Green Star
and Lisa Vogel, medical editorJens Richter is editor-in-chief at Since July 2020, the doctor and journalist has also been responsible as COO for business operations and the strategic development of
More posts by Jens Richter
Lisa Vogel studied departmental journalism with a focus on medicine and biosciences at Ansbach University and deepened her journalistic knowledge in the master's degree in multimedia information and communication. This was followed by a traineeship in the editorial team. Since September 2020 she has been writing as a freelance journalist for
More posts by Lisa Vogel All content is checked by medical journalists.Green star (glaucoma) is a collective term for various eye diseases that damage the optic nerve and retina. Mostly people are affected after the age of 40, whereby the incidence of the disease increases with age. However, glaucoma can also be congenital. If left untreated, the disease leads to blindness. Here you can find out everything you need to know about the glaucoma.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. H42H40Q15
Brief overview
- What is glaucoma? Group of eye diseases which, in advanced stages, destroy the retina and the optic nerve and, if left untreated, can lead to blindness. Also called glaucoma.
- Symptoms: In the beginning there are usually hardly any symptoms, in the advanced stage visual field defects, eye pain, headache. In acute glaucoma (glaucoma attack) symptoms such as sudden visual disturbances, very hard eyeball, severe headache and eye pain, nausea.
- Cause: irreversible damage to the optic nerve, often (partly) caused by excessive intraocular pressure.
- Risk factors: e.g. old age, low blood pressure, high blood pressure, coronary artery disease (CHD), diabetes mellitus, increased blood lipids, migraines, tinnitus, severe myopia or farsightedness, cases of glaucoma in the family, dark skin color, smoking.
- Treatment: medication, possibly surgery.
- Prognosis: If left untreated, glaucoma leads to blindness.
Green star: description
The term "glaucoma" (glaucoma) describes a group of eye diseases which, at an advanced stage, damage the nerve cells of the light-sensitive retina and the optic nerve. The name of the disease has nothing to do with the bird world. It describes, on the one hand, the often observed (blue-) greenish shimmer of the iris in advanced glaucoma, and on the other hand the “staring gaze” when the eye is blind.
Glaucoma is one of the most common causes of blindness. In the industrialized nations, the diagnosis of “glaucoma” ranks third among the causes of blindness. It is estimated that around 14 million people have glaucoma in Europe. In many cases, those affected are unaware of their illness.
As soon as an affected person perceives the visual disturbances caused by glaucoma himself, the damage to the retina and / or optic nerve is often well advanced. And damage that has already occurred can usually no longer be reversed.
Glaucoma is more common as you get older. Seven to eight percent of people are affected over the age of 75, and even 10 to 15 percent after the age of 80.
Forms of glaucoma
Green star can come in different forms. On the one hand, a distinction is made between primary glaucomas - they occur independently, i.e. without an identifiable cause - and secondary glaucomas. The latter are the result of other diseases (eye disease or general disease), eye injuries, surgical interventions or certain medications.
On the other hand, depending on the anatomy of the chamber angle, glaucoma can be divided into the two main groups of open-angle glaucoma (wide-angle glaucoma) and narrow-angle glaucoma (angle block glaucoma).
Open-angle glaucoma
By far the most common form of glaucoma in the elderly is primary open-angle glaucoma - it is found in about nine out of ten people with glaucoma. This form of glaucoma is based on a drainage disorder in the so-called trabecular system (spongy tissue in the chamber angle), the cause of which is unknown. Because the aqueous humor cannot drain off well, the intraocular pressure increases. Primary open-angle glaucoma is chronic and affects both eyes.
Secondary open-angle glaucoma is less common. Here, the aqueous humor cannot flow well due to an obstruction within the trabecular network. This displacement can be caused, for example, by inflammatory cells, red blood cells or tumor cells, or it can be the result of cortisone therapy.
Angle-closure glaucoma
In narrow-angle glaucoma, the anterior chamber of the eye is so flat that the iris (iris) sharply narrows or even blocks the angle of the eye. This happens above all when the pupil is dilated in the dark or by the action of medication (or drugs) and the iris "unfolds" in the chamber angle. The drainage of the aqueous humor is thus hindered or even completely prevented.
