Rheumatoid arthritis
and Sabrina Kempe, medical editorMareike Müller is a freelance writer in the medical department and assistant doctor for neurosurgery in Düsseldorf. She studied human medicine in Magdeburg and gained a lot of practical medical experience during her stays abroad on four different continents.
More about the expertsSabrina Kempe is a freelance writer for the medical team. She studied biology, specializing in molecular biology, human genetics and pharmacology. After her training as a medical editor in a renowned specialist publisher, she was responsible for specialist journals and a patient magazine. Now she writes articles on medical and scientific topics for experts and laypeople and edits scientific articles by doctors.
More about the experts All content is checked by medical journalists.
Rheumatoid arthritis (rheumatoid arthritis, primary rheumatoid arthritis) is an inflammatory joint disease that progresses in phases. Anyone can be affected. Patients suffer from swollen, painful and deformed joints, especially in the fingers and hands. With consistent drug therapy, complications of the disease can be prevented in many cases. Read everything you need to know about rheumatoid arthritis here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. M08M05M06
Brief overview
- What is Rheumatoid Arthritis (RA)? A non-contagious, chronic, relapsing inflammation throughout the body.
- Symptoms: initially unspecific (e.g. fatigue, slight fever, heaviness in the muscles), followed by swelling and tearing pains first in small joints (hands, feet), later also in larger ones (e.g. knees), morning stiffness, limited mobility
- Causes: RA is an autoimmune disease - the immune system attacks the body's own tissue. The cause is unclear; Hereditary factors and risk factors such as smoking, obesity and infections are discussed.
- Treatment: medication, invasive therapy (e.g. artificial joint), physiotherapy (such as massages, thermotherapy, electrotherapy), occupational therapy and rehabilitation, healthy nutrition, possibly psychotherapy
- Prognosis: RA is incurable. With the right, lifelong therapy, however, the disease can calm down (remission). If left untreated, however, cartilage, bones and connective tissue are increasingly destroyed.
Rheumatoid arthritis: definition
The term "rheumatoid arthritis" means "joint inflammation that belongs to the rheumatic type". In the past, the disease was also known as (primary) chronic polyarthritis (poly = many, arthritis = joint inflammation).
However, rheumatoid arthritis is a systemic (i.e., affecting the whole body) inflammation. It is long-lasting (chronic) and in many patients it progresses in relapses. Rheumatic symptoms are particularly evident in the small joints of the hands and feet.
Rheumatoid Arthritis: Who Does It Affect?
Rheumatoid arthritis is the most common inflammatory joint disease in the world. Around 550,000 people are affected in Germany. Around two thirds of the patients are female. Although rheumatoid arthritis can occur at any age, most patients are between 50 and 70 years old when the disease breaks out.
The variant "juvenile idiopathic arthritis" (see below) occurs in about 0.1 percent of the under 18 year olds, ie in about 13,000 children and adolescents. This form of rheumatoid arthritis is one of the most common chronic diseases in minors.
Ten percent of all RA patients have a first-degree relative (such as a parent) who also has rheumatoid arthritis. The probability that both identical twins will fall ill is around 15 to 20 percent.
Rheumatoid arthritis: special forms
There are some particular forms of rheumatoid arthritis:
Caplan syndrome: Rheumatoid arthritis in combination with quartz dust lung (silicosis). Doctors also speak of silicoarthritis here. Caplan syndrome typically occurs in coal-mining workers.
Felty syndrome: Felty syndrome is a severe form of rheumatoid arthritis that predominantly affects men. In addition to the inflammation of the joints, the spleen is swollen and the number of white blood cells (leukocytes) and platelets (thrombocytes) is reduced.
Elderly rheumatoid arthritis (late onset rheumatid arthritis, LORA): Elderly rheumatoid arthritis is a common disease. It does not break out until after the age of 60 and often affects only one or a few large joints. In addition, there are often general symptoms such as fever, poor performance, weight loss and muscle wasting.
Juvenile Idiopathic Arthritis: Also called Juvenile Rheumatoid Arthritis. The addition "juvenile" shows that this form of rheumatoid arthritis affects young people (children, adolescents). The cause of the disease is usually unclear. It is assumed that a - partially undetected - bacterial infection strongly activates the immune system in those affected.As a result, the body's own tissue is destroyed (autoimmune reaction).
