Passive smoking also increases the risk of lung cancer!
At present, medical professionals assume that of all these factors, the duration of smoking increases the risk of lung cancer the most.
However, the extent of tobacco consumption also plays a major role: Doctors measure the previous cigarette consumption of a patient in the unit pack years. If someone smokes a pack of cigarettes every day for a year, this is counted as "one pack year". If someone smokes one box a day for ten years or two boxes a day for 5 years, that's 10 pack years each. The following applies: the more pack years, the higher the risk of lung cancer.
In addition to the number of cigarettes smoked, the type of smoking also plays a role: the more smoke you inhale, the worse it is for your lungs. The type of cigarette also has an influence on the risk of lung cancer: strong or even filterless cigarettes are particularly harmful.
So, to protect yourself against lung cancer, you should quit smoking! The lungs can then recover, and the better the earlier you stop smoking (i.e. the shorter your smoking career is). Then your risk of lung cancer decreases again.
For example, for male ex-smokers two years after quitting smoking, the risk of lung cancer is only 7.5 times as high as for men who have never smoked. Quitting smoking also reduces the risk of bronchial carcinoma for women, but it is still twice as high as for lifelong non-smokers.
No matter how long and how much you've smoked - it's never too late to quit!
Other risk factors for lung cancer
Aside from smoking, there are other factors that can increase your risk of lung cancer:
- Air pollution: Air pollutants increase the risk of lung cancer, especially diesel soot and fine dust.
- other pollutants: asbestos, arsenic and arsenic compounds have long been known to be carcinogenic. Other substances such as quartz dust, artificial mineral fibers (such as rock wool), polycyclic aromatic hydrocarbons (PAHs), dichlorodimethyl ether, beryllium and cadmium also increase the risk of lung cancer (and other types of cancer).
- Ionizing radiation: Radon is a natural radioactive gas that is carcinogenic and in some places increasingly seeps out of the ground. It accumulates especially in the basement and ground floor of buildings. However, there is also radiation exposure, for example, to flight personnel (cosmic radiation) and during X-ray examinations (X-ray radiation).
- genetic predisposition: to some extent, lung cancer appears to be hereditary. So far, however, it is still largely unclear how important genetic factors are and in which patients they actually contribute to the development of lung cancer. Presumably they play a role especially in very young patients. The genetic predisposition could, for example, make those affected more susceptible to influences that damage the lungs (such as smoking).
- Infections and injuries: Scars in the lung tissue, which can occur as a result of infections (e.g. tuberculosis) or injuries, increase the risk of cancer. It is also being discussed whether the AIDS pathogen HIV and human papillomavirus (HPV) promote the development of lung cancer - either directly or through another connection.
- Low-vitamin diet: Eating little fruit and vegetables apparently increases the risk of lung cancer. This is especially true for smokers. However, taking vitamin supplements is not an alternative: such supplements seem to increase the risk of bronchial cancer even further, especially in smokers.
If several of these factors are present at the same time, the probabilities of lung cancer not only add up: rather, the risk of the disease increases many times over. For example, high air pollution increases the risk of lung cancer in smokers much more than in non-smokers.
Sometimes the cause of lung cancer cannot be found. One then speaks of an idiopathic disease. Of all lung cancer types, the most common is what is known as adenocarcinoma. This is a form of non-small cell lung cancer.
Lung cancer: examinations and diagnosis
The diagnosis of lung cancer is often made late. Symptoms such as persistent cough, chest pain and shortness of breath are often not recognized as possible signs of lung cancer, especially by smokers - most patients simply blame smoking. Others suspect a severe cold, bronchitis, or pneumonia is behind the symptoms. Only medical examinations then reveal the suspicion of bronchial carcinoma.
The first point of contact for possible symptoms of lung cancer is the family doctor. If necessary, he will refer the patient to specialists, for example to an X-ray specialist (radiologist), pulmonologist (pulmonologist) or cancer specialist (oncologist). In order to be able to make the diagnosis of lung cancer, a survey of the medical history, physical examinations and various apparatus-based examinations are necessary.