Sometimes the cause of narrow-angle glaucoma - that is, the flattened anterior chamber - remains unknown (primary narrow-angle glaucoma). On the other hand, secondary narrow-angle glaucoma can be traced back to another eye disease, for example rubeosis iridis (pathological formation of new vessels in the iris due to insufficient local blood flow, e.g. in diabetes patients).
If this outflow disorder occurs acutely (seizure-like), one speaks of a glaucoma attack (also called "acute angle block"). The chamber angle is suddenly shifted. The intraocular pressure can then increase so much within a few hours that the retina and nerves are immediately and permanently damaged (risk of blindness!).
A glaucoma attack is an ophthalmological emergency that needs to be treated as quickly as possible!
Other forms of glaucoma
There are several other types of glaucoma. So-called normal pressure glaucoma (low pressure glaucoma) is not found in many glaucoma patients. With this special form of glaucoma, typical glaucoma changes occur in the eye despite normal intraocular pressure.
Congenital (congenital) glaucoma, on the other hand, is rare: in the affected babies, the trabecular system in the corner of the eye is not completely laid out for an unknown cause or the drainage of the aqueous humor is obstructed by persistent embryonic tissue. This form of glaucoma is noticeable in the first year of life and can lead to blindness relatively quickly.
Green star: symptoms
The symptoms of glaucoma vary depending on the form and stage of the disease.
Chronic glaucoma: symptoms
The vast majority of patients have chronically progressive glaucoma - most often primary open-angle glaucoma, and sometimes chronic narrow-angle glaucoma. In such cases, there are usually no symptoms in the early stages. Glaucoma patients often only notice their disease at an advanced stage based on increasing visual field defects (scotomas):
Due to the course of nerves and blood vessels, the visual field of the eye narrows in an arc shape from the outside in people with glaucoma. Typically this starts from the blind spot, i.e. the area of the retina where the optic nerve originates. This type of visual field loss is called Bjerrum's scotoma. As a result of this loss of field of vision, which progresses from the outside to the inside, those affected develop a "tunnel vision": They see well what is in front of them, while everything in the periphery of the field of vision (right, left, top and bottom from the center) becomes increasingly poor is no longer perceived.
Occasionally, visual field defects also occur in the center of the visual area.
Other symptoms of glaucoma can include eye redness, headache, and eye pain. In addition, if the intraocular pressure has been elevated for a long time, swelling (edema) of certain cells in the eye can lead to light refractions, which are perceived as colored rings or halos (auras) around bright light sources.
Acute glaucoma (glaucoma attack): symptoms
In acute narrow-angle glaucoma (glaucoma attack), the sudden sharp rise in intraocular pressure causes the following symptoms within a few hours:
- palpable hard eyeball
- severe eye pain and headache
- Eye redness
- colored halos around light sources
- reduced visual acuity
- Fixed, medium-sized pupil ("fixed" means that it hardly narrows or not at all when exposed to light)
- Nausea and vomiting
A glaucoma attack is a medical emergency - there is an acute risk of blindness! Therefore, the pressure in the eyeball must be reduced as quickly as possible. The family doctor can initiate the first treatment steps and then refer the patient to the ophthalmologist or to a clinic.
Congenital glaucoma: symptoms
If a baby has the following symptoms, congenital (congenital) glaucoma may be the cause:
- Enlargement of the eyeball and cornea (cow or ox eye, medical buphthalmus)
- enlarged corneal diameter
- Corneal opacity
- photosensitive eyes (photophobia)
- watery eyes
If you notice these signs in your child, you should definitely see a pediatrician! They can refer you and your child to a specialist.
Green star: causes and risk factors
As mentioned above, there are primary forms of glaucoma, the cause of which is unknown, and secondary forms of glaucoma, which may develop as a result of another disease or an eye injury.
The most important causes and risk factors for glaucoma at a glance:
- Deposits (plaques) that obstruct the trabecular structure in the chamber angle and the “Schlemm‘ canal” in the chamber angle (open-angle glaucoma). The deposits are mostly age-related.