Systemic arthritis: It is a subtype of juvenile idiopathic arthritis. In addition to joint pain, attacks of fever occur here. Often a blotchy rash and lymph node swelling also develop. The disease also affects other organ systems such as the liver or spleen. This rare disease also occurs in adults, and is then referred to as Still's disease.
Rheumatoid arthritis: symptoms
Rheumatoid arthritis begins with unspecific symptoms such as
- Exhaustion
- slight fever
- Muscle heaviness
- fatigue
- Loss of appetite
- depression
Many patients then initially think of a flu-like infection or a sports injury. Typical rheumatoid arthritis symptoms only appear in the further course. This includes swelling and pulling, tearing (rheumatic) pain in the small joints on the fingers and feet. As a rule, both hands or feet are affected at the same time (symmetrical infestation). A strong handshake in particular causes severe pain in the patient (Gaenslen's sign).
In addition, the joints feel stiff in the morning. This morning stiffness lasts for more than half an hour and is associated with restricted mobility and weakness. For example, those affected suddenly find it difficult to hold a coffee cup.
Rheumatoid arthritis of the hand can also lead to circulatory disorders in individual fingers.
Later, larger joints towards the middle of the body can also be affected, for example elbows, shoulder and knee joints or the upper cervical spine. Rheumatoid arthritis, on the other hand, does not normally make itself felt in the end joints of the fingers (distal interphalangeal joints, DIPs) or in the thoracic and lumbar spine.
If you have joint swelling and pain, see a doctor as soon as possible! If rheumatoid arthritis is recognized in the first six months and treated immediately, the joints are most likely to be saved from destruction.
More Rheumatoid Arthritis Symptoms
Rheumatoid arthritis can attack other structures in addition to the joints. In this way, the following can arise:
- Carpal tunnel syndrome: constriction of the middle arm nerve (nervus medianus) on the wrist due to thickened, inflamed tendon sheaths
- Sulcus ulnaris syndrome: irritation of the ulnar nerve on the elbow
- Baker's cyst: An accumulation of fluid in the hollow of the knee that can affect bending
- Rheumatoid nodules: nodular structures that form in the subcutaneous fatty tissue along the tendons or at pressure points
- Sicca syndrome (secondary Sjogren's syndrome): dysfunction of the salivary and lacrimal glands
Rheumatoid arthritis: organ manifestations
Rheumatoid arthritis can also affect the internal organs. Possible consequences are:
- Heart valve changes
- Inflammation of the lung (pleurisy)
- connective tissue remodeling of the liver (liver fibrosis)
- Inflammation of the kidneys (glomerulonephritis)
Rheumatoid arthritis: causes and risk factors
The exact cause of rheumatoid arthritis is still unknown. There are, however, various theories about how the disease develops.
For one, genetic factors seem to have an influence. This is supported by the fact that rheumatoid arthritis occurs frequently in families.
In addition, many patients have something in common in the so-called HLA genes. HLA stands for "Human Leukocyte Antigen". The HLA proteins mark cells as endogenous or foreign. The immune system knows which cells (foreign ones) should be attacked and which should not (the body's own). However, certain changes in the HLA genes can lead to this distinction no longer working and the immune system attacking the body's own structures (autoimmune reaction). This is how rheumatoid arthritis can develop, experts suggest.
Studies have shown that around 70 percent of rheumatoid arthritis patients carry the HLA gene DR4 / DRB1. In the healthy population, only about 25 percent of people have this gene variant.
Another possible cause of rheumatoid arthritis are environmental influences in the sense of infections and allergies. Pathogens such as herpes or rubella viruses may trigger the disease. Smoking and being overweight can also contribute to the onset of the disease if other risk factors are present.
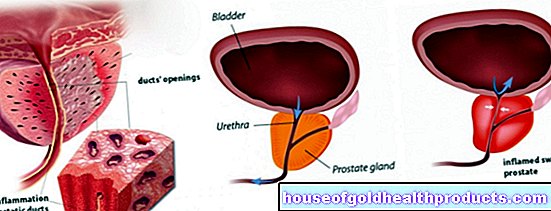
Rheumatoid arthritis: gradual joint destruction
Joints are surrounded by a joint capsule. The inner layer of the joint capsule is covered with the joint mucous membrane (also called the synovial membrane or synovium). This synovial membrane produces the synovial fluid to lubricate the joint.
