Hypoplastic left heart syndrome
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Hypoplastic left heart syndrome (HLHS) is a serious congenital heart defect. The left half of the heart and the main artery are underdeveloped (= hypoplastic) or have defects. The result is heart failure - the heart cannot pump enough blood around the body. If affected babies are not treated quickly, they will die. Read more about Hypoplastic Left Heart Syndrome here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. Q23
Brief overview
- What is Hypoplastic Left Heart Syndrome (HLHS)? A serious congenital heart defect in which the left ventricle and the part of the main artery that branches off from it are underdeveloped. In addition, the heart valves in the left half of the heart are narrowed or closed. Sometimes other defects also accompany hypoplastic left heart syndrome.
- Causes: several changes (mutations) in different genes
- Effects: Heart failure (heart failure), which means that too little blood is pumped into the body. If left untreated, HLHS is fatal within a short time after birth.
- Symptoms: e.g. rapid breathing, shortness of breath, pale-cool skin, weak pulse, bluish discolored skin and mucous membranes
- Diagnosis: by means of cardiac ultrasound; cardiac catheterization is rarely necessary
- Treatment: Medication to bridge the time until multi-step surgery or a heart transplant can enable longer-term survival.
What is Hypoplastic Left Heart Syndrome (HLHS)?
Hypoplastic left heart syndrome (HLHS) is a serious congenital heart defect. It mainly affects the left half of the heart and the main artery (aorta) that branches off from it. The HLHS causes heart failure (heart failure), the consequences of which lead to death without rapid treatment.
If only one heart chamber (ventricle) is fully developed, as in the HLHS, doctors also speak of a single-chamber heart or univentricular heart.
In detail, hypoplastic left heart syndrome is characterized by a combination of the following malformations:
Underdevelopment of the left ventricle: The left ventricle is severely underdeveloped (hypoplastic), i.e. very small. As a result, it is hardly or not able to perform its task - namely to pump blood into the branching artery (aorta) and thus further into the body (abdominal organs, arms, legs, etc.).
Underdevelopment of the ascending aorta: The ascending aorta ("ascending" aorta) is the first section of the main artery (aorta) extending from the left ventricle. She is also not properly trained at HLHS.
Underdevelopment of the isthmus aortae: The isthmus aortae is a natural bottleneck in the aorta at the transition between the aortic arch (second section of the aorta) and the descending aorta ("descending" aorta; third section of the aorta).
Severe narrowing (stenosis) or occlusion (atresia) of heart valves: The mitral valve (between the left atrium and left ventricle) and the aortic valve (between the left ventricle and aorta) are affected. Depending on the type of heart valve defect, there are four subgroups of hypoplastic left heart syndrome, such as MA / AoA (mitral and aortic valve atresia) or MS / AoA (mitral valve stenosis and aortic valve atresia)
Sometimes hypoplastic left heart syndrome is accompanied by other malformations of the heart and blood vessels, such as a ventricular septal defect: In this type of heart defect, the septum between the two chambers of the heart is not completely closed. Or there are additional malformations of the coronary arteries. Some HLHS children also have other abnormalities outside of the heart, such as a non-continuous esophagus or an underdeveloped duodenum (esophageal or duodenal atresia).
Hypoplastic left heart syndrome occurs in up to ten percent of cases in the context of genetic syndromes such as trisomy 21 (Down syndrome) or Turner syndrome.
Hypoplastic left heart syndrome: frequency
Hypoplastic left heart syndrome is rare: it affects about one to three children in 10,000 live born children. Boys are more often affected than girls.
Hypoplastic left heart syndrome accounts for around one to two percent of all congenital heart defects. However, it is one of the most common causes of heart failure (heart failure) in newborns. HLHS is also the most common cause of heart-related death in babies in the first week of life.
What happens at HLHS?
Hypoplastic left heart syndrome has serious consequences: the underdevelopment and malformations of the left half of the heart make it more or less inoperable. The right half of the heart has to take on its task: to pump the blood into the body's circulation. This is only possible without problems for children until shortly after birth, because they have "short circuits" in their bloodstream:
Ductus arteriosus and foramen ovale
The ductus arteriosus is a direct vascular connection in the unborn child between the pulmonary artery (originates from the right ventricle and leads into the pulmonary circulation) and the aorta - more precisely the "descending" aorta (aorta descendens), which leads into the body circulation. It is important for the fetus's blood circulation:
The child's lungs do not have to and cannot yet fulfill their function in the womb (i.e. load the blood with oxygen). Instead, the mother delivers oxygenated blood to the fetus. It passes through the umbilical cord into the child's inferior vena cava and on to the right atrium. From there it flows through the right ventricle into the pulmonary artery. Here only a small part of the blood is directed into the still "shut down" lungs. Instead, most of it is transported via the ductus arteriosus directly into the main artery (aorta) and thus further into the body's circulation.
