Dengue fever
and Sabine Schrör, medical journalist and Carola Felchner, science journalistFabian Dupont is a freelance writer in the medical department. The human medicine specialist is already doing scientific work in Belgium, Spain, Rwanda, the USA, Great Britain, South Africa, New Zealand and Switzerland, among others. The focus of his doctoral thesis was tropical neurology, but his special interest is international public health and the comprehensible communication of medical facts.
More about the expertsSabine Schrör is a freelance writer for the medical team. She studied business administration and public relations in Cologne. As a freelance editor, she has been at home in a wide variety of industries for more than 15 years.Health is one of her favorite subjects.
More about the experts
Carola Felchner is a freelance writer in the medical department and a certified training and nutrition advisor. She worked for various specialist magazines and online portals before becoming a freelance journalist in 2015. Before starting her internship, she studied translation and interpreting in Kempten and Munich.
More about the experts All content is checked by medical journalists.Dengue fever is a tropical viral disease. It is transmitted by a specific type of mosquito, the diurnal Aedes mosquito. Dengue fever manifests itself in a greatly increased temperature, headache and body aches. Those affected usually recover within a few days. Dengue fever can also lead to serious complications or even death. Find out here in which regions the tropical disease occurs, how you can avoid infection and how dengue fever is treated.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. A97
Brief overview
- What is dengue fever? A viral infection transmitted by the Aedes mosquito.
- Occurrence: mainly in tropical and subtropical countries, but also (occasionally) in Europe.
- Symptoms: sometimes none, otherwise typically flu-like symptoms (such as fever, chills, headache and body aches, muscle pain); in case of complications Blood clotting disorders, vomiting, drop in blood pressure, restlessness, drowsiness
- Treatment: symptomatic with hydration and pain relievers and fever medication; in-patient intensive care in the event of complications
- Prognosis: mostly benign course; increased risk of complications in children and secondary infections
- Prevention: Avoiding mosquito bites (long clothes, mosquito net, mosquito repellent, etc.)
Dengue fever: routes of infection and occurrence
Dengue fever is caused by the dengue virus, which comes in four different variants (serotypes): DENV 1-4. All of them are transmitted by the Aedes mosquito - most often by the yellow fever or tiger mosquito (Aedes aegypti or Stegomyia aegytpi), sometimes also by the Asian tiger mosquito (Aedes or Stegomyia albopictus).
This is how dengue fever is transmitted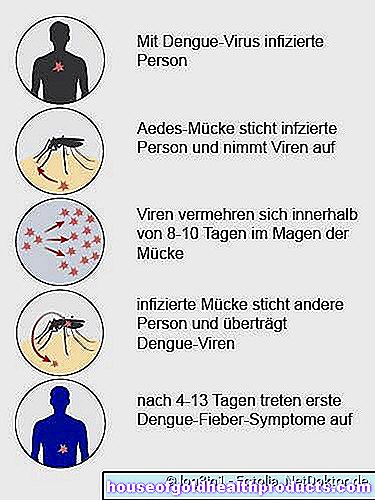
Dengue fever is usually transmitted to humans by Aedes mosquitoes. Such animal carriers are called "vectors".
These mosquitoes are mainly found in urban areas or generally in human-populated areas. They prefer to lay their eggs near water (bottles, rain barrels, buckets, etc.). If females are infected, they can transmit the virus directly to the brood. It is also the female mosquitoes that pass the disease on to humans.
Can people infect each other with dengue?
Usually people become infected with dengue viruses through a bite from Aedes mosquitoes. The stinging animals can also absorb the infected blood of sick people and transmit it to other people.
A direct dengue transmission from person to person - i.e. without the presence of Aedes mosquitoes - does not usually take place.
In contrast to flu viruses, for example, dengue viruses do not occur in saliva according to current knowledge. Dengue fever cannot be transmitted through sneezing, coughing or kissing. However, there are individual cases in which researchers assume that people have become infected through unprotected sexual intercourse.