The immune system of people with rheumatoid arthritis makes antibodies against their own synovial membrane (autoantibodies). It then becomes chronically inflamed and thickens. Now other inflammatory substances are released. These mediators (for example TNF-α or interleukin-1) cause the inflammation to flare up again. They ensure that further immune cells immigrate and that a so-called pannus is created through an increase in connective tissue cells. It overgrows and destroys the articular cartilage and can also grow into the bone below.
In addition to the inflammation of the synovial membrane, joint inflammation (arthritis), bursitis (bursitis) and tendinitis (tendovaginitis) gradually develop. Ultimately, it comes to misalignments and so-called ankyloses (stiffening of the joints).
Rheumatoid arthritis: treatment
The motto for rheumatoid arthritis therapy is “hit hard and early”. In this way, the inflammation can be suppressed sustainably in many cases and thus the threatened destruction of the joint can be prevented or at least delayed for a long time. Treatment should be started as early as the first three months after the onset of symptoms. Then it is most effective.
There are several drugs that are used to treat rheumatoid arthritis. In addition, there are supportive measures such as physiotherapy, heat therapy, relaxation therapy or alternative healing methods. However, the need for drug therapy is undisputed.
Careful therapy planning
Rheumatoid arthritis is individual in each patient. Therefore, your doctor will tailor the therapy to your needs as best he can. However, this will only work if you and your doctor speak openly to each other and make therapy decisions together. The following questions could be important to you and should therefore be discussed with your rheumatologist:
- What result can be expected from the treatment?
- What side effects and complications can occur?
- How long is the treatment expected to last?
- Can I follow my normal lifestyle during the treatment?
- Are the medication compatible with the medication I am already taking (e.g. for high blood pressure, etc.)?
If you did not understand something when talking to your doctor, then ask. A few days to think about it or a second opinion can also be useful if you are unsure. Rheumatoid arthritis therapy is a comprehensive and long-term measure that should be optimally planned.
Six weeks after the start of treatment, the tolerance and correctness of the dosage of your medication should be checked in a first control appointment. Another three months later, disease activity should have halved. After six months, thanks to the medication, almost complete freedom from inflammation and symptoms (remission) should be achieved. If this is not the case for you, your rheumatologist should adjust the therapy.
Rheumatoid arthritis: drug therapy
There are several medicines available for rheumatoid arthritis. A distinction is made between so-called basic therapeutic agents ("disease modifying antirheumatic drugs", DMARD), glucocorticoids and non-steroidal anti-inflammatory drugs (NSAIDs):
- DMARDs are disease-modifying drugs - they modulate the excessive immune reaction and can thus slow down or even stop the course of the disease. The symptoms then recede and the joints are protected from further destruction as far as possible.
- Glucocorticoids ("cortisone") are anti-inflammatory hormones and are also naturally produced in the adrenal cortex. They are particularly effective when administered as medication for rheumatoid arthritis and can help against joint damage caused by disease.
- NSAIDs (e.g. diclofenac, ibuprofen, naproxen, indomethacin) relieve pain in the acute episode and are sometimes also anti-inflammatory.
Therapy start
At the beginning of the disease, the most important representative of the conventional synthetic DMARD (csDMARD) is given: methotrexate (MTX). This active ingredient has been studied most intensively so far.
Methotrexate may not be given in some patients - due to comorbidities, drug interactions or intolerance. Therapy for rheumatoid arthritis can then also be started with the active ingredients leflunomide or sulfasalazine. These substances also belong to the csDMARDs and are as effective as MTX.
Since it takes several weeks for the csDMARDs to take full effect, the doctor will also prescribe anti-inflammatory glucocorticoids (cortisone) at the beginning of the therapy. Your doctor can also inject the glucocorticoids directly into particularly severely affected joints.
Due to their strong side effects, glucocorticoids are not suitable as long-term basic therapy. Your rheumatologist will therefore significantly reduce the starting dose (10 to 30 mg prednisolone per day) within eight weeks. After three to six months, you can ideally do without glucocorticoids altogether.
