Type 1 diabetes: tutoring the immune system
Christiane Fux studied journalism and psychology in Hamburg. The experienced medical editor has been writing magazine articles, news and factual texts on all conceivable health topics since 2001. In addition to her work for, Christiane Fux is also active in prose. Her first crime novel was published in 2012, and she also writes, designs and publishes her own crime plays.
More posts by Christiane Fux All content is checked by medical journalists.Not everyone with genes at risk for type 1 diabetes will get sick. In the first two years of life it is decided whether the immune system will later attack the insulin-producing cells in the pancreas or not. Researchers from the Helmholtz Center in Munich want to use insulin powder in baby food to track down immune cells.
Karoline * is 26 years old, a sports student - and diabetic. She has type 1 diabetes, just like her father. In addition to the red curly hair and freckles, he probably also passed the risk genes for the disease on to his daughter.
Karoline has lived with type 1 diabetes since she was eleven - and has the disease under control. “Diabetes is a part of me,” the young woman said in an interview with, “but I would have liked to have done without it.” She is currently focusing more on her illness again: She is five months pregnant.
Immune cells exercise program
It could not be prevented that she, too, presumably passed risk genes on to her child. But there is one method that may prevent the onset of the disease: an immune system exercise program.
The process was developed by researchers from Helmholtz Zentrum München. As part of a study, they are treating children who are at increased risk of type 1 diabetes with insulin. Until their third birthday, they receive the hormone in powder form daily with their food.
"The course for diabetes is set early"
"We know that the course for diabetes is set very early in life," explains the head of the study, Prof. Anette-Gabriele Ziegler *, to "We hope that we can stop the process in this time window by supporting the immune system to tolerate insulin and thus flipping the switch again."
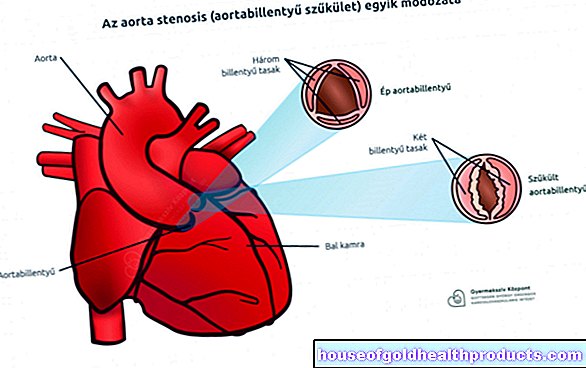
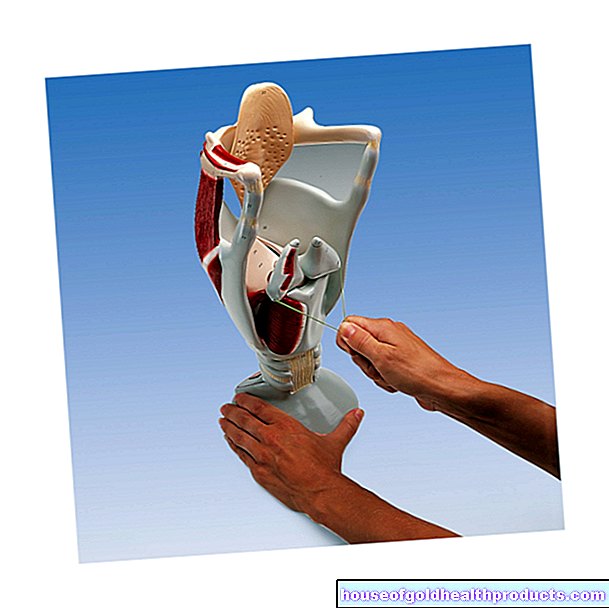
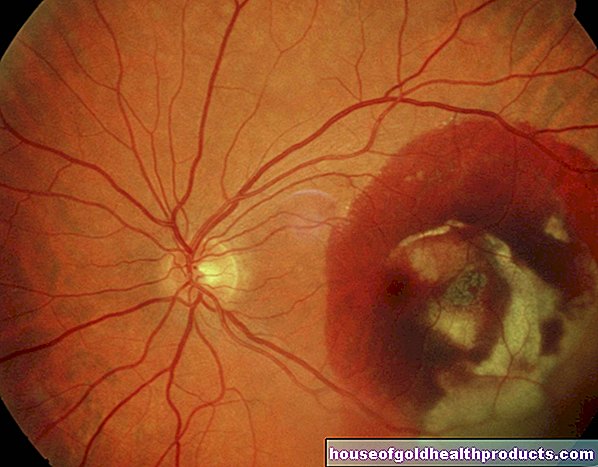
Malfunctioning immune cells
In an autoimmune disease, certain immune cells, so-called autoactive T cells, fight their own cells as if they were pathogens. In type 1 diabetics, for example, they attack the insulin-producing cells in the pancreas, the so-called beta cells. Then the patient has less and less insulin available. However, the hormone is necessary to shovel sugar from the blood into the body's cells. If that doesn't happen, the blood sugar will rise dangerously.