- Insufficient perfusion pressure, i.e. insufficient pressure difference between the intraocular pressure and the pressure in the retinal vessels (see below). Triggers or risk factors for this are cardiovascular diseases such as coronary artery disease (CHD), heart failure, arteriosclerosis and peripheral arterial occlusive disease (PAD) of the carotid arteries or carotid arteries.
- low blood pressure or a very low second blood pressure value (diastolic blood pressure), e.g. due to heart valve defects or certain disorders of the vascular function
- chronic high blood pressure (hypertension), which damages the blood vessel wall
- Chronically high blood lipid levels (such as hypercholesterolaemia), which lead to deposits in the blood vessels (arteriosclerosis)
- Diabetes (diabetes mellitus) and other metabolic diseases that change the inner wall of blood vessels and impede blood flow
- Autoimmune diseases that involve blood vessels
- Smoking, as nicotine narrows blood vessels, including those in the eyes
- (Temporary) spasmodic vasoconstriction such as Raynaud's syndrome, migraine, tinnitus
- Severe inflammation on or in the eye, which can result in scarring or deposits in the corner of the chamber
- long-term cortisone treatment
- Pupil-dilating drugs when the eye chamber is already flat, because then the iris can block the chamber angle
- Severe nearsightedness or farsightedness beyond four diopters, in which the shape of the eyeball and the anterior chamber is changed
- Cases of glaucoma in the family
- dark skin color
Increased intraocular pressure
In many cases, glaucoma is associated with increased pressure in the eyeball (intraocular pressure). This occurs when the aqueous humor accumulates in the anterior chamber, for example as a result of an obstruction to drainage:
The aqueous humor is formed by special cells and released into the posterior chamber of the eye. From there it flows into the anterior chamber of the eye, where it is then drained off via the drainage system in the chamber angle. The constant exchange of aqueous humor is important for the function of the eye. The aqueous humor carries nutrients and oxygen to the lens and cornea, which do not have their own blood vessels. It also serves as an optical medium.
The decisive factor for the development of glaucoma is not the absolute pressure inside the eye, but the difference between intraocular pressure and the pressure in the blood vessels of the retina and the optic nerve, the so-called perfusion pressure. If the pressure inside the eye increases so much that it approaches or even exceeds the perfusion pressure, the fine blood vessels are literally clamped off - blood can no longer flow.
Intraocular pressure increased in only every second patient
Recent studies have shown that abnormally high intraocular pressure is actually measured in only around half of glaucoma patients. In the other 50 percent of those affected, however, intraocular pressure is in the normal range. Nevertheless, the blood flow is disturbed in them as well as a result of a disproportion between intraocular pressure and perfusion pressure. This disproportion is not based here on obstacles to the outflow of the aqueous humor (as in the case of increased intraocular pressure), but possibly on changes in the blood vessels or disorders of the general circulatory function.
Green star: examinations and diagnosis
Many glaucoma patients only go to the ophthalmologist when they notice the first signs of illness (such as visual disturbances). The disease is then more advanced. But even without such symptoms, you should have your eyes checked (and regularly) if you have risk factors for glaucoma (such as family glaucoma cases, narrow chamber angles, diabetes, Raynaud's syndrome).
A detailed doctor-patient discussion (anamnesis) forms the beginning of the doctor's visit. This is followed by various eye exams.
anamnese
The doctor can use the information from the anamnesis interview to collect your medical history. Possible questions from the doctor include, for example:
- Do you suffer from visual disturbances?
- Do you have circulatory problems?
- Are you aware of any underlying illnesses such as diabetes mellitus, migraines or high blood pressure?
- Have you injured your eye, for example in an accident or while doing sports?
- Do you take any medicine?
- Can you tolerate the prescribed funds?
- Are you taking the medication as directed by your doctor?
- Are there any eye diseases in the family?
Inspection of the eye
The anamnesis is followed by an inspection of the eye. The doctor looks at the eyelids, the cornea, the lens and the lacrimal system and looks for possible changes. For example, redness or purulent secretions can indicate certain diseases.