Tip: Take cortisone tablets early in the morning. At this time, the body itself is also making the anti-inflammatory hormone. With the morning intake you follow your body's natural production rhythm.
Initially, you can suppress pain and morning stiffness with NSAIDs. However, these drugs are also unsuitable for long-term use due to their side effects. Therefore, if you respond well to DMARD treatment, you can stop taking NSAIDs.
Further therapy
If no effect can be determined twelve weeks after the start of treatment, you must decide on a new treatment strategy together with your doctor. If your rheumatoid arthritis progresses easily and the prospects of getting the disease under control are good, other conventional DMARDs are used together with MTX - either the three-way combination with sulfsalazine and hydroxychloroquine (antimalarial agent) or the two-way combination with leflunomide.
If the (adapted) drug therapy could not contain the rheumatoid arthritis successfully even after six months, you will receive biological DMARDs - also called Biologica (Biologicals) - or targeted synthetic DMARDs ("targeted synthetic Disease Modifying Anti-Rheumatic Drug", abbreviated tsDMARD) ). If possible, these are combined with MTX. You will also be given such medication if your disease becomes more severe and after three months there has not been sufficient improvement or the treatment goal has not yet been achieved after six months.
>>> Biologics are biotechnologically produced proteins that intervene in the body's immunological processes. They intercept inflammatory messenger substances in the blood. They include:
- TNF-α inhibitors (adalimumab, etanercept, infliximab, certolizumab, golimumab)
- T-cell activation inhibitor (abatacept)
- Interleukin-6 receptor antibodies (tocilizumab, sarilumab)
- B-cell antibodies (rituximab)
- Interleukin-1 competitor (anakinra)
If the patent protection for one of these original biologics has expired, similar biotechnologically manufactured drugs (so-called biosimilars) can also be given. According to the medical guidelines for rheumatoid arthritis, these can be used in the same way as the original biologics.
>>> Targeted synthetic DMARDs are the newest subgroup of base medications for rheumatoid arthritis. In contrast to biologics, they are not produced biotechnologically but, like conventional DMARDs, synthetically.
The active ingredients specifically inhibit a certain molecule within the cells and thereby interrupt an inflammation-promoting signal path that is partly responsible for the development of rheumatoid arthritis. So far, the Janus kinase (JAK) inhibitors baricitinib and tofacitinib have been approved for the treatment of rheumatoid arthritis from this group of drugs.
Which active ingredients work best differs from patient to patient. Once the right medication has been found, the dose is gradually reduced after a disease flare-up has subsided. The aim is to determine the so-called maintenance dose - the dose that is high enough to keep rheumatoid arthritis in check, but at the same time so low that the side effects are still acceptable.
Therapy control
From the time of diagnosis, your rheumatoid arthritis should be assessed and documented by your rheumatologist every three months with regard to disease activity and course. To do this, the doctor uses various scoring systems such as:
- Disease Activity Score of 28 joints (DAS28)
- Clinical Disease Activity Index (CDAI)
- Simplified Disease Activity Index (SDAI)
These systems can be used to assess how well you are responding to the therapy or whether it should be adjusted based on the number of painful and swollen joints, your condition and, if applicable, your inflammation values.
