Prostatitis
Sophie Matzik is a freelance writer for the medical team.
More about the experts All content is checked by medical journalists.Prostatitis is inflammation of the male prostate gland (prostate). It is a relatively common condition in men that is associated with pain when emptying the bladder (micturition) and ejaculation. Doctors differentiate between acute and chronic prostatitis. Therapy and prognosis depend on the type and causes of the prostate inflammation. Read everything you need to know about prostatitis here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. N41A54
Prostatitis: description
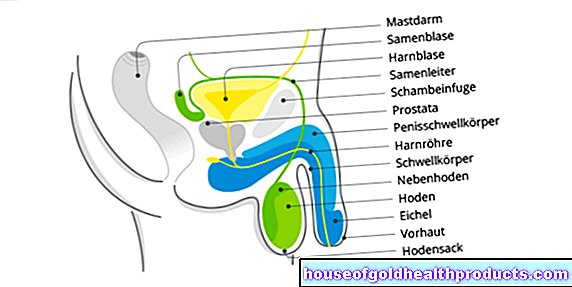
Prostatitis (inflammation of the prostate) is inflammation of the man's prostate gland. The prostate is located just below the urinary bladder and is about the size of a chestnut. It encloses the first section of the urethra and extends up to the so-called pelvic floor, which is made up of muscles.
The prostate produces a secretion, which among other things consists of the PSA (prostate-specific antigen) and the so-called spermine. The PSA makes the ejaculate thinner. The sperm is important for the mobility of the sperm.
Prostatitis is mainly associated with severe pain in the perineum and anal area. In addition, symptoms such as frequent urination, pain when urinating (micturition) and pain during ejaculation occur with inflammation of the prostate.
The prostate is relatively often affected by inflammation. It is estimated that around 15 percent of all men across Germany will develop prostatitis once in their life. The likelihood of developing prostate inflammation increases with age. According to studies, most cases of the disease occur in men between 40 and 50 years of age.
Prostatitis syndrome
In the meantime, a broader understanding of the term prostatitis has established itself in medicine. The so-called prostatitis syndrome includes various complaints in the man's pelvic area, most of which have an unknown cause. Various clinical pictures are summed up under the term prostatitis syndrome:
- Acute bacterial prostatitis
- Chronic bacterial prostatitis
- Inflammatory and non-inflammatory chronic pelvic pain syndrome ("Abacterial Chronic Prostatitis")
- Asymptomatic prostatitis
Acute and chronic bacterial prostatitis
Acute prostatitis is caused by bacteria (acute bacterial prostatitis). The bacteria either reach the prostate via the blood or spread to the prostate from a bacterial infection of the bladder or urethra. Acute prostatitis is usually a serious general illness with severe pain when urinating, fever and chills. Inflammation of the prostate is caused by bacteria in about ten percent of all cases.
Acute prostatitis can develop into chronic prostatitis: If the prostate inflammation lasts for more than three months and germs are repeatedly detected in the urine, the so-called prostate expression (fluid obtained by massaging the prostate) or in the ejaculate, it is chronic bacterial prostatitis. It is less fulminant than acute prostatitis. Chronic prostate inflammation also causes pain when urinating and possibly a feeling of pressure in the perineal area, but the symptoms are usually not as pronounced as in acute prostatitis.
Chronic pelvic pain syndrome (abacterial prostatitis)
In most cases of prostate inflammation, no bacteria in urine, prostate expression or ejaculate can be detected as the cause of the disease. The trigger for prostatitis remains unclear. Doctors call this a chronic pelvic pain syndrome (abacterial chronic prostatitis).
In such cases, however, white blood cells (leukocytes) can often be detected as an expression of the inflammation in the prostate (inflammatory chronic pelvic pain syndrome). This must be distinguished from another form of the disease in which neither bacteria nor leukocytes are detectable (non-inflammatory chronic pelvic pain syndrome). Overall, chronic pelvic pain syndrome (abacterial prostatitis) is the most common form of prostatitis.
