Fibrous dysplasia
All content is checked by medical journalists.Fibrous dysplasia (Jaffé-Lichtenstein's disease) is a malformation of the bones. It occurs mainly in children and adolescents. Instead of growing properly and developing a solid, mineral structure, individual bones form fibrous swellings. This is why fibrous dysplasia is sometimes referred to as a “tumor-like bone lesion”. Here you can find out everything you need to know about this disease.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. Q78M85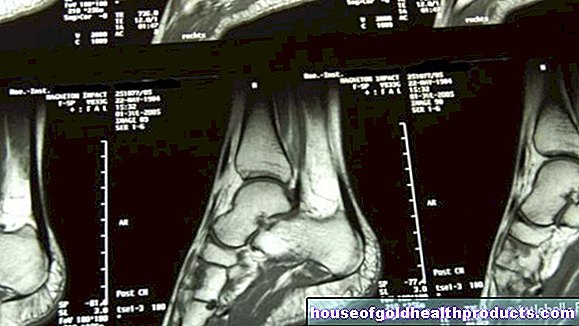
Fibrous dysplasia: description
Fibrous dysplasia is a congenital disease in which one or more bones do not develop in their normal cell structure; instead, tumors develop from fibrous connective tissue. Most often this happens on a thigh bone, but the shins, ribs, skull and jaw bones are also relatively often affected.
Fibrous dysplasia is based on a genetic defect, but it is not hereditary. Male and female sufferers are roughly in balance, although progressive forms with several affected bones (polystotic fibrous dysplasia) seem to be more common in girls. Children and adolescents between 5 and 15 years of age are most likely to develop the disease, and adults are less common.
Although it is one of the most common bone diseases, fibrous dysplasia is a rare disease overall. Exact figures are not known, however, since fibrous dysplasia in many cases proceeds without noticeable symptoms; Doctors therefore assume that it is often undiagnosed.
Fibrous dysplasia: different manifestations
Doctors differentiate between different forms of the disease:
- monostotic fibrous dysplasia (70%): only one bone is affected
- polystotic fibrous dysplasia (25%): multiple bones are affected
- McCune-Albright syndrome (very rare): fibrous dysplasia with café-au-lait spots and premature sexual maturity
McCune-Albright syndrome is often listed as a disorder in its own right, but has the same genetic basis as fibrous dysplasia and has no other noticeable symptoms.
Fibrous dysplasia: symptoms
Fibrous dysplasia can take very different courses; therefore the symptoms differ depending on the severity and which bones are affected. While some sufferers are completely symptom-free, others show various symptoms:
- easy pulling bone pain
- Stress pain (e.g. if the thigh bone is affected)
- Difficulty walking, causing some to limp
- frequent spontaneous bone fractures with actually light stress (fatigue fractures)
- Externally visible "bumps", curvatures and other changes in the bones (e.g. a visibly deformed facial skull)
- rapid physical development in affected children and adolescents (rapid growth and early puberty)
- Pigment disorders, so-called café-au-lait spots
The last two symptoms belong to the so-called McCune-Albright syndrome; very few people with fibrous dysplasia are affected. Café-au-lait spots are uniformly light brown, sharply delineated spots that also occur, for example, in the hereditary disease neurofibromatosis type 1 (Recklinghausen's disease). In McCune-Albright syndrome, they often concentrate on one half of the body - just like fibrous dysplasia or the areas affected by it ("foci"). The premature onset of puberty is due to a change in the hormonal balance. Sometimes fibrous dysplasia also occurs together with other hormonal diseases, such as diabetes, Cushing's disease or an overactive thyroid.
Fibrous dysplasia: causes and risk factors
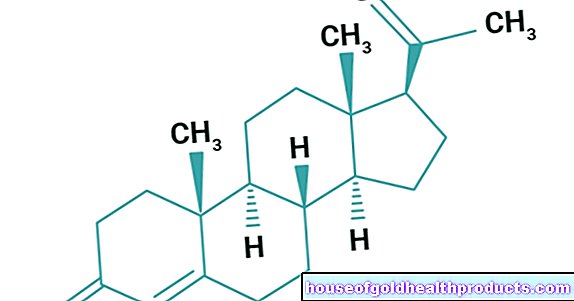
Fibrous dysplasia is due to a change in the genetic make-up: the so-called GNAS gene on the 20th chromosome is changed (mutated). This causes the enzyme adenylate cyclase to produce too much cAMP (cyclic adenosine monophosphate), a particular substance that plays an important role in signal transmission in the cell. Ultimately, the mutation leads to the fact that the spongy inner layer of the bone - the so-called cancellous bone - is not properly formed. In their place there is a soft, non-mineralized, connective tissue-like bone substance (osteoid). The cells divide before they are properly differentiated, which means that the bone can be literally expanded.