Rheumatoid arthritis: side effects of the drugs
All of the active ingredients mentioned can have side effects. These depend on the dose and also vary from patient to patient - some people suffer more from them than others. In the following table you will find MS drugs with the type of application (mostly orally, e.g. as a tablet) and the most important side effects
|
Active ingredient |
type of application |
Important side effects |
|
Methotrexate (MTX) |
orally |
Changes in the blood count, kidney and liver damage, gastrointestinal complaints, headache, skin rash |
|
TNF-alpha inhibitors |
Infusion or syringe under the skin |
Infections, administration site pain, infusion reactions, abdominal pain, nausea, vomiting, headache, low white blood cell count, increased blood lipid levels |
|
Interleukin-6 inhibitors (tocilizumab, sarilumab) |
intravenously (infusion, syringe) or syringe under the skin |
Upper respiratory tract infections (with cough, nasal congestion, sore throat and headache), infusion reactions (with fever, chills, fatigue) |
|
B-cell antibodies (rituximab) |
Infusion (combined with MTX) |
Infections, allergic reactions, changes in blood pressure, nausea, rash, itching, fever, runny or blocked noses and sneezing, tremors, accelerated heartbeat and tiredness, headaches, changes in laboratory values, infusion reactions (with fever, chills, fatigue) |
|
Interleukin-1 competitor (anakinra) |
Syringe under the skin |
Headache, injection site reaction, high cholesterol level |
|
JAK inhibitors |
orally |
Upper respiratory tract infections, headache, diarrhea |
|
NSAIDs |
orally |
Gastrointestinal complaints (such as nausea, vomiting, diarrhea, gastrointestinal bleeding), kidney dysfunction, water retention in the legs, central nervous disorders (such as hearing or visual disturbances, ringing in the ears, dizziness, headache, tiredness) |
|
Glucocorticoids |
mostly oral |
including osteoporosis, increased risk of infection, high blood pressure, psychological or neurological disorders, growth disorders in children |
During pregnancy, rheumatoid arthritis should only be treated with cyclosporine, azathioprine and sulfsalazine in order not to endanger the unborn child. In addition, MTX and leflunomide should be discontinued months before a planned pregnancy.
Rheumatoid Arthritis: Invasive Therapy
Rheumatoid arthritis can also be treated with invasive therapy, i.e. with measures that involve an intervention in the body. This includes:
- Joint puncture: If there is an effusion in the affected joint, this can be punctured to drain the fluid and thus alleviate the discomfort.
- Radiosynoviorthesis (RSO): Here radioactive substances are introduced into severely inflamed joints. In this way, pain relief can be achieved in individual joints after a few months.
- Synovectomy: In this operation, the joint mucous membrane (synovium) is removed, which makes a decisive contribution to the symptoms of rheumatoid arthritis.
- Joint replacement: If a joint has been destroyed by rheumatoid arthritis, it may be possible to replace it with a prosthesis.
With all invasive methods, strict adherence to the hygienic regulations must be observed, as joints can easily become infected.
Rheumatoid Arthritis: Physiotherapy
Rheumatoid arthritis should not only be treated with medication, but also with physiotherapy. This can:
- improve joint mobility
- strengthen or relax the muscles
- Prevent malpositions
- reduce pain
Physiotherapy includes various methods and techniques:
Special movements in manual therapy (manual therapy) can release joint blockages and restore mobility. Massages help against muscle tension.
Thermotherapy is also suitable for rheumatoid arthritis:
- Cold applications help relieve pain and reduce inflammation during periods of acute inflammation.
- The application of heat can be useful in phases of remission (temporary relief of symptoms) in order to stimulate the metabolism and promote blood circulation. This can relieve tension.
If you have a cardiovascular disease (such as high blood pressure, heart failure), you should avoid thermotherapy.
Direct currents and alternating currents in electrotherapy are also suitable for the supportive treatment of rheumatoid arthritis. They have different effects in different frequencies:
- A low-frequency therapy has pain-relieving and blood circulation-promoting properties.
- Medium frequency therapy strengthens the muscles.
- The high-frequency therapy is a heat treatment with a deep effect.
If you have a pacemaker and / or metal implants (such as a joint replacement), you are not allowed to receive electricity or only with restrictions.
Rheumatoid arthritis: occupational therapy and rehabilitation
If rheumatoid arthritis becomes severe, you will need to adapt your lifestyle to the disease. As part of occupational therapy and rehabilitation, you can practice activities of everyday life (at home, at work and in your free time) in order to maintain your independence (occupational therapy) or restore it (rehabilitation). For example, you can practice opening drinks bottles with as little stress as possible, handling cutlery, getting up and getting dressed.
Rheumatoid Arthritis: Alternative Medicine
Alternative medicine such as homeopathy or traditional Chinese medicine (TCM) are also often used by patients in addition to medicinal treatment. Naturopathy is also popular: there are several plants that can alleviate the symptoms of rheumatoid arthritis. These include:
- Nettle (anti-inflammatory, analgesic)
- Willow bark (relieves pain, reduces fever)
- Devil's Claw (anti-inflammatory, analgesic)
- Frankincense (anti-inflammatory)
Always discuss alternative therapies with your rheumatologist. These methods can only complement and support the drug treatment of rheumatoid arthritis, but not replace it.
