Gestational diabetes
and Martina Feichter, medical editor and biologistDr. med. Julia Schwarz is a freelance writer in the medical department.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Gestational diabetes is the most common concomitant disease of pregnancy. It occurs in about four out of ten pregnant women. Most of the time it is largely symptom-free. However, gestational diabetes can lead to serious complications for both mother and child. Read more about the causes, symptoms, therapy and prognosis of gestational diabetes!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. O24
What is gestational diabetes?
Gestational diabetes is a form of diabetes (diabetes mellitus) that is first diagnosed during pregnancy. It is sometimes referred to as type 4 diabetes. If the diabetes already existed before pregnancy, this is not referred to as gestational diabetes.
The transition between a slightly elevated blood sugar level and gestational diabetes is fluid. There is no defined threshold that marks the limit. Because pregnancy changes the metabolism, so that the sugar is absorbed from the blood into the body cells more slowly after a meal than in non-pregnant women: Slightly elevated blood sugar levels are therefore not uncommon in many cases in pregnant women.
By the way: Gestational diabetes is sometimes abbreviated as SS diabetes.
Gestational diabetes: causes and risk factors
The exact causes and mechanisms that lead to gestational diabetes are not yet known. However, experts assume that they are largely similar to those of type 2 diabetes mellitus.
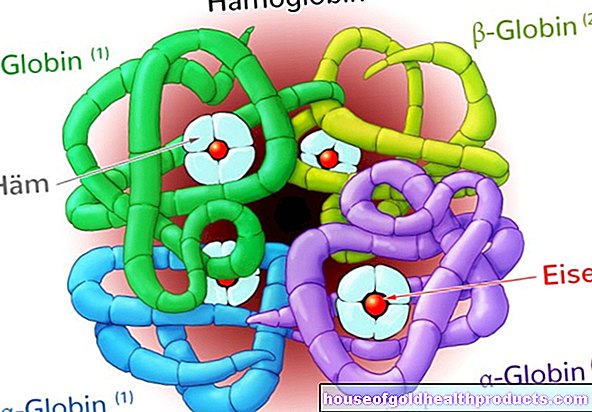
Apparently, affected women have chronically decreased insulin sensitivity even during pregnancy. This means that the body's cells respond less to the blood sugar lowering hormone insulin than normal. This increases in the course of pregnancy because from the 20th week of pregnancy the cells generally become less sensitive to insulin (physiological insulin resistance). Natural hormonal changes in pregnancy play a role in this:
Especially in the second half of pregnancy, the female body produces large amounts of the hormones estrogens, progesterone, cortisol, placental lactogens and prolactin. Among other things, these hormones ensure that larger amounts of energy are made available in the body - for optimal development of the child.
At the same time, the effect of the blood sugar lowering hormone insulin is reduced. Similar to type 2 diabetes, insulin resistance develops. Normally, pregnant women still produce enough insulin to counteract high blood sugar levels. In women with gestational diabetes, however, the insulin production is not sufficient to meet the additional requirement.
When is your risk particularly great?
Researchers have identified several risk factors for gestational diabetes. These include:
Overweight: Overweight and severe overweight (obesity = obesity) are mostly the result of an unhealthy, high-fat and high-sugar diet and a lack of exercise. Women with obesity, in particular, are at a higher risk of gestational diabetes (and type 2 diabetes in general). Abdominal fat cells in particular release certain messenger substances that promote insulin resistance in the body's cells (such as adipokines). The tissue then only responds in a weakened manner to the insulin produced by the pancreas. This means that larger amounts of insulin are required in order to be able to absorb the sugar circulating in the blood into the cells.
Women who gain excess weight during pregnancy are also at increased risk of gestational diabetes.
Family diabetes: Pregnant women who have a 1st degree relative (parent or sibling) with diabetes are more prone to gestational diabetes. This suggests that genetic factors (predisposition) are involved in the development of diabetes.
Previous pregnancy with gestational diabetes: Mothers-to-be who had SS diabetes in a previous pregnancy are more likely to get it again. Experts put this probability at 30 to 70 percent.