Slit lamp examination
The ophthalmologist uses a slit lamp to direct a sharply defined beam of light onto the eye. Depending on the bundling and direction of the light beam, different structures are visible or particularly emphasized. The microscope can then be used to detect even the finest changes, such as the cornea, the anterior chamber and the corner of the eye, the lens of the eye or the retina.
If glaucoma is suspected, the ophthalmologist assesses in particular the space available at the entrance to the anterior chamber and the depth of the anterior chamber. He also pays attention to changes in the iris and unusual pigmentation of the cornea.
The slit lamp examination takes place in a darkened room and is completely painless for the patient.
Intraocular pressure measurement (tonometry)
The pressure in the eyeball can be measured quickly with the so-called applanation tonometer. The measuring plate of the device presses from the front on the cornea of the eye (in the area of the pupil) and determines the pressure that is necessary to deform a defined area (applanation = flattening, flattening; tone = tension, pressure). Since the cornea of the eye is very sensitive to touch, it is numbed with a local anesthetic for the examination.
The unit of measurement for pressure in the eyeball is "millimeters of mercury" (mmHg) - the same unit that is used for blood pressure, for example. Normal values for intraocular pressure are between 10 and 21 mmHg. They can fluctuate by around five mmHg during the day, with the highest values occurring at night and in the early morning hours (therefore the time of day should always be documented when taking measurements).
Most people with glaucoma have intraocular pressure values above 21 mmHg, in extreme cases (glaucoma attack) sometimes even more than twice as high.
When measuring, the ophthalmologist will take into account that the pressure in the eye is often higher in older people without a glaucoma being present. In addition, the measurement result is also influenced by the thickness of the cornea, which should therefore be determined by a further examination (pachymetry - see below).
Controversial benefit
The benefit of intraocular pressure measurement in glaucoma diagnosis is, however, controversial. The intraocular pressure is not increased in every glaucoma patient. A glaucoma can also be present with normal measurement results. The benefits and risks of the examination must be weighed up on a case-by-case basis and discussed with the ophthalmologist.
Measurement of corneal thickness (pachymetry)
The thickness of the cornea is different in every person. It can be between approximately 450 and 650 micrometers (thousandths of a millimeter). The corneal thickness is measured either selectively with ultrasound or light - or a thickness profile is created over the entire corneal surface:
For this purpose, the entire anterior and posterior surface of the cornea is imaged with a slit-shaped light beam and captured by a high-resolution camera. A computer program uses these images to calculate the thickness at thousands of individual points and ultimately reconstructs a high-precision thickness profile.
Ophthalmoscopy (fundoscopy)
The ophthalmoscopy (funduscopy, ophthalmoscopy) is particularly informative for the diagnosis of "glaucoma" because it allows glaucoma damage and the stage of the disease to be made directly visible:
With the help of an ophthalmoscope - a mixture of magnifying glass and light source - the ophthalmologist assesses the condition of the retina, its blood vessels and the head of the optic nerve. Shortly before the examination, the patient is given special eye drops that dilate the pupil so that the doctor can view the largest possible section of the fundus.
Examination of the chamber angle (gonioscopy)
If the suspected diagnosis is “glaucoma”, the angle of the chamber is examined by means of gonioscopy. Due to its peripheral location in the anterior eyeball, this is usually not visible from the outside. The gonioscope, however, has a special lens with which the ophthalmologist can "see around the corner" as it were. To do this, he places the gonioscope directly on the previously locally anesthetized cornea.
In narrow-angle glaucoma, there is a shallow chamber angle. In open-angle glaucoma, for example, drainage blockages through the iris and possible age-related plaques can be recognized. Adhesions and discoloration can also indicate glaucoma.