Asymptomatic prostatitis
Asymptomatic prostatitis occurs in rare cases. In this form of prostate inflammation, there are signs of inflammation, but there are no pain or other symptoms. Asymptomatic prostatitis is usually discovered by chance, for example during an infertility examination.
Prostatitis: symptoms
Prostate inflammation can trigger a wide variety of symptoms. While the symptoms of acute prostatitis can be very massive and accompanied by a strong feeling of illness, they are usually somewhat milder in chronic prostatitis. Not every affected man necessarily has to experience all of the symptoms listed, and the severity of the symptoms can also vary from man to man.
Acute prostatitis: symptoms
Acute prostatitis is often an acute clinical picture in which those affected suffer from fever and chills. The inflammation of the prostate that surrounds the urethra also leads to typical urination problems. Burning pain occurs when urinating (alguria), and the urine stream is significantly weakened due to the swelling of the prostate (dysuria). Because those affected can only excrete small amounts of urine, they have a constant need to urinate and often have to go to the toilet (pollakiuria). Other symptoms of prostatitis include pain in the bladder, perineum and back area. Pain can also occur during or after ejaculation.
Chronic prostatitis: symptoms
Chronic prostatitis generally causes less severe symptoms than acute prostate inflammation. Symptoms such as fever and chills are usually completely absent. Symptoms of chronic prostate inflammation are typical, such as a feeling of pressure in the perineum or lower abdomen, the ejaculate turning brown from blood in the semen or blood in the urine (hematuria). Libido and erectile dysfunction are frequent symptoms in the chronic form, often caused by pain during or after ejaculation. The symptoms of chronic bacterial and chronic abacterial prostatitis (chronic pelvic pain syndrome) do not differ.
Complications of prostate inflammation
In addition to the acute symptoms, prostatitis can also lead to complications that complicate the course of the disease and prolong the healing process. The most common complication is a prostate abscess (especially in acute bacterial prostatitis). A prostate abscess is a purulent encapsulation of the inflammation, which usually has to be opened by an incision and emptied.
As a further complication of prostate inflammation, the inflammation can spread to nearby structures such as the epididymis or testicles (epididymitis, orchitis). There is also suspicion that chronic prostatitis is associated with the development of prostate cancer.
Prostatitis: causes and risk factors
Prostatitis can have a number of causes. Treatment and prognosis for the inflammation depend on the cause of the prostatitis.
Bacterial prostatitis: causes
In only about ten percent of cases, prostatitis is caused by an infection of the prostate with bacteria (bacterial prostatitis). The bacteria can enter the prostate either via the blood (hematogenous) or from neighboring organs such as the urinary bladder or urethra, where they cause an inflammatory reaction.
The Escherichia Coli bacterium (E. coli), which occurs primarily in the human intestine, is the most common cause of prostate inflammation. However, Klebsiella, enterococci or mycobacteria can also cause prostatitis. Bacterial prostatitis can also result from sexually transmitted diseases such as chlamydial or trichomonas infections as well as gonorrhea (gonorrhea).
In chronic prostatitis, the bacteria in the prostate evade the defense of the human immune system in a way that has not yet been explained with certainty. This allows the germs to colonize the prostate permanently. Antibiotics work relatively poorly in prostate tissue, which could be another cause of the bacteria in the prostate to survive.
Chronic pelvic pain syndrome: causes
The exact causes of chronic pelvic pain syndrome are still not fully understood. Scientists have put forward various theories about this, each of which sounds plausible, but all of which have not yet been clearly proven. In some cases, the genetic material of previously unknown microorganisms was detected in the basin. The cause of the pelvic pain syndrome could therefore be microorganisms that to this day cannot be cultivated in the laboratory and are therefore not detectable.
Another possible cause of chronic pelvic pain syndrome is urination disorders. The outflow disturbance increases the volume of the bladder, which presses on the prostate. Over time, this pressure damages the prostate tissue, causing inflammation.
Another possible cause is believed to be that inflammation of the bladder tissue can also spread to the prostate.
It is also conceivable that nerve irritation in the vicinity of the prostate leads to pain that is incorrectly attributed to the prostate.
Finally, it is also conceivable that an overactive or misdirected immune system could cause chronic pelvic pain syndrome.