Previous birth of a very large or malformed child: The risk of gestational diabetes is increased if a pregnant woman has given birth to a child with a birth weight of more than 4,500 grams. The same applies to pregnant women who have given birth to a child with severe malformations in the past.
Recurrent miscarriages: Women who have three or more miscarriages in a row are more prone to gestational diabetes.
Older age: Pregnant women of older ages have an increased risk of gestational diabetes. Experts are discussing what is meant by "older" age. The information in the specialist literature varies between> 25 years and> 35 years.
Diseases with insulin resistance: There are various diseases that can be associated with insulin resistance - i.e. with a reduced response of the body cells to insulin. This applies, for example, to polycystic ovarian syndrome (PCO). Pregnant women with such diseases may have an increased risk of SS diabetes.
Certain drugs: Some drugs have a negative impact on sugar metabolism. These include, for example, beta blockers (blood pressure lowerers), glucocorticoids ("cortisone") and some antidepressants. The use of such drugs is considered a risk factor for gestational diabetes.
Ethnicity: A higher risk of gestational diabetes is observed in women from Central America, Africa, the Middle East and South and East Asia.
Gestational diabetes: symptoms
In most cases, gestational diabetes is largely asymptomatic. The typical symptoms of diabetes mellitus such as severe thirst (polydipsia), frequent urination (polyuria), fatigue and weakness are often only very mild and are interpreted differently in connection with pregnancy. However, the following signs can indicate gestational diabetes:
- Frequent urinary tract infections or vaginal infections: The sugar in the urine provides bacteria and fungi with good conditions to multiply.
- Increased amount of amniotic fluid: the gynecologist can detect such a polyhydramnios with an ultrasound.
- Excessive increase in weight and size of the unborn child: This macrosomia is due to the abnormally high blood sugar level of the expectant mother.
- High blood pressure (arterial hypertension): It often occurs with gestational diabetes.
Gestational diabetes: examinations and diagnosis
The right contact person for suspected gestational diabetes is a specialist in gynecology and obstetrics.
As part of the prenatal care, the doctor will generally ask the expectant mother about any complaints and abnormalities. Symptoms such as severe thirst, tiredness, dizziness or repeated urinary tract infections can indicate gestational diabetes, but they can also have other reasons.
A physical examination (with blood pressure measurement, weight determination, etc.) can help clarify such complaints. But it is also part of a routine prenatal check-up.
Tests for gestational diabetes
In addition, all women are usually tested for diabetes or impaired glucose tolerance in the 24th to 28th week of pregnancy (SSW). Usually the oral glucose tolerance test (oGTT) is used for this. In pregnant women with risk factors, the diabetes addiction test can be carried out in the first trimester of pregnancy. If the result is negative, it should be repeated in the 24th to 28th week of pregnancy; if the result is negative again, in the 32nd to 34th week of pregnancy.
The glucose tolerance test consists of a pre-test and the actual "diagnostic test":
During the pre-test (50-g-oGTT), the pregnant woman drinks a glass of water in which 50 grams of glucose have been dissolved beforehand. An hour later, her blood is drawn from a vein in her arm to check blood sugar levels. If its value is below 7.5 mmol / l (below 135 mg / dl), the result is normal. This ends the glucose tolerance test.
However, if the blood sugar level is above this limit value, the result is conspicuous (but not yet proof of gestational diabetes!). For further clarification, the woman receives a new examination appointment for the more complex 75-g-oGTT. For this, the pregnant woman has to be sober. So she must not have eaten or drunk anything (except for still water) at least eight hours beforehand.
The 75-g-oGTT begins with a blood sample and blood sugar test (fasting blood sugar). Then the pregnant woman drinks a sugar solution with 75 grams of dissolved sugar. Both after one and after two hours, your venous blood will be drawn to determine your blood sugar level (1-hour and 2-hour blood sugar). If one of the three measured blood sugar values exceeds certain limit values, the diagnosis "gestational diabetes" is established:
- Fasting blood sugar: 5.1 mmol / l (92 mg / dl)
- 1-hour blood sugar: 10 mmol / l (180 mg / dl)
- 2-hour blood sugar: 8.5 mmol / L (153 mg / dL)
Other common diabetes testing methods are not suitable for diagnosing gestational diabetes. This includes measuring glucose in the urine and determining the HbA1c value or fasting blood sugar.
