The lost donors
Christiane Fux studied journalism and psychology in Hamburg. The experienced medical editor has been writing magazine articles, news and factual texts on all conceivable health topics since 2001. In addition to her work for, Christiane Fux is also active in prose. Her first crime novel was published in 2012, and she also writes, designs and publishes her own crime plays.
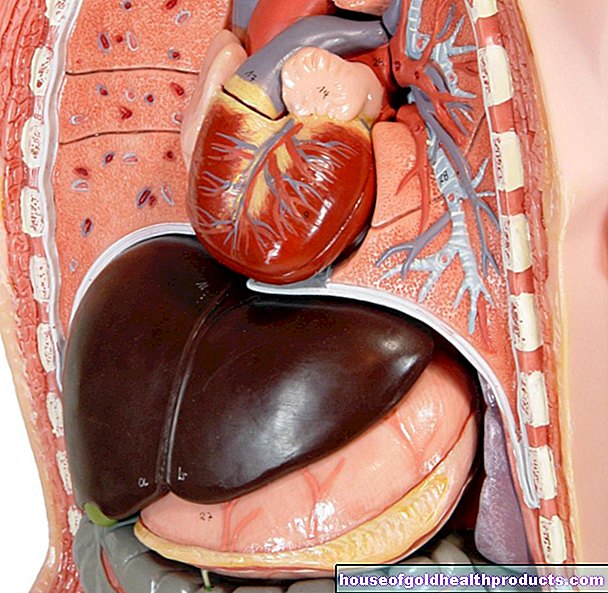
More posts by Christiane Fux All content is checked by medical journalists.There is an organ emergency at German transplant clinics. But the main problem is not a lack of willingness to donate. Often it is up to the clinics. What's wrong?
There is a great shortage in rich Germany. On donor organs. And that has become even worse due to the major organ donation scandals. A study has now revealed that the main reason is no longer a lack of willingness to donate. Far too often, the clinics fail to identify and report potential donors.
797 - the number of people who became organ donors in 2017. In 2010 it was 1296. A devastating result. This means that the clinics had fewer than 2,700 donor organs at their disposal - for around 10,000 people who hope for a heart, liver, healthy kidney or lungs every year.
The willingness to donate is actually high in Germany: around 80 percent of people are positive about organ donation, 36 percent have a donor card - more than ever before. More than 90 percent of them confirm their consent to organ removal.
More willing to donate, fewer transplants
Researchers working with Prof. Thorsten Feldkamp and Dr. Kevin Schulte from the University Medical Center Schleswig-Holstein found out. To determine this number, the scientists developed a special software program based on the accounting data from the clinics.
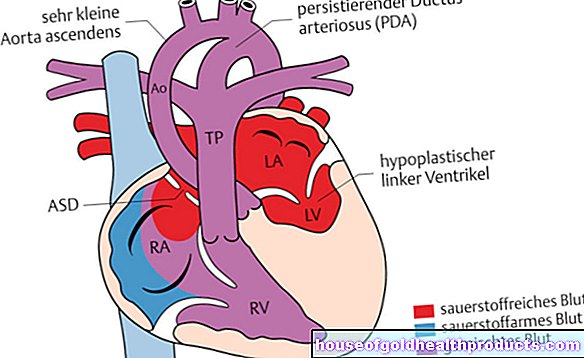
"Potential donors" are those who have died for whom organ donation would probably have been possible. These are all patients who have suffered severe brain damage and to whom no obvious exclusion criterion applies: "For example, you cannot donate organs with an active cancer disease," says Dr. Axel Rahmel in conversation with The Medical Board of the German Organ Transplantation Foundation (DSO) was also involved in the study.
Another exclusion criterion is if the body is so badly damaged that the doctors are unable to stabilize the circulation. Even if a patient is not in the intensive care unit and is therefore not artificially ventilated, he or she will not be a donor. And then there are severely brain-damaged people who continue to breathe independently - a clear sign that their brain stem is still working, i.e. that there is no brain death.