Medical history and physical exam
First, in a conversation with the patient, the doctor creates the patient's medical history (anamnesis): He has the symptoms such as shortness of breath or chest pain described in detail. He also asks about risk factors for lung cancer. For example, he asks whether the patient smokes or works with materials such as asbestos or arsenic compounds.
Information on possible pre-existing or underlying diseases such as COPD or chronic bronchitis is also important for the diagnosis of lung cancer. Patients should also tell the doctor if there has been a history of lung cancer in their family.
After the anamnesis discussion, the doctor will carefully examine the patient physically. Among other things, he taps and listens to the patient's lungs and measures blood pressure and pulse. The examination can provide possible clues as to the cause of the symptoms. In addition, the doctor can better assess the general health of the patient.
roentgen
Using a chest x-ray (chest x-ray), the doctor can already detect changes in the lung tissue. If lung cancer is suspected, the next step is computed tomography (CT).
The doctor x-rays the patient's chest in two planes, i.e. from the front and from the side.
Computed tomography (CT)
Computed tomography provides detailed cross-sectional images of the lungs in high resolution. This is possible with the help of X-rays, which are much more dosed than a normal X-ray examination. In addition, a contrast agent is administered to the patient in advance. In this way, the various tissue structures can be better represented.
The doctor can use the CT to assess suspicious lung changes better than the X-ray images. This can corroborate the suspicion of lung cancer.
Examination of tissue samples (biopsy)
In order to be sure whether a suspicious area in the lung tissue is actually a bronchial carcinoma, a small piece of tissue must be removed and examined under the microscope. Depending on the location of the suspicious area, different methods are used:
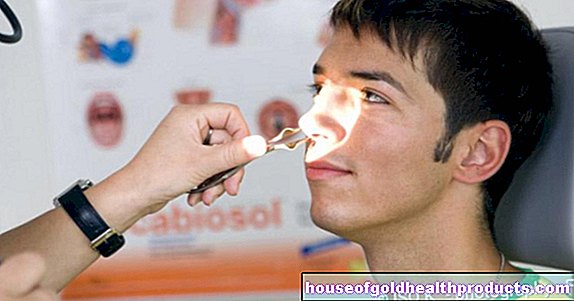
In a lung specimen (bronchoscopy), a tube-shaped instrument with a tiny camera and a light source at the tip (endoscope) is inserted through the mouth or nose into the patient's windpipe and further into the bronchi. This allows the doctor to look inside the lungs. A tumor can often be seen optically. In addition, the doctor can take tissue samples and secretions from the lungs via the endoscope with the help of fine instruments in order to have them analyzed more precisely.
If it is difficult or impossible to reach the suspicious tissue via the bronchi, the doctor carries out what is known as a transthoracic needle aspiration: Here, he pricks between the ribs from the outside with a very fine needle. Under CT control, he shows the needle tip to the suspicious lung area. He then sucks in (aspirates) a bit of tissue through the needle.
In some patients, bronchoscopy and transthoracic needle aspiration are not possible, or both examinations do not give a clear result. A surgical biopsy may then be necessary: Either the surgeon opens the chest with a larger incision (thoracotomy) and takes a sample of the suspicious tissue. Or he makes small incisions in the chest, through which he introduces a small camera and fine instruments for tissue removal (video-assisted thoracoscopy, VATS).
Regardless of the way in which the tissue removal is carried out - the removed tissue sample is examined under the microscope. As a rule, just a few cells can be used to tell whether there is lung cancer and, if so, what type of tumor (cytological diagnostics). Only in special cases is it necessary to examine larger tissue sections (histological diagnosis).
Investigation of tumor spread (staging)
Once the diagnosis of lung cancer has been made, the next step is to examine its spread in the body. Doctors refer to this section of the examination as staging. Only through such staging can bronchial carcinoma be classified according to the TNM classification.