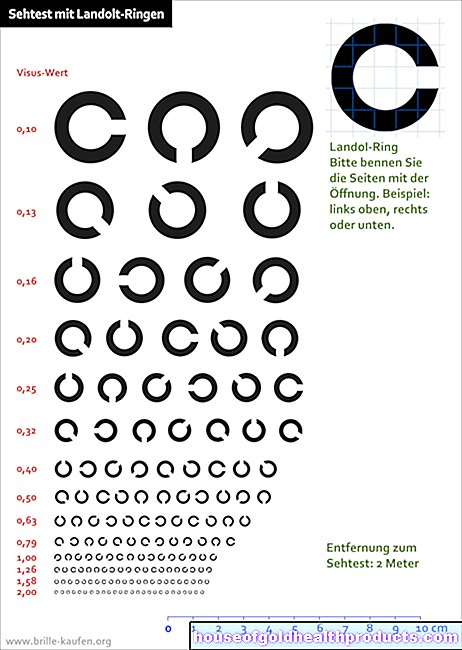
Field of view measurement (perimetry)
An important examination for the detection of existing retinal or nerve damage is the field of view measurement (perimetry). It is carried out individually for each eye (while the other is covered).
During the examination, the patient is presented with optical stimuli one after the other at different locations in the room, without being allowed to look directly at them. If he perceives a light stimulus, he has to indicate this with the push of a button. Thus, the size of the visual field and any visual field defects (scotomas) can be determined, as they occur in glaucoma.
Glaucoma is not the only cause of reduced field of view. In addition, scotomas usually appear late in glaucoma - when more than 30 percent of the nerve fibers are damaged.
Measurement of blood flow
Various tests can determine the flow of blood to the retina and optic nerve. Frequently used methods are fluorescence angiography (X-ray contrast examination of the blood vessels in the eye), thermography (recording of the heat given off by the eyeball as a measure of blood flow) and capillary microscopy (magnification of the finest blood vessels in the retina).
Since the relationship between intraocular pressure and the pressure in the blood vessels of the eye is incorrect in glaucoma, blood pressure measurement is also part of the routine examinations.
Green star: treatment
Once the diagnosis of "glaucoma" has been made, treatment should be started as soon as possible in order to prevent possible (further) damage to the eyes. There are various treatment options available for this. Many people with glaucoma need to have their intraocular pressure lowered - with medication and / or surgery. This can prevent the progression of glaucoma and at least slow it down.
In secondary glaucoma, the underlying cause (e.g. another eye disease or a disease affecting the whole body such as diabetes) must also be treated if possible.
Lowering of intraocular pressure
The aim of glaucoma treatment is to permanently lower the elevated intraocular pressure below a critical value so that enough blood can flow again to the cells of the retina and the optic nerve. This "critical intraocular pressure" varies from person to person. It depends on the mean pressure at which the blood circulates in the blood vessels of the eyeball (perfusion pressure):
It is important that the pressure in the eyeball is well below the perfusion pressure so that there is not too much resistance to the blood flow. Ophthalmologists also call the desired value for intraocular pressure "target pressure". In order to determine this individual target pressure, especially at the beginning of glaucoma treatment, it is necessary to closely monitor intraocular pressure, blood pressure and blood flow to the retina and optic nerve head. In principle, the ophthalmologist uses the same procedures for diagnosing glaucoma. The check-ups are also important because glaucoma can get worse over time. In this case, the therapy must be adjusted.
The lowering of the intraocular pressure to below the individual target value can often be achieved with medication, but sometimes glaucoma surgery is also necessary. That depends on the cause and the course of the disease.
Green star: medication
Not all forms of glaucoma can be treated satisfactorily with medication. In the most common form of glaucoma, primary open-angle glaucoma, drug treatment is often sufficient.
The patients here usually receive special eye drops that have to be used once or several times a day. The drops contain active ingredients that are intended to lower the intraocular pressure below the individual target value - by reducing the production of the aqueous humor and / or improving the outflow of the aqueous humor:
- Beta blockers: They are also prescribed for high blood pressure, heart failure and coronary heart disease, among other things. Used as eye drops, they can lower the production of aqueous humor.
- Carbonic anhydrase inhibitors (e.g. dorzolamide, brinzolamide): They also reduce the formation of aqueous humor. Usually they are used as eye drops. In the case of an acute attack of glaucoma, it can also be injected directly into a vein so that it takes effect more quickly.