In many cases, however, the cause of chronic pelvic pain cannot be clearly established. Doctors then speak of idiopathic prostatitis.
Anatomical causes
In rare cases, prostatitis is caused by narrowing of the lower urinary tract. If the urinary tract is narrowed, the urine backs up and can also cause inflammation if it penetrates the prostate. Such a narrowing can be caused by tumors or so-called prostate stones.
Doctors also suspect that a dysfunction of the pelvic floor muscles can promote the development of prostatitis.
Psychological causes
Lately, the psychological causes of prostatitis have also been discussed more and more. In the case of non-inflammatory chronic pelvic pain syndrome in particular, a psychological trigger is likely. The exact mechanisms are still unknown.
Risk factors for prostatitis
Some men are particularly at risk of developing prostate inflammation. These include, for example, men with a disorder of the immune system or a suppressed immune system (for example through drug, immunosuppressive therapy). Underlying diseases such as diabetes mellitus can also promote prostatitis: the increased blood sugar level in diabetes patients often also leads to an increased sugar level in the urine. It is possible that the abundant sugar in the urine provides the bacteria with good growth conditions, so that urinary tract infections can develop more easily. In addition, the immune system is weakened in diabetes mellitus.
Another risk factor for prostatitis is a urinary catheter. Just inserting the urinary catheter through the urethra into the bladder can lead to small tears in the urethra and injuries to the prostate. In addition, like any other foreign body, bacteria can settle on a urinary catheter and form a so-called biofilm. This allows bacteria to ascend along the urethra to the bladder and thereby also lead to an inflammation of the prostate.
Prostatitis: examinations and diagnosis
If you have problems with the prostate, your family doctor or a urologist is the right contact. The family doctor can take the medical history (anamnesis), but if prostatitis is suspected, he will refer you to a urologist. This will conduct a physical exam.If prostatitis is suspected, this is usually the so-called digital rectal examination. However, this examination does not yet provide any clear evidence of prostate inflammation, but only corroborates the suspicion. A laboratory test can follow to detect bacterial prostatitis. If no specific cause can be proven, appropriate treatment is given even if there is a justified suspicion of prostatitis.
anamnese
Typical questions when recording the medical history (anamnesis) can be:
- Do you have pain when urinating?
- Where exactly do you feel the pain?
- Do you have back pain?
- Have you noticed any changes in ejaculation?
Digital rectal exam
Since the prostate is directly adjacent to the rectum, it can be felt over the rectum with a finger. This digital rectal examination is carried out on an outpatient basis and without anesthesia; it is usually painless. The patient is asked to lie down on their sides with knees bent. With the help of lubricant, the doctor then slowly inserts a finger into the anus and feels the prostate and adjacent organs (palpation). He checks the size and sensitivity of the prostate to pain: an inflamed prostate gland is greatly enlarged and very sensitive to pain.
Laboratory examination
In most cases, the urine is tested in order to be able to detect possible pathogens. The standard method is the so-called four-glass test. The first urine, the midstream urine, a prostate expression and the urine after a massage of the prostate are tested. Doctors refer to the secretion of the prostate as prostate expression. The doctor receives this by applying light pressure on the prostate, for example during palpation. The ejaculate can also be examined for pathogens and signs of inflammation.
Further investigations
A rectal ultrasound examination (sonography) can determine exactly where the inflammation is localized and how far it has spread. Another important goal of the investigation is to rule out other diseases with similar symptoms (differential diagnoses).
In order to be able to rule out that an existing urinary flow disorder is caused by a narrowing of the urethra, a urinary flow measurement (uroflowmetry) is carried out. To do this, the patient urinates in a special funnel that measures the amount of urine per unit of time. A normal urine flow is between 15 and 50 milliliters per second, with a urine flow of ten milliliters per second or less there is a high probability that there is an obstruction in the urethra.
Prostatitis: PSA measurement
An elevated PSA (prostate-specific antigen) level in the blood is generally considered an indicator of prostate cancer. However, even with prostatitis, PSA levels in the blood can be greatly increased. If the reading is significantly increased, a tissue sample (biopsy) is usually carried out and examined in a laboratory to reliably rule out prostate cancer.