The European Center for Disease Prevention and Control (ECDC) therefore advises that patients with or suspected of having dengue fever should not practice or practice safer sex during the period of illness. However, the experts also emphasize that further studies are necessary for a more precise statement.
So far, researchers have been able to detect dengue virus RNA in semen, vaginal secretions and urine. To what extent an infection can occur through this remains unclear (it is also conceivable that an infection through small injuries that occurred during sexual intercourse and infected blood is transferred is also conceivable). A positive test does not necessarily mean that the person affected is contagious, as it only detects the genetic make-up of the dengue virus.
There are also isolated reports of pregnant women who have passed the virus on to their unborn child via the blood. Doctors call this transmission path vertical transmission. A transmission of the virus through breast milk has so far been assumed in a single case. In addition, the dengue virus can be infected through infected blood (transfusions, needlestick injuries).
Although very rarely reported, the direct transmission of the dengue virus between people does not play a relevant role in the spread of dengue fever, according to experts. The transmission via Aedes mosquitoes is decisive.
Occurrence of dengue fever
Dengue fever is the most common and fastest spreading mosquito-borne infectious disease worldwide. Southeast Asia, South and Central America, parts of the Pacific such as New Caledonia and Hawaii as well as Africa and Australia are particularly affected.
Due to global warming, the Asian tiger mosquito is meanwhile also widespread in southern Europe and is expanding its settlement area further. In recent years, there have been isolated local dengue infections in Europe, such as in Madeira, Croatia, France or Spain. Experts fear that the mosquito will also increasingly spread to continental Europe.
The Aedes mosquito is not at home in Germany so far. German dengue fever patients were infected in tropical and subtropical countries. Since Germans like to travel more and more, the number of dengue fever cases introduced has risen sharply in recent years. Around 600 cases were reported in Germany in 2018.
According to the reporting data of the Infection Protection Act (IfSG), the most common countries of infection in 2018 were:
- Thailand: 38 percent
- India: 8 percent
- Maldives: 5 percent
- Indonesia: 5 percent
- Cuba: 4 percent
- Cambodia: 4 percent
- Sri Lanka: 4 percent
- Vietnam: 3 percent
- Mexico: 2 percent
- Tanzania: 2 percent
- Others: 25 percent
Dengue fever is one of the notifiable diseases in Germany. This means that the attending physician must report every case to the health department. This measure should help to identify larger outbreaks as quickly as possible and to be able to take countermeasures.
Dengue fever: diseases are on the rise
Dengue fever has spread over the past few decades. In the past 50 years, the number of people infected has increased thirty-fold. Experts estimate that between 284 and 528 million people worldwide contract the dengue virus every year.
Dengue fever: symptoms
The time between the bite of the Aedes mosquito and the appearance of the first symptoms (incubation period) is three to 14 days. Most of the time, the infection breaks out between the 4th and 7th day.
The symptoms of dengue fever are often very unspecific and resemble those of ordinary flu: Typically, the patient has a high fever (up to 40 degrees Celsius), chills, headache, pain in the joints and limbs. Because of the severe muscle pain, dengue fever is also called "bone breaker fever". The fever is often biphasic (biphasic). Along with the second bout of fever, a rubella-like, itchy rash may appear all over the body. Other possible accompanying symptoms in dengue fever are, for example, fatigue, nausea, vomiting and swollen lymph nodes.
Many infected people also show no symptoms at all (especially children).
Complications in dengue fever
In the majority of patients, dengue fever heals without any further consequences. In some cases, however, there are complications: Doctors differentiate between two serious disease courses that can also be life-threatening. They occur primarily in children and adolescents under the age of 15 and generally in patients who have already suffered from dengue:
Dengue hemorrhagic fever (DHF): In hemorrhagic dengue fever, an acute outbreak of fever is followed by symptoms caused by a sharp drop in blood platelets (thrombocytopenia). and bleeding gums and gastrointestinal bleeding (with vomiting blood and bloody stools).