The foramen ovale can also be used to bypass the lungs, which only start working after birth: This is a natural small opening in the atrial septum in the fetus (unborn from the 9th week of pregnancy until birth). Through this opening, part of the oxygen-rich umbilical cord blood can flow directly from the right to the left atrium and thus be fed into the body's circulation.
After the birth, the "short circuits" disappear
In the first few days after the birth, the ductus arteriosus closes and the pulmonary circulation is expanded: the blood flowing from the right ventricle into the pulmonary artery now completely reaches the lungs, where it is charged with oxygen via the inhaled air. It then returns to the heart via the pulmonary veins, to the left side of the heart, which it then pumps into the body's circulation - at least in babies without HLHS.
The foramen ovale also usually closes on its own shortly after birth. Sometimes it remains partially or completely (open foramen ovale).
HLHS: After the birth, “short circuits” are essential for survival
An open ductus arteriosus and an open oval shape ensure the survival of newborns with HLHS: oxygen-enriched blood, which comes from the now expanded lung and flows into the left atrium, can reach the right atrium via the open foramen oval. There it mixes with the deoxygenated blood from the body.
The heart pumps this “mixed blood” through the right ventricle into the lungs. From there, part of the blood flows through the still open ductus arteriosus into the body's circulation and thus maintains the supply of the organs and other tissues.
An occlusion of the ductus arteriosus shortly after birth therefore has dramatic consequences if hypoplastic left heart syndrome is present. The underdeveloped left ventricle can hardly or not at all maintain the body's circulation.
As a result of the closure of the foramen ovale, the blood in the left atrium also backs up into the lungs because it can no longer flow into the right atrium. However, the right ventricle continues to pump blood to the lungs. The volume of blood in the lungs increases rapidly and breathing deteriorates noticeably.
Hypoplastic left heart syndrome: symptoms
Hypoplastic left heart syndrome becomes noticeable with symptoms as soon as the ductus arteriosus begins to close after birth (HLHS children therefore usually appear healthy immediately after delivery). Affected babies quickly develop signs of cardiogenic shock (= shock that originates in the heart):
- rapid breathing
- Shortness of breath
- weak pulse
- paleness
- bluish discoloration of the skin and mucous membranes (cyanosis)
- low body temperature (hypothermia)
- metabolic acidosis (metabolic acidosis)
- Apathy (lethargy)
- decreased or absent urination (oliguria or anuria) - so hardly any wet diapers
Due to the underdevelopment and malformations of the left half of the heart and the aorta, too little oxygen-rich blood ends up in the body's circulation. In addition, the blood flow to the lungs continues to increase through various mechanisms. That puts an enormous strain on breathing.
If the circulatory situation deteriorates further, there is a risk of heart and cerebral infarction (stroke due to reduced blood flow). Damage to other organs (such as the liver, intestines) can also occur due to the insufficient supply of blood.
If the ductus arteriosus is not opened again immediately so that the right half of the heart can continue to pump blood into the body's circulation via this "short circuit", at least for the time being, the baby will die of cardiovascular failure!
If a newborn shows symptoms as described above, hypoplastic left heart syndrome is suspected. This is especially true if the metabolic acidosis of the blood (metabolic acidosis) worsens after the administration of oxygen - a common and characteristic sign of HLHS. Sometimes the symptoms are initially misinterpreted as an "adjustment disorder". If you are concerned about your baby, it is best to speak to the pediatrician again.
Hypoplastic left heart syndrome: diagnosis
After each birth, paediatricians, among other things, listen to the heart and measure the oxygen saturation in the blood (pulse oximetry). In the HLHS, however, these examinations are often normal at first.