Overall, the researchers found, the number of potential donors rose by 13.9 percent between 2010 and 2015.
Possible donors are often not reported
More possible donors, more willing to donate - and still a third fewer transplants? The scientists soon found the solution to this apparent contradiction: More and more suitable donors were not reported to the DSO at all. In 2016, for example, there were around 4,600 deaths with severe brain damage in North Rhine-Westphalia that might have been considered as organ donors. “Ultimately, we were notified of 369 cases,” says Rahmel.
The DSO employees, together with the clinic doctors on site, investigated what the other patients were all about. "At least with 911 of the other deceased, the possibility of organ donation should have been carefully considered," Rahmel reports. No brain death diagnosis was carried out in 118 of them, although the brain functions were probably irretrievably lost.
In another 371 patients, there was also no longer any hope that the brain would recover. The doctors then shut down the therapy in consultation with the relatives. However, she had not previously asked her about the possibility of organ donation. "Some of these patients would probably also have been considered as donors," says Rahmel.
Hectic everyday clinical routine, lack of knowledge, psychological hurdles
How did it happen that so many possible opportunities for donor organs were missed? “You always have to look at the individual case. The increasing intensification of work in the clinics certainly plays a not insignificant role, ”says Rahmel. First of all, it makes sense to end therapy for brain injured people for whom there is no longer any hope. In the hustle and bustle of everyday hospital life, people quickly forget that they are possible donors.
Sometimes the necessary knowledge is also missing in the clinics: for example, that a cancer survivor can be a donor again ten years later. Or that organs that are 75 years old can still help if they are sufficiently efficient.
Psychological barriers can also be a reason. Rahmel reports on a special case: “The parents of a brain-dead child asked the doctors themselves about the possibility of organ donation. The doctors just didn't dare to ask. "
Transplant officer in time trouble
The so-called transplant officers should actually ensure that such hurdles do not become obstacles to organ donation. They have been mandatory in all extraction clinics since 2012. Its central task is to act as an interface between the clinic and the DSO. The specially trained medical professionals must keep an eye on who is eligible as a donor and accompany the process. “You have to work closely with the intensive care units, be involved in decisions, but also educate relatives. All of this takes time, ”explains Rahmel.
The idea is good, but implementation is still a problem in many places. "The problem is that the tasks as well as the rights of the transplant officers had not yet been clearly regulated - that was a matter for the federal states," says Rahmel. Often the transplant officers were given new tasks without giving them the necessary time to carry them out.
Bavaria as a model
Bavaria is an exception. The state was particularly hard hit by the transplant scandal. That may also be one reason why the role of the transplant officer has been particularly strengthened here.
In designated transplant centers, the representative must be completely relieved of other tasks; in other clinics with intensive medical care, the degree of exemption is calculated depending on the number of intensive care beds: for every ten beds there is one tenth position. The measures are obviously working: Contrary to the previous federal trend, the number of organs removed in the Free State has increased by 18 percent.
The Bavarian model is now to become a model for other federal states. Corresponding plans, including for a more consistent release, are already set out in the coalition agreement. “That is a clear political goal,” said Rahmel.
Thinking about organ donation must become a matter of course
The DSO doctor hopes that this will lead to a rethinking of patients with severe brain damage. “We want to promote a culture in which thinking about organ donation at the end of life is a matter of course both in society and in clinics,” explains the doctor. Only if this becomes part of the routine will it not be lost again and again in the stressful everyday clinical routine.
Is the trend reversal finally coming?
The first successes of the constant education by the DSO and other organizations are already evident: The recently published figures indicate a slight trend reversal that is encouraging: for the first time in years, the number of transplants is increasing again. In the first half of 2018, a total of 484 donors across Germany were able to take organs for transplantation. That is a remarkable 72 more donors than from January to June 2017.
Tags: stress sex partnership vaccinations