Prostatitis: treatment
As with other diseases, prostatitis therapy and duration of treatment depend on the triggering cause.
Medical therapy
Acute bacterial prostatitis is treated with antibiotics. In mild cases, administration of antibiotics for about ten days is sufficient. With chronic prostatitis, the medication must be taken for a longer period of time (around four to six months). Depending on the pathogen, ofloxacin, ciprofloxacin, azithromycin, erythromycin or doxycycline can be used as active ingredients. Even if the symptoms have already subsided, the antibiotics should in any case continue to be taken as prescribed by the doctor. This prevents a relapse and reduces the likelihood of a relapse.
Asymptomatic prostatitis is also treated with antibiotics.
If there is chronic abacterial prostatitis (chronic pelvic pain syndrome), antibiotic therapy is usually ineffective. In the case of inflammatory chronic pelvic pain syndrome, despite the lack of evidence of a pathogen, it is worth trying antibiotics, as an improvement can sometimes be achieved. In contrast, antibiotic therapy is not recommended for non-inflammatory chronic pelvic pain syndrome.
Further therapeutic approaches for chronic abacterial prostatitis are so-called 5α-reductase inhibitors such as finasteride or dutasteride, pentosan polysulphate and herbal medicines (phytotherapeutic agents) such as quercetin or pollen extract. If this also does not improve, the drug therapy is supplemented with a physical therapy. Exercise therapy, pelvic floor exercises or regular prostate massage are recommended here. In addition, microwave heat therapy can stimulate the tissue to increase blood flow and reduce pain.
Symptomatic therapy
Symptomatic therapy can also help to alleviate acute symptoms of prostate inflammation. Pain reliever medication can be prescribed for severe pain. Heat pillows and hot water bottles on the back or lower abdomen also help to relax the muscles. This often relieves the pain of prostate inflammation.
Home remedies such as a rye cure or eating soft-skinned pumpkin seeds can also help against the symptoms of prostatitis. Other tips include regular pelvic floor training, avoiding a sharp bicycle saddle and beer, meat, fat and sugar.
Treatment of complications
If the disease causes a massive obstruction of the urinary flow, a prostate removal (prostatectomy) can be useful, as residual urine always carries a high risk of infection in the urinary tract.
If the inflammation causes pus to become encapsulated in the prostate (abscess), it must be emptied through an incision. The access route is usually the rectum.
Relapse
The overall relapse rate in prostatitis is very high. Around 23 percent of all those affected go through a second episode of illness after a single illness, 14 percent suffer three and 20 percent even four or more cases. To reduce the risk of a relapse, you should avoid wearing wet clothes during and after prostatitis, overcooling (for example during exercise) or drinking bladder-irritating drinks such as black tea or coffee. This reduces the risk of cystitis and thus prostatitis. However, these methods cannot safely prevent prostatitis caused by bacteria.
Prostatitis: disease course and prognosis
The prognosis of prostatitis depends on the one hand on the cause of the inflammation and on the other hand on how quickly the right therapy is started.
In the case of acute bacterial prostatitis that is treated as quickly as possible with antibiotic therapy, the prognosis is usually good. Taking antibiotics kills the pathogens, which usually prevents the transition to chronic prostatitis.
Scientists suspect that pain during ejaculation increases the risk of chronic prostatitis. Such pain is a sign of a change in the positional relationships of the structures in the pelvic area, for example the prostate being crushed by the urinary bladder. Chronic prostatitis can develop if this compression persists for a long period of time.
About 60 percent of all patients with acute prostatitis no longer show symptoms after six months, and about 20 percent develop chronic prostate inflammation. Treatment and prognosis are more difficult here. In many cases, intermittent episodes of illness occur that can accompany those affected for many years.
Chronic prostatitis usually requires enormous patience from those affected. The very often protracted course can mean a great deal of psychological stress. Affected patients should seek professional help (e.g. psychotherapeutic support) if necessary, as their mental state has an enormous influence on the prognosis of prostatitis.
Tags: alcohol alternative medicine drugs