Celiac Disease Test
Ricarda Schwarz studied medicine in Würzburg, where she also completed her doctorate. After a wide range of tasks in practical medical training (PJ) in Flensburg, Hamburg and New Zealand, she is now working in neuroradiology and radiology at the Tübingen University Hospital.
More about the experts All content is checked by medical journalists.A celiac disease test determines antibodies in the blood serum that are typical for gluten intolerance. In some cases, however, the patient has celiac disease even though the test does not work. Further examinations are then necessary to ensure the diagnosis of celiac disease. Read here how the celiac disease test works and what to watch out for.

Celiac Disease Test: Antibodies
If gluten intolerance is suspected, a gluten allergy test should be carried out before changing your diet. To do this, the doctor takes a blood sample and tests it for certain immunoglobulins.These are antibodies that are directed against transglutaminase (anti-TG) and against the endomysium (EmA).
Transglutaminase is a protein (enzyme) in the intestinal mucosa that processes the glutamine contained in gluten. In celiac disease, the body makes antibodies against the enzyme. They circulate in the blood and attack the transglutaminase, which causes the intestinal lining to become inflamed.
In addition, the immune system in people with celiac disease also makes antibodies against the so-called endomysium. The endomysium is a layer of connective tissue in the intestinal wall. If it is attacked, the villi of the intestinal wall break down. The concentration of the endomysial antibodies therefore allows a conclusion to be drawn as to how much the intestinal villi have regressed.
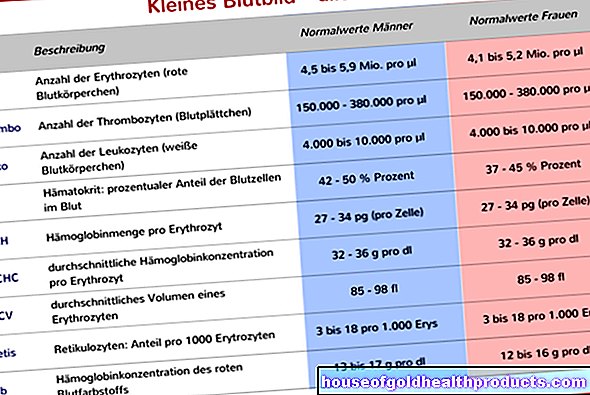
The total amount of class A antibodies (immunoglobulin A / IgA) should also be determined as part of the celiac disease test.
Doctors divide immunoglobulins into different classes: G, A, M, D and E. The transglutaminase and endomysium antibodies active in celiac disease belong to group A.
Gluten intolerance is often associated with an IgA deficiency. This is problematic for the diagnosis: If the total amount of antibodies is too low, antibodies against transglutaminase or the endomysium cannot be detected at all or only with difficulty in a blood test. Doctors refer to this as a false negative test result. This means that the all-clear is falsely given, although the typical celiac antibodies are actually present in the blood.
The celiac disease test, which is easy to carry out, detects over 74 percent of people with a gluten intolerance. If this celiac disease test is negative at a normal IgA concentration, gluten intolerance is very unlikely.
Celiac disease test for IgA deficiency
In another celiac disease test, antibodies against the gluten component gliadin are detected. However, this test is only useful in the case of IgA deficiency. As part of an initial celiac disease diagnosis, it is not carried out as standard. The accuracy of this test is always under discussion. Instead, if there is an IgA deficiency, transglutaminase antibodies of the IgG group can also be determined.
Celiac Disease Self-Test
Various manufacturers now offer celiac self-tests in different price ranges. They can also be used to detect the antibodies transglutaminase and endomysium antibodies typical of celiac disease in the blood.
How do you do the celiac disease self-test?
A celiac disease self-test (also known as a "gluten self-test") is comparable to a pregnancy test. However, you need a small drop of blood instead of urine for the self-test. The test kit is available without a prescription in pharmacies and on the Internet. It contains a lancet for collecting a drop of blood, a small capillary tube, a test solution in a reaction vessel, a pipette and a test cassette.
For the test, the end of the test pricks his fingertip with the lancet so that a small drop of blood oozes out. He picks up this with a small capillary tube. This is placed in a liquid-filled reaction vessel and shaken a little. The end of the test then soaks up the blood-liquid mixture with a pipette and places a drop on a field provided within the test cassette. After a few minutes, the result can be read from a color change.
Does the celiac disease self-test make sense?
However, experts advise against a celiac disease self-test. The tests are very imprecise. A gluten self-test can therefore only serve as a first orientation. But it certainly cannot replace a detailed medical diagnosis, including professional blood tests and a possible collection of tissue samples from the small intestine. Similar rapid tests, in which stool or saliva are examined, are also not reliable enough.
Some manufacturers of the test kits advertise with an allegedly almost 100 percent certainty of the test result. However, if you consider that erroneous results cannot even be ruled out in a professional, elaborate blood test at the doctor's, this claim can hardly stand up to a serious examination. For example, a rapid celiac disease test is prone to an erroneous test result if the patient is immunoglobulin A deficient.
After a positive result, the patient has to see a doctor anyway, who will carry out the complete diagnosis again. A negative result of the celiac disease self-test, on the other hand, only offers dubious certainty. For those with statutory health insurance, there is also the fact that many health insurance companies cover the costs of a doctor's diagnosis, while a celiac self-test has to be paid for out of your own pocket.
Celiac disease: test of the air you breathe (H2 breath test)
With pronounced celiac disease, a large part of the intestinal villi has regressed. This reduces the surface area of the intestine and the nutrients can only pass into the blood to a limited extent (resorption disorder). In some of these digestive disorders, this also applies to the sugar molecule xylose. It therefore reaches the large intestine with the rest of the food pulp, where it is broken down by bacteria. This creates hydrogen (H2), which is transported into the lungs and then exhaled.
With a xylose test, the doctor measures the H2 concentration in the breath of an empty patient before and after giving a xylose drink solution. An increased hydrogen concentration indicates an absorption disorder, the cause of which can be celiac disease. However, since there are other reasons for a resorption disorder, it is not a specific celiac disease test.
Celiac Disease Test: Children
Although separate recommendations for antibody determinations have been made in many guidelines for children under two years of age, there was and still is insufficient evidence for this. More recent studies show a similarly good sensitivity and specificity for tTGIgA antibodies and EmA-IgA antibodies for this age group as in older children and adults.
If no antibodies can be measured in the celiac disease test in children (including screening tests for risk groups), the antibody levels should be checked again in them (in contrast to adults) at the following intervals: in the first two years every six months, then after five and after ten years.
In some cases, a tissue sample from the small intestine can be dispensed with in children with suspected celiac disease. This is the case if the children suffer from symptoms of celiac disease, show typical signs of a disordered use of food and, moreover, meet the following four criteria:
- In the celiac disease test, the transglutaminase antibodies reach a value ten times higher than the limit value.
- Endomysial antibodies can be detected.
- There is a genetic predisposition for celiac disease (HLA-DQ2 and / or -DQ8)
- The symptoms subside on a gluten-free diet.



















.jpg)