By the way: The costs for the oral glucose tolerance test (preliminary and diagnostic test) are covered by the statutory health insurance companies.
Gestational diabetes: treatment
Most women with gestational diabetes can normalize their blood sugar levels by changing their diet. Physical activity is also useful. If the two do not work together sufficiently, insulin injections are necessary.
Blood sugar-lowering drugs in tablet form (oral antidiabetic drugs) have not yet been approved for pregnant women. Because it is not certain whether they might not harm the child. In some other countries, tablets containing the blood sugar lowering drug metformin may also be given to pregnant women if the high blood sugar level cannot be reduced sufficiently with insulin injections. In Germany they are prescribed (despite the lack of approval) in exceptional cases for overweight pregnant women after adequate information.
Gestational diabetes: nutrition
After diagnosing gestational diabetes, expectant mothers should receive individual nutritional advice. The change in diet has the following goals:
- Lowering blood sugar levels to a healthier level, which at the same time should avoid complications such as hypoglycaemia
- Weight gain as recommended during pregnancy (depending on weight and body mass index before pregnancy)
- normal growth of the unborn child
The nutrition plan should take into account the eating habits, the daily routine and the body weight of the pregnant woman.
In total, women with gestational diabetes should consume 1,800 to 2,400 kilocalories per day. This amount of energy should be divided among the main nutrients as follows:
- 40 to 50% carbohydrates: Slowly absorbable carbohydrates should be preferred, such as whole grains. Quickly absorbed sugars such as white flour products, confectionery and fruit juices, on the other hand, are unfavorable: They cause blood sugar to rise excessively quickly and sharply. In addition, at least 30 grams of fiber should be consumed every day (whole grains, legumes, fruits, vegetables).
- 30% fats: In general, pregnant women (and non-pregnant women) should prefer vegetable fats and oils to animal ones.
- 20 to 30% protein: Prefers low-fat milk and milk products as well as low-fat meat and sausage products.
It makes sense if the pregnant woman eats five to seven small meals (instead of a few large ones). In this way, blood sugar spikes can be avoided after a meal. In the late evening, a small, carbohydrate-rich late meal should be taken. This prevents a nocturnal lack of energy.
When putting together the menu, attention should also be paid to an adequate supply of vitamins and minerals.
Overweight pregnant women (with and without gestational diabetes) should not adhere to a strict diet! This could endanger the child's care and development. Instead, the daily calorie intake should be reduced to an acceptable level in consultation with your doctor or nutritionist.
By the way: If gestational diabetes is only treated with a change in diet (without insulin), the women affected should check their blood sugar level with a blood sugar meter several times a week.
Gestational diabetes: physical activity
Pregnant women with gestational diabetes should also get regular exercise. You may even be able to exercise (in moderation). The prerequisite is, of course, that nothing speaks against it from a medical point of view.
Regular physical activity can help reduce high blood sugar levels. Which and how much activity is advisable in individual cases depends on how resilient the woman is and how the pregnancy goes. Most suitable are sports such as cycling, walking or swimming. But regular brisk walks also have a positive effect. Every pregnant woman should seek advice on this from her doctor.
Gestational diabetes: insulin
If a change in diet and physical activity do not bring the desired result in gestational diabetes, the doctor will also prescribe insulin. In most cases, intensified insulin therapy is carried out:
The affected women inject long-term insulin (delay insulin) under their skin in the evening or in the morning and evening. It covers the basic need for this hormone. Before a meal, an injection with a short-acting insulin is usually necessary in order to absorb the expected increase in blood sugar (as a result of food consumption). To choose the right insulin dose and to check the sugar metabolism, a blood sugar test is necessary several times a day.
Before starting insulin therapy, women with gestational diabetes should receive training. You need to learn how to properly measure blood sugar, interpret the readings, choose the right dose of insulin, and give yourself the right injections. Pregnant women should also know about possible complications and countermeasures. Every diabetic who injects insulin should always have some glucose with her - in case of sudden hypoglycaemia.