The genetic defect only affects body cells and not the germ cells - one also speaks of a somatic mutation. Presumably, the gene mutates during embryonic development or in early childhood, so the mutation is not in the genome from the start. This means that the GNAS gene defect is not hereditary.
Fibrous dysplasia: examinations and diagnosis
To diagnose fibrous dysplasia, the doctor first asks about the symptoms and the medical history (anamnesis). For example, he asks about possible pain, in which situations it occurs and whether one or more areas are affected. During a physical examination, he looks at the abnormal areas and feels them to check for changes. The doctor may take blood from the person concerned. In the case of fibrous dysplasia, the calcium and phosphate levels in the blood serum are normal; but the enzyme alkaline phosphatase may be increased. This blood count belongs to a group of enzymes that can indicate changes in bone metabolism, among other things.
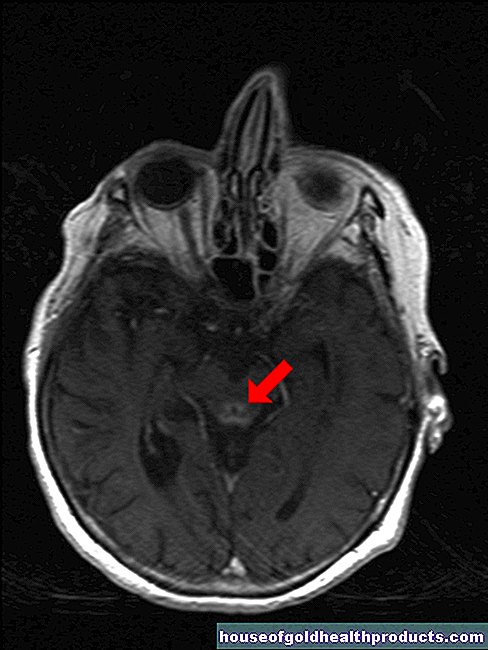
The most important way to diagnose fibrous dysplasia is through an X-ray examination. It is not uncommon for an X-ray to lead the suspicion to the rare disease, for example after a broken bone. The doctor sees an often spindle-shaped, frosted glass-like, thickened area in the affected bone, where the bone structure has been replaced by connective tissue. Sometimes the changes look like bone cysts. The outer bone layer (cortex) is also usually thinner than in a healthy bone. A computed tomography (CT) scan helps the doctor take a closer look at the changes. The person examined lies in a special device that takes very precise x-rays of the body layer by layer in the form of cross-sectional images. Another imaging technique is skeletal scintigraphy. This nuclear medicine examination reveals changes in bone metabolism. If polystotic fibrous dysplasia is suspected, skeletal scintigraphy will help track down all of the affected bones (foci).
If only a single bone is changed (monostotic fibrous dysplasia), the correct diagnosis using imaging techniques can sometimes be difficult, as some other diseases are similar (e.g. bone cyst, benign fibrous histiocytoma, hemangioma, chondrosarcoma). In this case, the doctor takes a tissue sample from the changed area (biopsy), which is then examined under a microscope. In fibrous dysplasia, there is a typical structure made of connective tissue of varying density, containing collagen, traversed by small trabeculae made of bone tissue (bone trabecula). Only a few “primordial bone cells” (osteoblases) are found on their surface, but collagen fibers are arranged in rays.
Fibrous dysplasia: treatment
A causal treatment is not possible in fibrous dysplasia. If the thighbone or the shin is affected, it can make sense to relieve the bone with a splint, for example. In this way you can prevent possible bone fractures in the unstable areas. However, this should be discussed with an experienced orthopedic surgeon, as further bone deformations sometimes occur, especially during growth. It may therefore make more sense to strengthen the surrounding bones and muscles as part of physical therapy with strength exercises.
If fibrous dysplasia causes severe pain, it can be contained with pain relievers (analgesics). A relatively new therapeutic approach are so-called bisphosphonates - drugs that are also used to treat osteoporosis and other bone diseases. They appear to have a beneficial effect on the bone pain and fracture tendency that accompany fibrous dysplasia.
In rare cases, fibrous dysplasia is so pronounced that, for example, bones in the face are severely deformed; then an operation can be useful for aesthetic reasons.
Fibrous dysplasia: disease course and prognosis
Overall, fibrous dysplasia has a good prognosis. The course can be slightly different. In some patients, the herd increases in stages during puberty, so that the affected bones are further distended; as a rule, however, no new flocks emerge. In adulthood at the latest, however, the fibrous dysplasia usually comes to a standstill and the bone is no longer remodeled.
The fact that fibrous dysplasia develops into a malignant bone tumor (osteosarcoma) is very rare and occurs in less than one percent of cases. Severe courses are just as rare, for example when fibrous dysplasia affects the cranial bones and these are so deformed that they restrict the function of the brain.
Tags: desire to have children news sports fitness