Lymphatic drainage
Dr. med. Philipp Nicol is a freelance writer for the medical editorial team.
More about the experts All content is checked by medical journalists.Lymph drainage (decongestion therapy, manual lymph drainage, MLD) is a special, medical form of massage. It is part of the “Complex Physical Decongestion Therapy” and is used for congestion in the tissue fluid (lymphedema). Read everything you need to know about this procedure, when it is done, and the risks involved.

What is lymphatic drainage?
Lymphatic drainage is used to treat lymphedema. Lymphedema occurs when the lymphatic drainage is disturbed as a result of a chronic, inflammatory disease of the interstitium (space between cells, tissues, organs) so that fluid accumulates in the tissue. This can be recognized by a clearly visible swelling. Lymphedema often occurs on the limbs; however, lymphedema can also develop in the face.
Lymphedema can be congenital (primary lymphedema). Much more often, however, they are caused by another disease. Such secondary lymphedema is usually caused by cancer. For the treating therapist, any lymphedema is therefore suspect until the opposite is proven.
In the initial stages of lymphedema treatment, patients should receive lymphatic drainage once or twice a day. This can happen on an outpatient or inpatient basis. The "complex physical decongestion therapy" knows a total of four basic procedures for lymphedema:
- Compression therapy using bandages
- Decongesting movement exercises
- Skin care
- Manual lymph drainage
Legs and arms are primarily affected by lymphedema and can therefore be treated with lymphatic drainage. The face and torso can also be treated with this procedure.
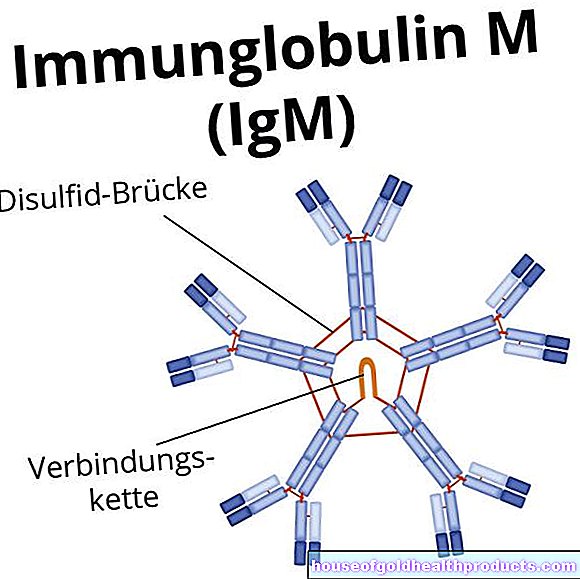
The effect of lymphatic drainage is essentially based on four effects, namely the decongesting, the pain relieving and the muscle relaxing effect as well as a strengthening effect on the immune system. The latter effect, however, is medically controversial.
When do you perform lymphatic drainage?
Edema therapy is often used for the following diseases:
- Chronic lymphedema
- Chronic venous insufficiency (often visible in the form of "varicose veins")
- Post-operative swelling
Lymphatic drainage can also be beneficial for other diseases, but it is less of a therapeutic value. These include:
- Chronic polyarthritis
- CRPS (complex regional pain syndrome, formerly Sudeck's disease)
- Swelling after hemiparesis in a stroke
- headache
In addition, there are other, non-disease-related areas of application for lymphatic drainage: For example, pregnancy can lead to edema in women, which mainly occurs in the evening and after long periods of standing. These do not necessarily require treatment, but can be very stressful for a pregnant woman. Then lymph drainage helps. Cellulite is another area of application. However, the effect of lymphatic drainage has not been scientifically proven.
When is lymphatic drainage not advisable?
Lymphatic drainage should not be used in certain illnesses. These include:
- malignant tumors
- acute inflammation
- severe cardiac insufficiency (decompensated heart failure grade III-IV)
- Cardiac arrhythmias
- very low blood pressure (hypotension, below 100/60 mmHg)
- acute deep thrombosis of the leg veins
- Overactive thyroid (hyperthyroidism) or carotid sinus syndrome (especially relevant for lymphatic drainage on the neck)
- unclear skin changes (erysipelas)
What do you do with lymphatic drainage?
With lymphatic drainage, the lymphatic vessels should be stimulated and stimulated to increase the removal of the lymphatic fluid. Increased blood flow or activation of pain receptors in the skin is not the aim of lymphatic drainage. “Massage” in its classic form, on the other hand, works through both mechanisms.
The therapist achieves the special effect of lymphatic drainage through circular movements. The following four basic grips are particularly important:
- standing circle
- Pump handle
- Scoop handle
- Twist grip
These handles are basically used. Depending on the cause of the edema, so-called “supplementary grips” are added.
After the treatment, the corresponding part of the body is wrapped ("compression therapy"). This prevents the edema from developing again after the manual lymphatic drainage is finished. Lymph drainage should be carried out by a specially trained physiotherapist.
Lymphatic drainage of the head and neck region
Lymph drainage of the head and neck region is usually started on the neck or shoulder. It is therefore also referred to as "basic therapy". The therapist begins the treatment and then slowly works his way from the trunk to the extremities. This is followed by lymphatic drainage on the face. This type of lymphatic drainage usually results in a very extensive "relaxation effect". The eyes, jaw, forehead and nose are treated individually and one after the other.
Lymphatic drainage of the extremities and trunk
The extremities are also often the starting point for lymphatic drainage: the arm and leg are often affected by lymphedema. For example, as part of radiation therapy for breast cancer or removal of lymph nodes in the armpit, edema develops on the arm.
The treatment on the arms begins in the armpit area, before you then work your way up to the hand using the upper arm. Here, too, the basic grips may be expanded to include additional grips. On the legs, you start with the lymphatic drainage on the groin (knees and buttocks can be treated with special handles).
What are the risks of lymphatic drainage?
If lymphatic drainage is carried out properly by a trained therapist and certain clinical pictures have been ruled out in advance, there are usually no risks.
What do I have to consider after lymphatic drainage?
No special behavior is required after the lymphatic drainage. However, there are some things you can do to prevent the lymphedema from coming back too quickly:
- Clothing: Make sure that you do not wear tight or constricting clothing, which will make the lymphatic drainage even more difficult. The same goes for watches, jewelry and footwear.
- Skin care: As there is an increased risk of infection with lymphedema, you should carefully care for your skin, preferably with a pH-neutral cream. Take care when caring for your nails - even small injuries can be entry points for pathogens. You may want to consider medical foot care.
- Household: Wear gloves when doing housework or gardening! Elevate your legs regularly for better lymph drainage.
- Leisure time: In sporting activities you should limit yourself to "light" movements (walking, Nordic walking, swimming, etc.). Avoid extensive sunbathing, sauna or solarium visits - this will damage your skin!
Basically, lymphatic drainage is an effective and safe method for treating lymphedema that is well tolerated.
Tags: toadstool poison plants gpp foot care