By the way: Only rarely is an insulin pump used instead of intensified insulin therapy in the case of gestational diabetes. This can be the case, for example, if a pregnant woman needs high doses of insulin and has severe insulin resistance.
Gestational diabetes: disease course and prognosis
Successful treatment for gestational diabetes usually only requires a change in diet (and possibly more exercise). For the vast majority of women affected, the pregnancy is otherwise normal and they give birth to a healthy child. After the birth, gestational diabetes usually disappears on its own.
Nevertheless, pregnancy with gestational diabetes is classified as a high-risk pregnancy. The increased blood sugar level can cause various complications and consequences for mother and child:
Preeclampsia, eclampsia, and HELLP syndrome
Poorly controlled gestational diabetes favors the development of high blood pressure (hypertension) during pregnancy. In some women, high blood pressure is accompanied by protein excretion in the urine (proteinuria) and water retention in the tissue (edema). This triad of symptoms during pregnancy is also known as preeclampsia. Women with gestational diabetes (or other diabetes diseases) are more prone to it than non-diabetics.
Preeclampsia is a preliminary stage of the potentially life-threatening clinical pictures of eclampsia and HELLP syndrome. Eclampsia is manifested by neurological disorders. Headaches, flickering vision and seizures can occur. The so-called HELLP syndrome can develop within a very short time (about an hour). HELLP stands for H = hemolysis (breakdown of blood cells), EL = elevated liver values and LP = low platelets. Severe upper abdominal pain, nausea and vomiting, and possibly diarrhea are common signs.
Eclampsia and HELLP syndrome also occur more frequently in patients with gestational diabetes than in healthy pregnant women.
Urinary tract infections
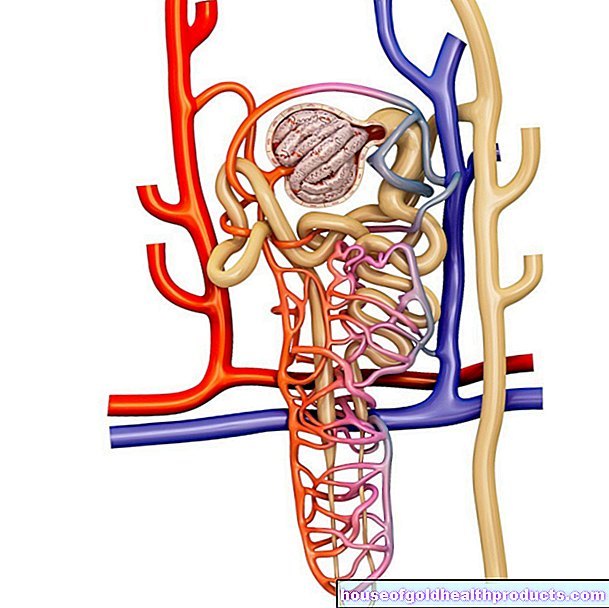
There is usually no sugar in the urine. It is different with gestational diabetes (and other forms of diabetes): If the blood sugar level is too high, sugar is excreted in the urine (glucosuria). This favors the spread of pathogens such as bacteria and fungi in the urinary tract of the pregnant woman - the germs use the sugar as food. As a result, women with gestational diabetes are more prone to urinary tract infections such as cystitis. This can lead to inflammation of the renal pelvis if the germs rise from the bladder via the ureters into the kidneys.
Dangerous blood sugar levels
Gestational diabetes can cause dangerous blood sugar levels. With pronounced gestational diabetes, dangerously high blood sugar levels can occur, especially after eating. This is especially true if the disease is left untreated. The large amount of sugar is then excreted through the kidneys and draws water with it. The women have to urinate a lot and lose important blood salts in the process. If left untreated, the dehydration and blood salt disorders can lead to a comatose state (hyperosmolar coma).
Even if gestational diabetes has to be treated with insulin, it can be dangerous - for example if the woman uses the insulin syringe incorrectly or not at all. If she injects too much insulin, there is a risk of severe hypoglycaemia.