- Sympathomimetics: They can also reduce the production of aqueous humor.
- Alpha agonists: They can both reduce the production of aqueous humor and increase its outflow.
- Prostaglandins: They ensure that the aqueous humor can drain off better. As a side effect, the color of the iris can become darker.
- Cholinergics: They too improve the outflow of aqueous humor.
- Parasympathomimetics: They constrict the pupil (miosis), thereby widening the angle of the chamber and making it easier for the aqueous humor to drain away. Unpleasant side effect: the narrowing of the pupil, especially older people, restrict their eyesight.
The doctor can also combine various active ingredients in order to increase the success of therapy for glaucoma.
Which medication is ultimately prescribed in which dosage depends primarily on the type of glaucoma to be treated. In any case, it is important that the doctor and glaucoma patient work well together and that the patient consistently adheres to therapy.
Green star: surgical interventions
Surgery is required when drugs used to treat glaucoma fail to reduce intraocular pressure adequately and reliably. Sometimes drug and surgical glaucoma therapy are also combined.
In the case of a glaucoma attack, for example, medication is first used to relieve pressure and only then is the eye operated on. In the early childhood form of glaucoma (primary congenital glaucoma), on the other hand, glaucoma surgery is performed as early as possible.
The following procedures are available for surgical glaucoma treatment:
Trabeculectomy / trabeculotomy
In this method, the aqueous humor is drained from the anterior chamber by placing an artificial drainage system. The aqueous humor can seep out from the anterior chamber of the eye to the conjunctiva; there it is drained off via the large vessels of the conjunctiva.
The operation is performed under local anesthesia and can often also be performed on an outpatient basis. The procedure takes about 30 minutes.
Iridectomy and laser iridotomy
The iris is opened by a small incision - either with a fine knife or a laser. The aqueous humor can pass through the small hole directly from the posterior chamber into the anterior chamber, where it then flows off via a canal.
This procedure is useful if you have narrow-angle glaucoma and there is a risk of angular block (glaucoma attack). It is performed under local anesthesia.
Laser trabeculoplasty
The sponge-like tissue in the chamber angle (trabecular structure) is bombarded with laser beams, which improves the drainage of the aqueous humor. The method is mainly used in patients with open-angle glaucoma. Ideally, this can lower the pressure in the eye by around eight millimeters of mercury (mmHg).
The procedure is performed under local anesthesia and the patient can go home immediately after the treatment. However, the effect of laser therapy on glaucoma is often not permanent.
Cyclophotocoagulation / Cyclocryocoagulation
The focus of the surgical procedure here is the ciliary body - a ring-shaped part of the middle skin of the eye to which the eye lens is "suspended" and which is involved in the production of the aqueous humor.
During the procedure, the ciliary body is destroyed with a laser (cyclophotocoagulation) or cold stick (cyclocryocoagulation) in the area that forms the aqueous humor - the amount of aqueous humor that is formed decreases, which lowers the intraocular pressure.
Both glaucoma treatment can be used for secondary glaucoma and glaucoma where other surgeries are unsuccessful.
Opening of Schlemm's Canal
Schlemm's canal plays a major role in draining the aqueous humor. During the procedure, the surgeon locates the canal with a probe and then creates an opening to the anterior chamber from there. This improves the drainage of the aqueous humor.
This glaucoma operation is performed on congenital glaucoma (congenital glaucoma).
Regular check-ups
An important part of glaucoma treatment is regular check-ups with an ophthalmologist. One to three check-ups per year are useful - depending on how far the green star has already progressed.
Green star: disease course and prognosis
Without treatment, glaucoma leads to blindness because it continues to damage the visual cells of the retina and the optic nerves. The course of the disease accelerates the longer the glaucoma has existed. Damage that has occurred once cannot be reversed.
It is all the more important to detect glaucoma early, avoid risk factors and consistently continue treatment.The good news: With suitable medication and / or surgery, glaucoma can usually be stopped and eyesight preserved.
Tags: interview womenshealth Diagnosis