Vena cava syndrome
Florian Tiefenböck studied human medicine at the LMU Munich. In March 2014, he joined as a student and has supported the editorial team with medical articles ever since. After receiving his medical license and practical work in internal medicine at the University Hospital Augsburg, he has been a permanent member of the team since December 2019 and, among other things, ensures the medical quality of the tools.
More posts by Florian Tiefenböck All content is checked by medical journalists.The vena cava syndrome is the name for a specific form of circulatory disorders. It occurs when the pressure on the vena cava no longer allows blood to flow freely to the heart. Pregnant women are particularly affected. The child presses on the inferior vena cava (Latin: vena cava inferior), the blood pressure drops and the expectant mother can even pass out. Read everything about life-threatening vena cava syndrome here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. I87

Vena cava syndrome: description
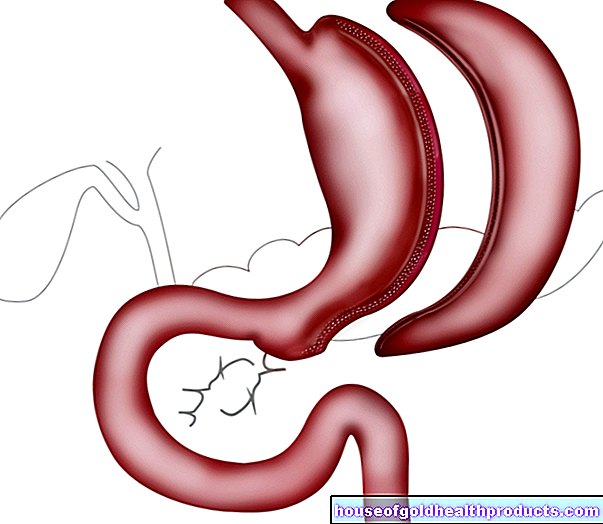
Vena cava syndrome is a circulatory problem that mainly affects pregnant women. If the heavily pregnant woman lies on her back, the uterus with the unborn child can press the inferior vena cava (compression) and interrupt the flow of blood from the lower half of the body to the heart. This is why doctors also speak of vena cava compression syndrome. Since the child increases in size and weight significantly in the last months of pregnancy, women suffer from vena cava syndrome, especially towards the end of their pregnancy (3rd trimester).
The syndrome can also be triggered by swellings and tumors - both benign and malignant. Liver cancer in particular presses the inferior vena cava. Doctors then speak of the inferior vena cava syndrome. If a tumor, for example of the mediastinum, compresses the superior vena cava, the symptoms are summarized under the term superior vena cava syndrome (also: upper congestion). In the case of such space-occupying diseases, the symptoms usually arise insidiously, but are constant (whereas the vena cava syndrome in pregnant women occurs suddenly and can be treated with appropriate measures (change of position).
Strictly speaking, the vena cava syndrome is not an independent disease. Rather, it describes a complex of several symptoms of reduced blood reflux such as a sudden drop in blood pressure up to fainting. In the case of pregnant women, the vena cava syndrome can also cause undersupply for the child. In extreme cases, a life-threatening situation develops for both of them. Since the inferior vena cava can also be completely closed (occluded) by the pressure of the uterus, some doctors use the term vena cava occlusion syndrome.
About 30 to 40 percent of pregnant women suffer from vena cava syndrome during the second or especially third trimester.
Vena cava syndrome: symptoms
There are a number of ailments people can suffer from. The following symptoms may occur in pregnant women with vena cava syndrome:
- sudden drop in blood pressure
- dizziness
- sweat
- cold sweaty skin
- nausea
- Edema on the legs
- paleness
- Fainting (or feeling of beginning syncope)
- Palpitations (tachycardia), later also a strongly slowed heartbeat possible (bradycardia)
- Shortness of breath
Not all of these symptoms have to appear. However, if the vena cava syndrome is not resolved quickly, the signs will get worse. In vena cava compression syndrome, the baby also suffers from poor blood circulation. Because this means that enough oxygen can no longer be transported to the fetus (fetal hypoxia). In extreme cases, those affected develop cardiovascular shock and the unborn child dies.