Staging consists of three steps:
- Examination of the tumor size (T status)
- Examination of lymph node involvement (N status)
- Search for metastases (M status)
Examination of the primary tumor (T status)
First of all, one examines the size of the tumor from which the lung cancer originates (primary tumor). For this purpose, the patient is given a contrast medium before his chest and upper abdomen are examined using computed tomography (CT). The contrast agent accumulates mainly in the tumor tissue for a short time and causes a mark on the CT image. This allows the doctor to assess the extent of the primary tumor.
If the CT examination is not conclusive enough, other methods are used. This can be, for example, an ultrasound examination of the chest (thorax sonography) or a magnetic resonance tomography (MRT) - also known as an internal spin tomography.
Examination of lymph node involvement (N status)
In order to be able to plan the therapy optimally, the doctor must know whether the lung cancer has already affected lymph nodes. The examination using computed tomography (CT) also helps here. A special technique is often used here: the so-called FDG-PET / CT. This is a combination of positron emission tomography (PET) and CT:
Positron Emission Tomography (PET) is a nuclear medicine examination. First a tiny amount of a radioactive substance is injected into a vein of the lying patient. The FDG-PET / CT is FDG. This is a radioactively marked simple sugar (fluorodeoxyglucose). It is distributed in the body and particularly accumulates in tissues with increased metabolic activity, for example in cancerous tissue. During this time, the patient must remain as calm as possible. After about 45 (up to 90) minutes, the PET / CT scan is performed to visualize the distribution of FDG in the body:
The PET camera can show the different metabolic activity in the different tissues very well. Particularly active areas (such as cancer cells in lymph nodes or metastases) literally "glow" on the PET image. However, PET cannot display bones, organs and other structures of the body as well. This is done almost simultaneously by computed tomography (CT) - PET camera and CT are combined in one device. It allows a very precise representation of the various anatomical structures. In combination with the exact mapping of the metabolic activity, cancer foci can be precisely localized.
Using FDG-PET / CT, metastases from lung cancer in lymph nodes and organs and tissues further away can be displayed very precisely. To be on the safe side, the doctor can take a tissue sample from the suspicious areas and examine it for cancer cells (biopsy).
Search for metastases (M status)
The spread of cancer cells to other organs is a major problem in lung cancer. Metastases are particularly common in the liver and brain, as well as in the bones and adrenal glands. In principle, however, any body structure can be attacked by cancer cells. Lung cancer that has already spread is no longer considered curable.
With the special FDG-PET / CT examination described above, metastases can be detected anywhere in the body. In order to find possible settlements in the brain, the skull is also examined using magnetic resonance imaging (MRI).
FDG-PET / CT is not possible in some patients. The alternative is then a computed tomography or ultrasound examination of the trunk and, in addition, a so-called skeletal scintigraphy (bone scintigraphy). Whole-body MRI images are also possible.
If necessary, other examination methods can also be used for staging, such as an endoscopic examination of the pleural cavity (thoracoscopy).
Blood tests
There are no blood tests that can be used to reliably diagnose lung cancer. However, so-called tumor markers can be determined in the blood. These are substances the blood level of which can be increased in the case of Kresber disease. This is because the tumor markers are either produced to a greater extent by the cancer cells themselves or by the body in response to the cancer. In lung cancer, for example, the tumor markers neuron-specific enolase (NSE) and CYFRA 21-1 can be increased.
The measurement of tumor markers only plays a subordinate role in the diagnosis of lung cancer and is not routinely recommended here. The measured values alone are not meaningful - on the one hand, tumor makers are not detectable in all patients and, on the other hand, they can sometimes also be found in the blood of healthy people.
Tumor markers are more relevant when assessing the course of the disease: the concentration of tumor markers in the blood can give the species clues as to how fast the tumor is growing or whether cancer cells reappear after treatment.
Examination of the sputum
The sputum that a patient coughs up from the lungs can be checked for the presence of cancer cells. This method is mainly used when it is not possible to take a tissue sample (for example because the patient is in poor health).
If the sputum is normal, this does not necessarily mean that there is no lung cancer. The examination of the sputum serves more to confirm an existing suspicion.