Rheumatoid Arthritis: Psychological Support
Psychological support can reduce pain, stress and disabilities in everyday life and improve your quality of life. Your psychotherapist can recommend relaxation techniques such as Jacobson's progressive muscle relaxation or autogenic training. In order to be able to deal with the complaints better, he will also provide you with pain, illness and stress management programs if necessary.
Rheumatoid Arthritis: Remedies
In order to cope better with the disease in everyday life, there are various aids, the costs of which are often covered by the health insurance company for rheumatoid arthritis:
Orthopedic shoes and insoles: metatarsal, ball of the foot or toe rolls provide support and ensure that the pressure is better distributed. Heel wedges support the shortened foot at the back. Custom-made shoes adapt to the changed shape of the foot. Soft insoles or walking soles have a pleasant cushioning effect.
Splints with and without joints: Supporting splints or bandages maintain the mobility of the joint and take away excessive pressure. There are also movable rails that use hinges to secure the direction and extent of movement of the joints. Immobilizing splints are also available that immobilize a joint overnight or in the event of acute pain.
Walking aids: Depending on the degree of walking disability, a simple walking stick with or without a special handle, a forearm crutch or an armpit crutch will help. They provide the necessary security when walking. A so-called rollator can also be helpful in the case of particularly pronounced walking difficulties. This is a walker with brakes, a seat board and small storage space, which enables longer journeys or independent shopping.
Special aids: Raised toilet seats, grab bars, shower wheelchairs and bathtub lifts facilitate thorough body hygiene without outside help, even with severe mobility restrictions - an important prerequisite for a good quality of life.
Rheumatoid Arthritis: What Can You Do By Yourself?
With rheumatoid arthritis, you don't just have to rely on others for your wellbeing and disease management. You can also take action yourself:
Patient education
In a patient training course, you will get to know your disease better. You will also learn how to better cope with the illness, the pain that goes with it and the stress it causes. The more informed you are, the easier it is for you and your doctor to make decisions about treatment. The German Society for Rheumatology has developed such patient training courses in cooperation with the German Rheumatism League.
Support groups
Rheumatoid arthritis is easier to manage together. Therefore, if possible, you should join a self-help group for rheumatism sufferers. The exchange with other affected persons can be very valuable and helpful! You can find information, for example, at: www.rheuma-liga.de.
Sport and smoking cessation
Painful joints often prevent the desire to exercise in rheumatoid arthritis. You should still do sport regularly: Endurance sport helps you to feel better and to keep your body fit. This is how you can prevent painful muscle tension.
In addition, you shouldn't smoke (anymore). Not using nicotine can have a positive effect on the course of rheumatoid arthritis.
nourishment
Diet is also an important issue in rheumatoid arthritis. It should focus on plant-based foods rather than animal-based foods. The reason: Meat, sausage, eggs & Co. contain arachidonic acid - a fatty acid that the body uses as a building block for pain relievers and inflammatory substances (prostaglandins).
There is no arachidonic acid in plant foods such as fruit, vegetables and nuts - but plenty of vitamins, minerals and other substances that are good for the sick body.
You can find out more about this and why fish, despite its animal origin, is important for people with rheumatoid arthritis in the article "Diet in Rheumatism".
Rheumatoid arthritis: examinations and diagnosis
Most rheumatoid arthritis patients see their family doctor first. The unspecific symptoms at the beginning of the illness are often misinterpreted as a harmless flu-like infection. If your family has a history of rheumatoid arthritis, your GP will refer you to a rheumatologist. With a lot of experience and extensive specialist knowledge, he can make the correct diagnosis and initiate the necessary therapy.
Medical history and physical examination
To diagnose rheumatoid arthritis, the doctor will first ask you in detail about your medical history (anamnesis). Possible questions are:
- Does anyone in your family have rheumatism?
- When are the symptoms worst?
- Which joints are affected?
- Besides joint pain, have you noticed any other symptoms?
The interview is followed by a physical exam. For example, the doctor will take a close look at your fingers and wrists and check their mobility.