Dengue shock syndrome (DSS): If the blood pressure derails due to the illness, the heart can no longer pump enough blood through the body. As a result, the heart rate rises sharply. Nevertheless, vital organs such as the brain and kidneys are no longer adequately supplied.
Warning signs of such complications are:
- sudden abdominal pain
- repeated vomiting
- sudden drop in body temperature below 36 ° C
- sudden bleeding
- Confusion, agitation, or lightheadedness
- sudden drop in blood pressure
- fast pulse
Both complications are potentially life threatening and require hospital treatment. The tricky thing: They usually only appear when the patient is already feeling better again, often between the third and seventh day of the illness. For this reason, one speaks of the critical phase in this context, as the course of the disease is now apparent and the doctor has to decide whether (drastic) countermeasures need to be taken.
Dengue fever: treatment
There is no causal therapy for this infection. This means that the doctor can only alleviate the symptoms, but not fight the virus itself.
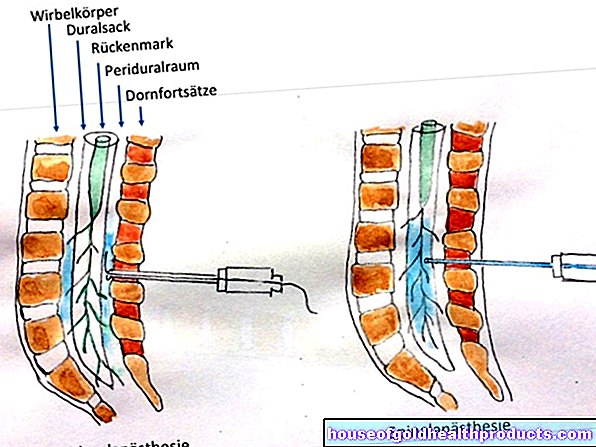
Dengue fever treatment does not differ significantly from flu treatment in the fever phase without complications: it is important to drink enough fluids. In addition, you can take a pain reliever and antipyretic drug such as paracetamol against the high fever and pain. Painkillers and fever medicines, which impair blood clotting and thus increase the bleeding tendency, are not suitable. These include above all acetylsalicylic acid (ASA), but also ibuprofen.
As long as there are no complications, the patient does not necessarily have to go to the hospital. However, as soon as signs of bleeding appear or a shock threatens, inpatient treatment (possibly in the intensive care unit) is unavoidable. The vital parameters (heart and respiratory rate, blood pressure, etc.) can be precisely monitored there. In addition, the patients are given infusions or blood reserves as needed.
The risk of complications is particularly high when the fever subsides. Any deterioration in health should then be reported to the doctor immediately.
Dengue fever: prevention
In October 2018, the European Medicines Agency (EMA) approved a vaccine against dengue for the European market. For most EU citizens, however, this approval does not matter. It is restricted to people who are nine to 45 years old, who live in an endemic area (e.g. La Réunion, Guadeloupe or French Polynesia) and who have ever suffered from dengue fever. The dengue vaccine is also not permitted as a travel vaccine.
Research has shown that people who have not had dengue fever and have been vaccinated have a slightly increased risk of developing serious dengue. That is why only people who have survived the infection receive the dengue vaccination.
According to the Robert Koch Institute, scientists are researching several other vaccines against dengue fever, some of them in clinical test phases. Until then, a few measures will help to prevent dengue fever in the first place. The most important thing is to protect yourself from mosquito bites when traveling to risk countries (exposure prophylaxis). The following protective measures are recommended:
- wear long trousers and long sleeves
- Apply repellents (mosquito sprays) to skin and clothing
- Stretch mosquito nets with a mesh size of no more than 1.2 mm - this corresponds to approx. 200 MESH (meshes / inch2) - over the bed
- Install fly screens on windows and doors (impregnated with insecticides)
If you are planning a trip to a dengue fever area, you should inform yourself carefully about the risks and protective measures before you travel. Travel doctors and tropical institutes offer appropriate advice.