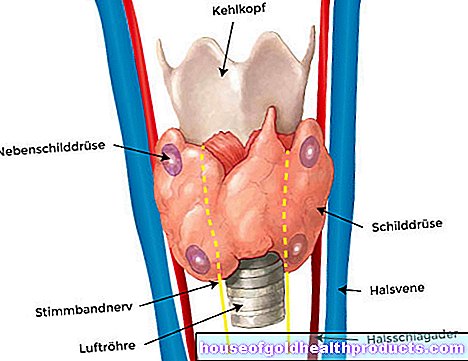
Signs of upper stagnation of influence
In the vena cava syndrome of the superior vena cava, the neck veins in particular are congested. But the veins on the arms and head can also protrude. Many patients also suffer from a feeling of pressure in the head or even headaches. If the pathological swelling or the tumor presses on other organs, further symptoms can arise: if the esophagus is narrowed, for example, difficulty swallowing (dysphagia). If the windpipe is compressed, the shortness of breath (dyspnoea) increases. Depending on the symptoms that occur, the vena cava syndrome of the superior vena cava is divided into five degrees of severity (from mild to no longer treatable).
Vena cava syndrome: causes and risk factors
In vena cava syndrome, the lower (inferior vena cava) or upper vena cava (superior vena cava) is compressed. Deoxygenated blood flows through the large vena cava from the lower and upper areas of the body back to the right heart (right atrium and right ventricle; the confluence of the vena cava inf. And sup.) Is located on the right atrium. From there, the blood goes to the lungs, where it is oxygenated and eventually flows back to the heart. The left ventricle pumps the now oxygen-rich blood back into the body's circulation. The inferior vena cava is located on the right in front of the spine and therefore behind the uterus in pregnant women. The superior vena cava runs in close proximity to the lungs, trachea and esophagus.
Vena cava syndrome in pregnancy
During the nine months of pregnancy, the child grows steadily in the maternal uterus. As a result, the weight of the fetus also increases. If the mother lies on her back, the uterus with the heavy child in it presses on the inferior vena cava. As a result, the blood can no longer flow freely back to the right heart as usual. As a result, the amount of blood the left heart can pump into the body also decreases (by up to 30 percent of the normal circulating blood). So the blood pressure drops (hypotension). In the supine position, it takes about three to seven minutes for the blood pressure to drop measurably.
The body tries to compensate for the vena cava syndrome with various mechanisms. For example, the heart beats faster (tachycardia) in order to be able to pump the reduced amount of blood quickly enough into the circulation. In addition, very small arteries in the terminal flow path (for example the fingers) narrow, which means that less oxygen-rich blood can flow through them. Instead, this is redirected to important organs (e.g. the brain). However, the vessels of the uterus also contract (placental insufficiency). As a result, less oxygenated blood flows to the child. There is a threat of an undersupply of the fetus, which in the worst case can end in its death.
Risk factor cancer
In addition to pregnancy, there are other circumstances that can trigger vena cava syndrome. In general, any swelling in the abdomen can press the inferior vena cava. Since this is on the right in front of the spine, advanced, malignant liver diseases (liver cancer, liver metastases) or right-sided kidney diseases (kidney cancer) in particular can cause a lower vena cava syndrome. In connection with liver diseases, so-called ascites (ascites) also often occur. This accumulation of fluid in the abdomen can also lead to a vena cava compression syndrome in an advanced stage.
The most common cause of upper vena cava syndrome is lung cancer. Cancer settlements (metastases) from other organs are less responsible. However, cancer of the lymph glands or thyroid gland can also lead to a vena cava syndrome. Very rarely does a benign swelling such as the goiter (goiter) press on the superior vena cava.
The symptoms of vena cava syndrome can also result from blood clots (thrombi) in the vena cava. Such thrombi often also arise as a result of long-term compression of the vein.
Vena cava syndrome: diagnosis and examination
Diagnosing vena cava syndrome in pregnant women is usually quite simple. The specialist in gynecology and obstetrics (gynecologist) or experienced midwives can usually recognize a vena cava syndrome quickly.
If you suffer from circulatory disorders during pregnancy, you should definitely consult a doctor. If you are not pregnant but suffer from typical symptoms of the vena cava syndrome, it is best to make an appointment with your general practitioner or internist (specialist in internal medicine). If you are already aware of illnesses (e.g. cancer), your attending doctor will help you. Depending on the subject, the doctor asks questions such as:
- Do you have any previous illnesses?
