Semen analysis
Dr. Manuela Mai studied medicine at the Universities of Heidelberg and Mannheim. After graduating, she gained clinical experience in gynecology, pathology and clinical pharmacology. She is particularly interested in the broader connections that lead to diseases - also outside of conventional medicine. She completed additional training in classical homeopathy as well as ear and skull acupuncture.
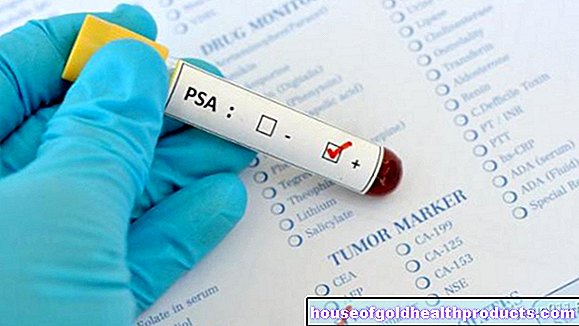
More about the experts All content is checked by medical journalists.A spermiogram (sperm examination) provides information about the quality of the sperm and thus about the man's fertility. The semen analysis is an important diagnostic aid when looking for the cause, especially when the desire to have children is unfulfilled. Here you can find out how a semen analysis is carried out and how the results are to be interpreted.

What is a semenogram?
A semen analysis provides information about the number, shape and mobility of the sperm in the ejaculate (semen). The pH value, sugar value, viscosity and bacterial colonization of the semen are also part of the semen analysis.
One possible reason for a semen examination is an unfulfilled desire to have children. If a couple tries unsuccessfully to have children for a long time, one of the reasons for this may be poor sperm count and / or quality. Both factors can be assessed using a semen analysis.
Another reason for a sperm test is to check if a vasectomy (sterilization of the man) was successful.
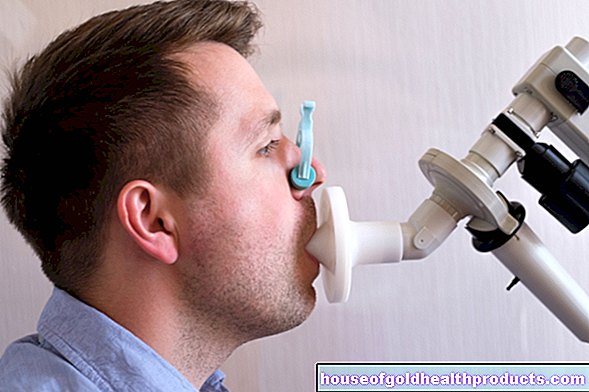
Spermiogram: procedure
If a man would like to have a spermiogram made, he seeks a urologist, andrologist (the male equivalent of the gynecologist) or a fertility clinic. There, the semen analysis is carried out in their own laboratory or delegated to an appropriate laboratory.
The semen is usually obtained by masturbation at the examination site. As a rule, the man has a quiet room available for this. For some men it is helpful if the partner helps with the collection of semen.
Some doctors also allow the semen sample to be generated at home. However, there is a higher risk that incorrect handling of the sample will impair the quality. For example, it is important that no lubricant is used when harvesting, as this reduces the mobility of the sperm cells. In addition, if possible, the entire ejaculate must be collected. The sample must then be transported in a sterile container at body temperature, for example in a trouser pocket. And: the sample should reach the laboratory a maximum of one hour after collection.
In addition to masturbation, there is also the option of collecting the sperm with the help of a condom during sexual intercourse. A sterile, spermicide-free and lubricant-free special condom must be used for this.
Sperm analysis waiting period
In order for the spermiogram values to be meaningful, the man must not have an ejaculation for three to five days before submitting the sperm sample. However, he must not abstain for more than seven days in advance, because this can also falsify the spermiogram result.
Sperm analysis in the laboratory
The actual evaluation of the sperm sample takes place in the laboratory. The relevant parameters are determined there, including volume, appearance, consistency and pH value. Healthy sperm, for example, becomes thin within a few minutes at room temperature and takes on a milky, gray-opal color.
The sperm itself is examined more closely under the microscope, examining its shape, activity and number. In addition, inflammatory factors can be searched for and an immunological examination and fructose measurement of the semen can be carried out.
Sperm analysis: WHO guideline values
When evaluating the sperm sample, the laboratories adhere to the requirements of the World Health Organization (WHO). The WHO guideline values for sperm analysis state, for example, that men are considered fertile if the concentration of sperm cells is at least 15 million sperm per milliliter of ejaculate. If the number is lower, it is called oligozoospermia. In some men who have not been surgically sterilized, there are even no sperm to be found in the ejaculate. Then there is a so-called azoospermia.
Other spermiogram norm values that serve as reference values are:
- 58 percent of sperm vital (living)
- Ejaculate volume at least 1.5 milliliters
- pH between 7 and 8
- Total sperm count in ejaculate at least 39 million
- a maximum of 1 million white blood cells per milliliter
- at least 13 µmol fructose in the ejaculate (important energy supplier for the sperm)
Sperm analysis: morphology and motility
In addition to the number of sperm cells, their quality is also decisive for a man's fertility. This is because the sperm must be able to swim to the egg cell. This does not work if they are impaired in their function, for example because they are deformed or poorly mobile. That would result in a bad semen analysis.
Three different areas are examined for the morphology of the sperm: the head, the midsection and the tail. There may be deviations in all three areas. For example, several tails can be created or the head containing the genetic information can be too small or too big. In fact, most sperm are not normally formed, so that, according to the WHO, the normal value is reached with four percent of healthy cells.
In addition, the sperm mobility is assessed in the spermiogram. A basic distinction is made here:
- fast forward movement (fast progressive)
- slow forward movement (progressive)
- swim in circles or only locally (not progressive)
- no movement (immotile)
The reference values here are that a total of 40 percent of the sperm cells should move at all (total motility) and of that a third (32 percent) should move progressively, i.e. in a targeted manner.
MAR test
Another criterion for the quality of the sperm is the so-called MAR test (mixed antiglobulin reaction test). For this purpose, the ejaculate is examined for sperm autoantibodies. These antibodies arise, for example, when the spermatic duct is injured on the inside. They stick to the sperm and make it harder for them to swim through the uterine mucus. As a guideline, therefore, is that only less than 50 percent of the sperm cells are allowed to carry such particles.
Bad semen analysis - what now?
The reasons for a poor semen analysis can be many. For example, previous or active infections (such as mumps, chlamydia), undescended testicles, hormonal disorders or genetic predispositions play a role. Sometimes the causes remain unclear. In the same way, incorrect determinations can also have occurred as a result of errors in handling (e.g. collecting sperm at home).
It is generally recommended to repeat the spermiogram after a few weeks if the findings are outside the normal spermiogram values. If the values still deviate, further diagnostic methods are used to find the cause of the poor semen analysis.
Improve semen analysis
There are a few things you can do to improve your semen analysis. Lifestyle is an important starting point. Affected men should, for example, stop smoking, lose weight if they are overweight or consume alcohol only in moderation. In some cases, hormonal treatment or surgery will help. If none of these attempts are fruitful, that does not mean that the desire to have children has to be buried. Medicine has several methods of artificial insemination available.
Ultimately, the semen analysis is a snapshot and will not always clearly state whether a man is fertile or not. Nevertheless, the spermiogram is an important element of the diagnosis when the desire to have children is unfulfilled.
Tags: Baby Child palliative medicine teenager