Blood test
A blood test is also important for the diagnosis. As with other inflammations in the body, rheumatoid arthritis also shows noticeable changes in blood values:
- increased CRP (C-reactive protein)
- strongly accelerated ESR (sedimentation rate)
- decreased Hb (hemoglobin = red blood pigment)
- increased ceruloplasmin
- increased α2 and γ bands in electrophoresis
In addition, rheumatism patients often develop anemia.
Laboratory values that can indicate rheumatoid arthritis (RA) are rheumatoid factor, anti-CCP antibodies and other autoantibodies:
- Rheumatoid factor: The term refers to antibodies against so-called Fc fragments of antibodies of the IgG class. They can be found in most RA patients. Then there is what is known as seropositive rheumatoid arthritis. If the rheumatoid factor is missing despite the presence of RA, it is a case of seronegative rheumatoid arthritis.
- Anti-CCP antibodies: They are directed against cyclic citrullinated peptides: Citrulline is a protein building block (amino acid) that occurs in large quantities in the coagulant fibrin, but only rarely in the rest of the body. Fibrin is not only released when the blood clots, but also when there is inflammation in joints. According to the theory, there must be inflammation where citrulline antibodies dock. Anti-CCP antibodies are often detectable in the blood early and in many patients with rheumatoid arthritis.
- Other autoantibodies such as ANA (antinuclear antibodies) can be detected in a few RA patients.
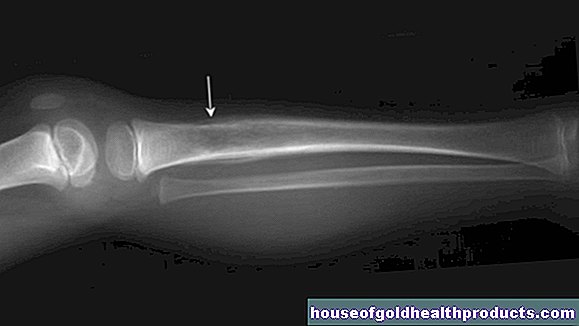
Rheumatoid arthritis: imaging tests
Imaging techniques help diagnose and determine the stage of the disease.
X-rays of the hands and feet, especially at an advanced stage, show changes in the joints that result from rheumatoid arthritis, for example:
- Narrowing of the joint space
- Cartilage atrophy
- Ossifications
- Joint dislocations
Other imaging tests that can help diagnose rheumatoid arthritis include:
- Ultrasound (sonography): visualization of joint effusions and thickening of the tendons
- Scintigraphy (nuclear medicine examination): representation of an increased metabolism in the inflamed area
- Magnetic resonance tomography (magnetic resonance imaging, MRI): presentation of early changes at the onset of the disease
Rheumatoid arthritis: Differentiation from similar diseases
There are many diseases that are associated with joint problems. Therefore, when making a diagnosis, it is important to differentiate rheumatoid arthritis from these diseases. These include:
- ankylosing spondylitis
- Psoriatic arthritis
- Polymyalgia rheumatica
- Sjogren's syndrome
- Systemic lupus erythematosus (SLE)
- Rheumatic fever (post-infectious)
- gout
Rheumatoid arthritis: disease course and prognosis
Rheumatoid arthritis occurs in phases. This means that highly inflammatory, painful conditions alternate with asymptomatic phases. There are often more relapses at the onset of the disease. Overall, rheumatoid arthritis runs in stages, classified according to the predominant symptoms:
- Stage 1: flare-ups of joint swelling and pain, morning stiffness and general symptoms.
- Stage 2: Progressive decrease in joint mobility, muscle and bone loss, involvement of the connective tissue (capsules, tendon sheaths, bursa).
- Stage 3: Beginning destruction of articular cartilage and bones. Gradual damage to the connective tissue (loosening of the ligaments and joint capsule), resulting in instability and misalignment of the joints. Increasingly restricted mobility. Spread of the disease to other regions (cervical spine, large joints, temporomandibular joints).
- Stage 4: Beginning joint stiffening, gross deformations; extensive disability and immobility. The patients are dependent on outside help in everyday life.
The exact course of the disease can vary from patient to patient.
Rheumatoid arthritis: prognosis
Rheumatoid arthritis is incurable and it is difficult to predict how it will turn out in individual cases. However, a rough prognosis can be estimated based on various factors:
- If the rheumatoid factor is present in the blood, the CCP antibodies are particularly high, and the patient is a smoker, it can be assumed to be severe.