Dengue fever: examinations and diagnosis
The main symptoms of dengue fever are indistinguishable from those of normal flu in the early stages. However, a specialist doctor such as a tropical doctor can often suspect an infection with "dengue fever" based on the symptoms described and the information that the person concerned was in a risk country. The doctor obtains such information in the initial consultation with the patient (anamnesis).
The physical exam is also important. It includes:
- Temperature, pulse and blood pressure measurement
- Listening to the sounds of your heart and lungs
- Palpation of the superficial lymph nodes
- Examination of the throat and mucous membranes
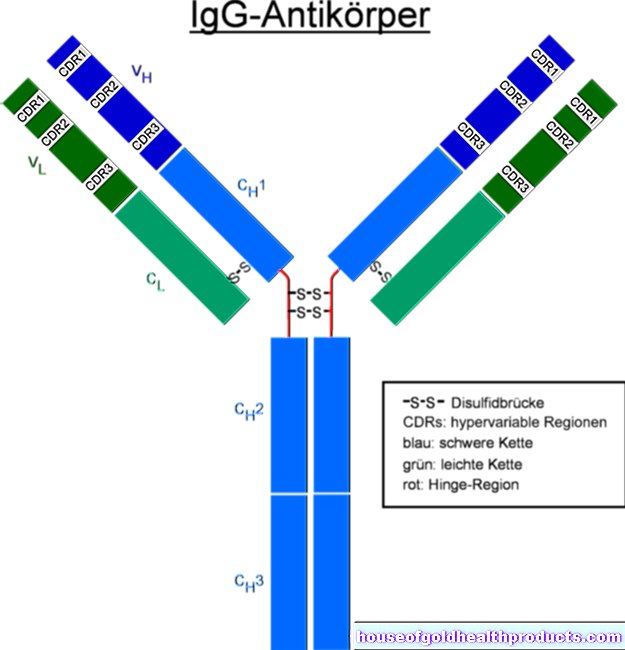
The suspicion of dengue fever can be confirmed by blood tests: A blood sample from the patient is examined for dengue viruses and specific antibodies against the pathogen. Rapid tests for the detection of specific antibodies are also available.
In addition, the doctor pays attention to signs of a tendency to bleed, for example in the form of bleeding gums, nosebleeds or small skin hemorrhages (petechiae). In this context, the so-called tourniquet test provides valuable information. It can be used to check the stability of the finest blood vessels (capillaries): To do this, a blood pressure cuff is placed on the patient's upper arm and inflated to a value between systolic and diastolic blood pressure. After about ten minutes, the cuff is removed and the doctor will check to see if there are any small hemorrhages (petechiae) on your forearm.
Dengue fever: disease course and prognosis
Dengue fever is usually uneventful. Most patients recover within a few days. However, the exhaustion can persist for a few more weeks.
There is an increased risk of complications in dengue fever in patients who do not drink enough or who are younger than 15 years. A second infection with dengue viruses is also dangerous:
After a dengue fever infection one is immune to the respective type of dengue virus for life. But you can get infected with one of the other three types of virus and get sick again. This second infection is often more serious (for example as dengue hemorrhagic fever). Experts suspect that an overreaction of the immune system is responsible for the more severe course of the disease. People who have already suffered from dengue fever must therefore be particularly careful when they return to the tropics.
Risk of death
In the case of dengue hemorrhagic fever (DHF) and dengue shock syndrome (DSS), timely intensive medical treatment is very important. The mortality (lethality) with DHF is between six and 30 percent. The DSS is even more dangerous: Without adequate treatment, 40 to 50 percent of patients die of this severe form of dengue fever. With timely therapy, however, the mortality drops to one percent or less.
Tags: alcohol drugs skin care sleep