Examination of lung water
"Lung water" often forms in lung cancer patients. This means that more fluid collects between the pleura and the pleura. Such a pleural effusion can also have other causes. For clarification, the doctor will take a sample of the effusion through a fine hollow needle (pleural puncture) and examine it microscopically. In this way he can determine what caused the effusion.
Are there screening examinations for lung cancer?
General screening tests, such as those used for breast cancer, colon cancer or skin cancer, are difficult for lung cancer. For example, you could regularly take chest x-rays or examine the sputum for cancer cells. Such preventive examinations are either too imprecise or too sensitive (they could therefore result in an unfounded suspicion of cancer). In addition, regular X-ray or CT examinations mean exposure to radiation for the person concerned.
However, people who are at high risk of lung cancer could benefit from preventive medical check-ups - for example, smokers and people who have professional contact with cancer-causing substances. For example, studies have been carried out in which high-risk patients were regularly examined using computed tomography (CT) with low radiation dose (low-dose CT). In this way, bronchial cancer could be detected earlier in heavy smokers, for example. But this still needs to be investigated in more detail.
Nevertheless, the current guidelines already recommend annual lung cancer screening with low-dose CT for certain risk groups (e.g. heavy smokers aged 55 and over). However, this early detection is not (yet) part of the statutory catalog of health insurance benefits, so it has to be paid for out of pocket.
Lung cancer: disease course and prognosis
There is a special aftercare plan for patients who have received therapy with the intention of healing (curative therapy). After completing treatment, those affected should go to the hospital for check-ups at regular intervals. Regular X-ray and CT images are particularly important. The doctor will assess each of these in comparison to the last recordings of the patient.
Even patients who are no longer expected to cure are regularly examined by the doctor. In this way, it can be determined whether the palliative therapy sufficiently alleviates the symptoms or whether it may need to be adjusted.
Lung cancer: prognosis
Overall, lung cancer has a poor prognosis: Lung cancer is only discovered in many patients when the disease is well advanced. A cure is then often no longer possible. If the lung cancer is discovered in the early stages, you may be able to operate. After a while, however, a new cancer tumor often forms (relapse = relapse).
Precisely because the chances of a cure are so slim, it is important not to unnecessarily increase the risk of lung cancer. The most important factor that everyone has in their own hands is smoking. Those who refrain from smoking or do not even begin to smoke significantly lower their personal risk of bronchial carcinoma. The prognosis and course of an existing lung cancer can also be improved by quitting smoking.
Lung Cancer: Life Expectancy
People diagnosed with lung cancer often ask themselves the question: "How long will I live?" It is not easy for the doctor to answer this question. Life expectancy with lung cancer depends on various factors:
For example, how advanced the tumor is at the time of diagnosis plays a role. Lung cancer is often discovered late, which has a detrimental effect on the patient's life expectancy. The type of tumor also has an impact on survival: non-small-cell lung carcinomas grow more slowly than small-cell carcinomas. You therefore generally have a better prognosis.
The general state of health is also important: if, for example, a patient's heart and lung function are significantly weakened, certain forms of treatment may only be carried out to a limited extent or not at all. This can significantly reduce the life expectancy of lung cancer patients.
You can find more information on life expectancy and a cure for lung cancer in the text Lung Cancer: Life Expectancy.
Additional information:
Guidelines:
- S3 guideline "Prevention, diagnosis, therapy and aftercare of lung cancer" of the German Society for Pneumology and Respiratory Medicine e.V. and the German Cancer Society (as of 2018)
Self-help groups:
- Federal Association for Self-Help Lung Cancer e.V .: http://www.bundesverband-selbsthilfe-lungenkrebs.de/
- Self-help lung cancer: http://www.selbsthilfe-lungenkrebs.de
- German Cancer Aid e.V .: https://www.krebshilfe.de/helfen/rat-hilfe/selbsthilfe/
- Lung Cancer Forum Austria: http://lungenkrebsforum-austria.at/
- Lung League Switzerland: www.lungenliga.ch
Tags: stress Baby Child sports fitness