Education for more tolerance
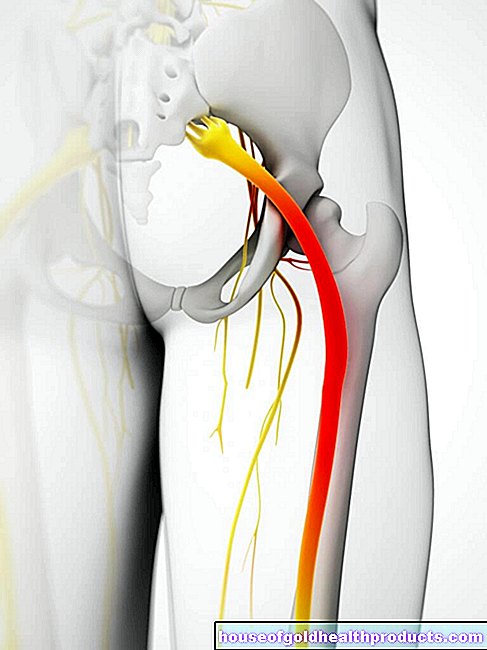
Normally, the T cells are trained in their place of birth, the thymus, to tolerate endogenous proteins such as those of insulin or islet cells. T cells that don't do this are sorted out and self-destruct.
However, some of these autoreactive T cells escape and get into the blood. So-called regulatory T cells patrol there so that they do not cause any damage. They usually keep their autoreactive colleagues from attacking healthy body cells.
“In children with type 1 diabetes, however, something goes wrong with the selection process,” says Ziegler. Too many autoreactive T cells enter the body. They are initially directed against insulin. Later they also attack the beta cells.
Ziegler and her colleagues want to make the children's immune system more tolerant of the hormone with daily insulin doses. Her strategy: “We are trying to strengthen the regulatory cells so that they intercept the autoreactive cells. We also give insulin to sensitize the cells, ”says the diabetes researcher.
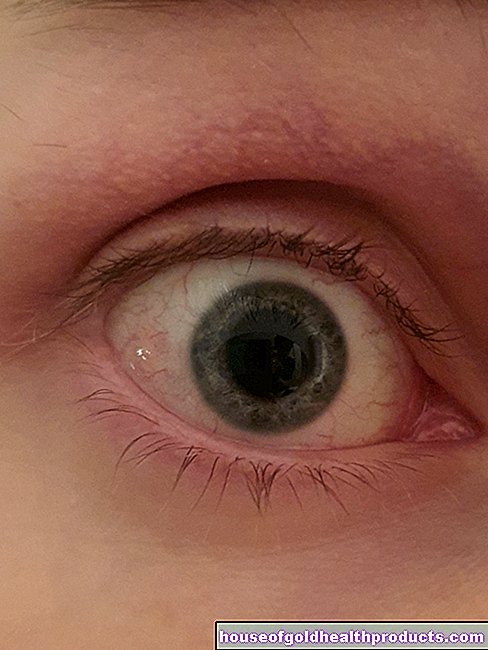
Encounters in the gut
In the gastrointestinal tract, the administered insulin encounters immune cells, which cavort there in particularly large numbers. Each time they eat food, they have to decide whether they are dealing with valuable nutrients that are allowed to pass through the intestinal wall. Or whether there are potential pathogens that need to be fought off. "If the immune cells are confronted with insulin on a daily basis, they increasingly accept it," says Ziegler.
The researchers have already been able to demonstrate in a small pilot study that the tutoring lessons actually work in tolerance: the hoped-for immune response had developed in the blood of the children treated. Regulatory T cells specialized in the protection of insulin romped about in it. “That is a very good sign and gives us hope,” says Ziegler.
The immune system can be programmed
Another study with children at high risk of peanut allergy has shown that the immune system can actually be programmed at an early age. Even as babies, they received comparatively large amounts of peanuts. "That is the exact opposite of what has been recommended so far when there is a higher allergy risk, namely avoiding allergens as much as possible," says Ziegler. The success was resounding: none of the children later reacted allergic to the legumes.
Manhunted in Bavaria, Saxony and Lower Saxony
As part of the so-called POInT study with a larger number of children at risk, the researchers are currently investigating whether and how well daily insulin administration works for diabetes prevention. The federal states of Bavaria, Saxony and Lower Saxony are involved across the board. There all parents have the opportunity to have their babies' genetic risk tested. One tiny drop of blood is enough to identify 42 genes that increase the likelihood of type 2 diabetes.
A droplet of blood is taken from the children with a finger prick. Depending on which genes are found in them and how strong their respective influence is, the researchers use a mathematical model to calculate the little ones' individual risk of diabetes. If it is 25 times higher than normal, the children can take part in the study.
First results in 2025
The aim is to treat at least 1,000 children with powdered insulin, of whom at least 100 would normally develop type 1 diabetes. An equally large group of children at risk should serve as controls - instead of insulin, they receive an ineffective powder.
"As early as 2025 we will be able to say whether the insulin administration helped or not," says Ziegler. With the help of special antibodies that are already formed in the blood in advance of diabetes, it can then be determined with certainty whether the children will one day get sick or not.
Have it tested - also in other federal states!
Karoline lives in Hamburg and not in one of the participating federal states. She can still test her child and, if necessary, have them participate. This option is available to all children who have parents or siblings with type 1 diabetes.
“I will definitely take the test,” says the mother-to-be. "In the best case, I find out that I don't have to worry." And if the risk for the child is actually increased, participating in the study could possibly prevent the disease from breaking out. “Life is good even with diabetes. But of course it's easier to live without it. "
Prof. Anette-Gabriele Ziegler is director of the Institute for Diabetes Research at the Helmholtz Zentrum München and heads the Chair for Diabetes and Gestational Diabetes at the Klinikum rechts der Isar of the Technical University of Munich.
Tags: home remedies healthy feet foot care