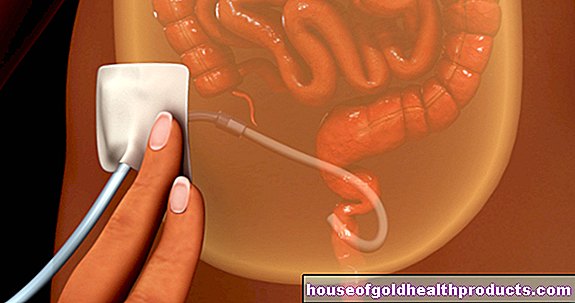
A hypoplastic left heart syndrome can be reliably proven by means of a cardiac ultrasound examination (echocardiography). With their help, the doctor can assess how pronounced the underdevelopment and malformations of the left half of the heart and the aorta are and which subtype of HLHS is present. An examination using a cardiac catheter is only rarely necessary for the diagnosis (read more about this procedure here).
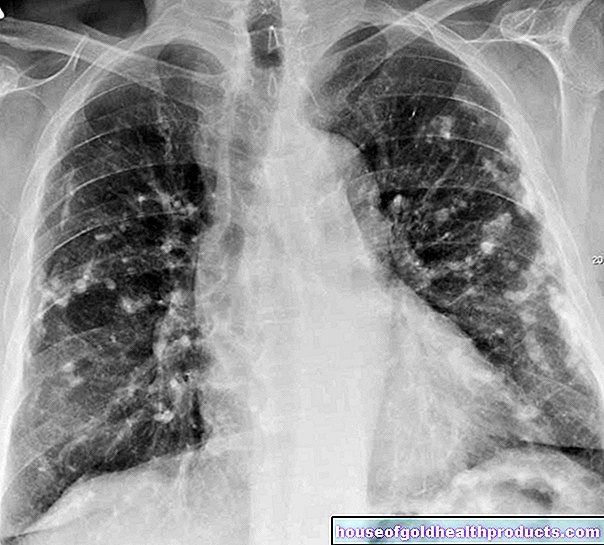
Further studies provide information on the effects and possible consequential damage of hypoplastic left heart syndrome. For example, different blood values show how pronounced the metabolic dysfunction (hyperacidity) is. The enlargement of the heart muscle (cardiomegaly), which is usually present in hypoplastic left heart syndrome, can be seen on chest x-rays (chest x-ray) - as well as increased pulmonary vessel markings. The x-ray may also show an accumulation of fluid in the lungs (pulmonary edema).
In most affected children, hypoplastic left heart syndrome is discovered in the womb - during one of the ultrasound examinations that are provided during pregnancy or a cardiac ultrasound examination of the fetus. Doctors then initiate treatment for HLHS immediately after the birth.
How is Hypoplastic Left Heart Syndrome treated?
Doctors immediately move babies with hypoplastic left heart syndrome to a neonatal intensive care unit or an intensive care unit for children with heart disease. There you can not only monitor it continuously, but also stabilize it until an operation is possible.
Until then you have to keep the ductus arteriosus open: To do this, the baby is given an infusion with prostaglandin E1 (PEG1). This active ingredient can prevent the short-circuit connection between the pulmonary artery and the main artery from closing or can completely open the short-circuit again.
If doctors have already found the heart defect in the womb, the newborn is given the prostaglandin infusion immediately after its birth.
In addition, babies with HLHS are stabilized and treated as needed. Seriously ill babies may need mechanical ventilation to ensure oxygen supply to the small body. Sometimes an HLHS baby also needs medication to improve cardiovascular function.
Three-step surgical procedure
For the continued survival of babies with hypoplastic left heart syndrome, doctors usually recommend a multi-stage surgical procedure: the heart and vessels near the heart (such as the aorta, pulmonary artery) are "remodeled" in three interventions. As a result, the right ventricle can in future take over the function of the underdeveloped left ventricle: It pumps oxygen-rich blood from the lungs into the body's circulation.
The "used", oxygen-poor blood flowing back from the organs flows directly into the lungs via a diversion without any pump support from the heart. After the three interventions, the lungs and body blood circulation function practically separately from each other with only one heart chamber as the "motor" (Fontan's circulation).
The schedule of the three-step surgical procedure:
- 1st stage (Norwood procedure / Norwood operation I, alternatively: hybrid therapy): in the first week of life
- 2nd stage (bidirectional Glenn or Hemi-Fontan procedure, also called Norwood operation II): at the age of three to six months
- 3rd stage (Fontan procedure, also Norwood OP III): at the age of 24 to 36 months
Heart transplant
In particularly severe cases, a heart transplant is sometimes the better choice of therapy for hypoplastic left heart syndrome than three-stage cardiovascular remodeling. Until a suitable donor heart is available, doctors continue to use prostaglandin infusions (and other necessary measures) to keep the baby alive. Unfortunately, this does not always work because the supply of donor hearts is limited. About 20 percent of babies with HLHS die while waiting for a transplant.