By the way: expectant mothers who suffer from type 1 diabetes have to be careful. The need for insulin changes during pregnancy. At the beginning it tends to decrease, whereas as the pregnancy progresses, more and more insulin is required. It is best to talk to your diabetologist about the right treatment steps. Without proper therapy adjustment, there is a risk of severe blood sugar imbalances.
Premature birth and miscarriage
Women with gestational diabetes are at an increased risk of premature birth and miscarriage. For example, maternal infections or too much amniotic fluid (see below) can promote premature birth.
Too much amniotic fluid (polyhydramnios)
Women with gestational diabetes (or other forms of diabetes) often have too much amniotic fluid (polyhydramnios). If the uterus cannot hold the unusually large amount of fluid, it can lead to premature rupture of the bladder. The doctor can use an ultrasound scan to determine whether a pregnant woman has excessive amounts of amniotic fluid.
Excessive growth in the child (macrosomia)
The unborn child's body reacts to the increased blood sugar levels in pregnant women with gestational diabetes (or other forms of diabetes) with an excess of insulin (hyperinsulinism). The result is that the child grows excessively (macrosomia): Such macrosomal children weigh more than 4,000 grams at birth and their size can also cause problems during childbirth.
For example, the child's shoulder can get caught in the mother's pelvis (shoulder dystocia). Then there is a risk that the child will not get enough oxygen. Doctors and midwives must therefore intervene quickly - with the risk of birth injuries to mother and child.
Sometimes a vaginal delivery is not even attempted in the case of very large babies, but a caesarean section (sectio caesarea) is made straight away.
Other complications in the child
Although macrosomal newborns are larger and heavier than average, they are functionally immature. They therefore often suffer from breathing problems (respiratory distress syndrome) due to the not yet fully developed lungs. Macrosomia can also lead to increased bilirubin levels and clotting disorders. Elevated bilirubin levels in the blood can trigger newborn jaundice (jaundice).
The increased insulin production of the unborn child as a reaction to the high levels of sugar in the mother's blood can lead to hypoglycaemia (low blood sugar) after birth.
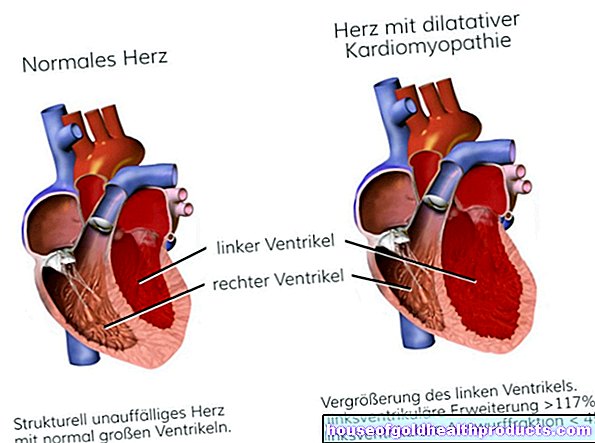
Especially with early onset gestational diabetes (in the first trimester), which is not discovered and treated, there is an increased risk of malformations, for example in the child's heart.
Long-term consequences for mother and child
About four out of ten women who have had gestational diabetes before will get it again in another pregnancy. This is especially true if there are other risk factors (such as being very overweight).
In addition, more than half of all women who had gestational diabetes will develop persistent diabetes (diabetes mellitus) within the next ten years. This danger exists especially if gestational diabetes had to be treated with insulin. Therefore, even after gestational diabetes has subsided, women should have their blood sugar levels checked regularly and reduce risk factors such as obesity.
These measures can also be advisable for children: The offspring of mothers with gestational diabetes also have an increased risk of diabetes mellitus. This can already show in the first two decades of life. At this young age, overweight (or obesity), high blood pressure and metabolic syndrome often develop. The risk of these diseases is higher than in children whose mothers did not have gestational diabetes.
Additional information:
Guidelines:
- S3 guideline "Gestational diabetes mellitus (GDM)" of the German Diabetes Society and the German Society for Gynecology and Obstetrics (as of 2016)
- Guideline "Gestational diabetes" for patients, pregnant women and those interested in diagnosis, treatment and follow-up care; German Diabetes Society and German Society for Gynecology and Obstetrics (as of 2012)