- Severe courses are also found in young patients in whom more than 20 joints are affected. Because rheumatoid arthritis often manifests itself outside the joints (extra-articular) in them, their life expectancy is reduced compared to the healthy population.
In addition, the following applies: The symptoms of rheumatoid arthritis often improve during pregnancy.
In any case, it is important to treat rheumatoid arthritis as early and correctly as possible. Then the disease can rest (remission). For this, it is necessary that the patients take their medication for the rest of their lives and have continuous care by their rheumatologist - even during phases in which the disease is dormant. In this way, a flare-up of rheumatoid arthritis can be detected and treated at an early stage.
Consequences of inadequate or inadequate treatment
If rheumatoid arthritis is not treated adequately and properly, cartilage, bones and connective tissue are increasingly destroyed. This results in typical deformities of the fingers and feet:
- Ulnar deviation of the fingers (fingers pointing towards the little finger)
- Buttonhole deformity (flexion malalignment in the middle finger joint, overstretching in the end and metacarpophalangeal joint)
- Gooseneck deformity (flexion malalignment in the end and metacarpophalangeal joints, hyperextension in the middle joint of the fingers)
- 90/90 deformity of the thumb (flexion misalignment in the base joint, overstretching in the end joint)
- Hallux valgus, hammer toes or toe joints pointing to the sides
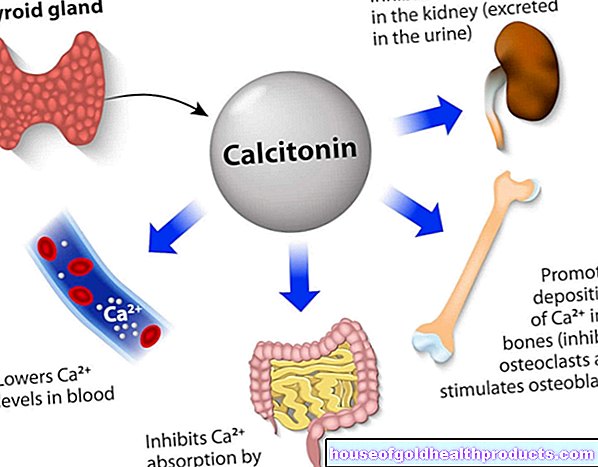
In addition, many patients develop bone loss (osteoporosis) as the disease progresses. Then those affected should ensure that they have an adequate supply of calcium and vitamin D: Calcium is found in dairy products, broccoli or leeks, for example, and vitamin D is mainly in fish. The body can also produce vitamin D itself with the help of sunlight. If necessary, the doctor may also prescribe a preparation with calcium and / or vitamin D.
Rheumatoid Arthritis & COVID-19
The drug treatment of rheumatoid arthritis suppresses inflammation and therefore also the excessive immune system that attacks the own body. It is now unclear whether this also increases the risk of getting more seriously ill with the new infectious disease COVID-19. That is why researchers are currently in the process of collecting international cases of rheumatoid patients with COVID-19 in registers and observing and comparing the courses.
Results so far are reassuring, as most patients recover from COVID-19, even on rheumatism medication. In the register "EULAR and Global Rheumatology Alliance COVID-19", 600 COVID-19 diseases in patients with rheumatic diseases from 40 countries were analyzed from March 24, 2020 to April 20, 2020: The intake of conventional DMARDs, biologicals, non-steroidals Anti-inflammatory drugs and TNF-alpha inhibitors increased the likelihood of not requiring hospital treatment. Only treatment with a moderate to high dose of cortisone (with more than 10 mg of prednisone per day) was associated with a higher likelihood of hospitalization.
However, these are only preliminary findings. More research and studies are needed to better assess the risk. A Covid19 register is also kept in Germany (first data at: https://www.covid19-rheuma.de).
You can support the researchers: Register if you suffer from COVID-19 as a rheumatoid patient or if you would like to take part in a patient survey on the situation of rheumatic patients independently of a COVID-19 illness at https: //www.covid19-rheuma. de / patient information.
Tags: elderly care medicinal herbal home remedies healthy feet