Some children with a single-chamber heart develop pronounced cardiac insufficiency over time, even after an operation. In these cases, a heart transplant is often necessary as well.
Living with HLHS
A hypoplastic left heart requires some people to take long-term anticoagulant medication to prevent blood clots from forming. Many children also need one or more drugs to help their heart function.
Some children with HLHS need to take antibiotics before a dentist or certain operations (e.g. on the respiratory tract). This is to prevent bacterial inflammation of the inner lining of the heart (endocarditis), which can occur as a result of such interventions.
Children who have had a donor heart transplanted have to take immunosuppressants for life - drugs that suppress the immune system so that it does not reject the foreign organ. As a side effect, those affected are more prone to infections. In addition, the immunosuppressants cause pathological changes in the vessels supplying the heart (coronary arteries) in many children within the first five years. Then a new heart transplant will be necessary.
HLHS: Complications
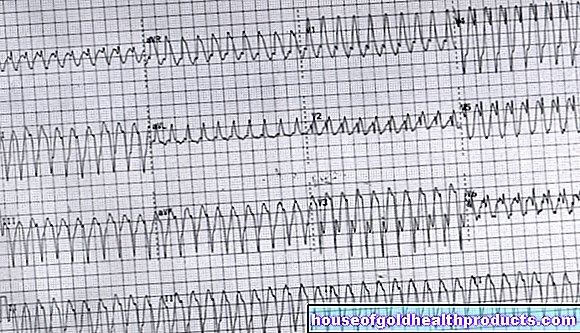
Some children get arrhythmias. If the heart beats too slowly, a pacemaker may be necessary. However, an operated HLHS heart can also beat very quickly. In these cases, medication can also help. Doctors may obliterate a certain part of the heart muscle (ablation) so that the electrical impulses can spread again regularly.
A possible consequence of the HLHS - even after a successful operation - is a weakening single-chamber heart. On the other hand, medication can work in mild forms. However, sometimes a heart transplant is needed.
After an HLHS operation, the pressure conditions in the blood circulation change. For example, the pressure in the vena cava is increased. As a result, proteins leak from the blood into the intestines, where they cause diarrhea (protein loss syndrome / enteropathy). Children with hypoplastic left heart syndrome can develop this complication as they age. As a result, protein loss occurs in some people only in adolescence.
The lungs, more precisely the bronchi, can also be affected by such an event (bronchitis fibroplastica). Affected children suffer from the leaked protein and fibrin-containing liquid, strong coughing fits and sometimes develop severe breathing problems. The complaints doctors then try to alleviate the complaints through various examinations and measures. A protein-rich diet can be helpful or necessary if too much protein is lost.
Developmental disorders are often associated with hypoplastic left heart syndrome. It is therefore important that the children are permanently cared for by specialist paediatricians and that they receive targeted early support.
Quality of Life of Children with HLHS
The general quality of life differs from case to case. Some HLHS children can live almost normally (play, kindergarten, school, light exercise). Others have repeatedly suffered severe performance losses. However, the physical performance of people with hypoplastic left heart syndrome is usually generally limited compared to healthy people.
HLHS: life expectancy
The course and prognosis of hypoplastic left heart syndrome depend largely on the type and severity of the heart defect and the time of treatment. The HLHS is definitely life-threatening: If a baby is born with HLHS, its immediate survival depends on the ductus arteriosus being kept open or reopened until the child is operated on (or receives a new heart). If left untreated, it dies within a few days to weeks.
What life expectancy and long-term prognosis will look like in an operated hypoplastic left heart syndrome cannot be precisely predicted. According to various studies, 50 to 80 percent of affected children are still alive after five years. The 10-year survival rate is given as around 50 to 70 percent.
The 5-year survival rate after a heart transplant is similar to that after the multi-step surgical procedure.
The majority of children with HLHS today are likely to reach adulthood thanks to improved therapies. However, if hypoplastic left heart syndrome occurs as part of a genetic syndrome (such as trisomy 21, Turner syndrome) or together with other malformations, the prognosis worsens.
Tags: laboratory values Baby Child menshealth


.jpg)


.jpg)