- When and how often do you suffer from circulatory problems?
- Did you lose consciousness for a short time as a result? Did you go black?
- Did you have blood pressure problems before you became pregnant or before you got cancer?
- Do the symptoms occur more frequently in certain situations, for example when you lie on your back for a long time?
- Does the discomfort get better when you lie down or sit down differently?
If a vena cava syndrome of the superior vena cava is suspected, the doctor pays particular attention to blocked veins in the neck region or a whistle when inhaling (stridor, indication of a narrowing of the trachea). It also listens to the heart (auscultation) and measures both blood pressure and pulse. Sufferers are usually examined first sitting or standing and then lying on their back. If the circulatory values deteriorate as a result, this provides a decisive indication of the vena cava syndrome.
With the help of an ultrasound (sonography), the doctor can check organs in the abdomen and rule out other causes of a drop in blood pressure (especially internal bleeding).
Child's heartbeat
In the case of vena cava syndrome in pregnant women, the doctor performs a so-called cardiotocography (CTG). The device records the unborn child's heartbeat (and contractions). The mother lies on her back during the examination. If there is an inadequate blood supply to the fetus due to a vena cava syndrome, this is shown in the CTG. Typically the heart beats more slowly (bradycardia). Sometimes the fetal heart rate only drops into a critical range from time to time due to the vena cava syndrome. The CTG curve drops off in the shape of a trough. Then doctors speak of sporadic or prolonged decelerations.
Diagnosis in cancer
The ultrasound device also plays a decisive role in cancer. In these cases, the vena cava syndrome usually only occurs in the advanced stage of an already known disease. Here, too, imaging examinations (computed tomography, sonography) help rule out other reasons for the symptoms. It should also be noted that the vena cava syndrome of the superior vena cava is significantly less position-dependent than the vena cava syndrome of the inferior vena cava.
Vena cava syndrome: treatment
Leaving the supine position is the first and foremost measure in vena cava syndrome. In many cases, it is enough to simply sit up in an upright position. Often, however, the patients are turned on their left side. Sometimes the right hip is also raised and a pillow or something similar is placed under it. This makes it easier for the blood to flow back to the heart.
If the vena cava syndrome leads to a cardiovascular shock (loss of consciousness, rapid heartbeat, barely measurable blood pressure) despite being repositioned to the side, the emergency doctor must be alerted immediately. After admission to an intensive care unit, the circulation is stabilized, among other things, by administering fluids. Doctors also examine the unborn child. In life-threatening situations, a caesarean section follows immediately.
The vena cava syndrome in malignant tumors usually has to be treated surgically. Until then, however, special reclining positions (sideways, sitting) will also help to reduce the discomfort. Sometimes doctors insert a stent - a sturdy wire mesh or tube that protects the vena cava from being compressed. Radiation can also help alleviate the symptoms, as it shrinks the tumor.
Vena cava syndrome: disease course and prognosis
The symptoms of a lower vena cava syndrome can usually be eliminated by a quick repositioning. They rarely take on life-threatening proportions for mother and child. However, such processes can also be successfully treated with immediate hospitalization and appropriate therapy. In some vena cava syndromes, the main artery (aorta) is also compressed.However, it has a much more stable vessel wall and usually only narrows slightly. Doctors speak of the aortocaval compression syndrome.
In vena cava syndrome of the superior vena cava, the symptoms usually increase over time. However, they can also decrease again if, after some time, new vessels ("bypass circuits") have formed that bridge the compression.
Prevent vena cava compression syndrome
To prevent vena cava syndrome, pregnant women should avoid prolonged flat supine positions from the second trimester onwards. Change your lying position regularly. The left side position is particularly advantageous (but not permanently and exclusively). This moves the uterus away from the inferior vena cava, which is more in the right half of the body. Place flat pillows under the right side of your body to help you lie on your side. Special side sleeper or pregnancy pillows can also prevent vena cava syndrome.
Tags: drugs sex partnership symptoms




















.jpg)