Palliative medicine - pain therapy
Updated onMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Relief of discomfort, especially pain, is a main goal of palliative medicine. A whole range of drugs is now available for pain therapy. Learn more about the possibilities, advantages and disadvantages of drug-based pain therapy.

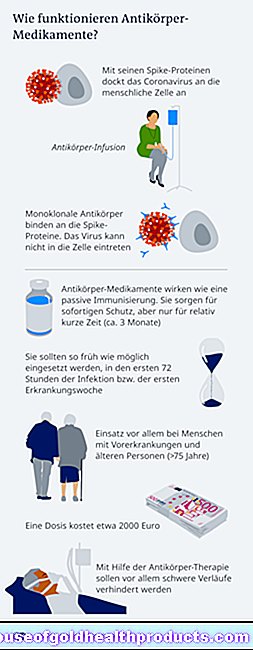
Patients in advanced stages of cancer or with other serious illnesses often suffer from severe pain, against which simple measures such as the application of cold or heat can no longer be used. Then the use of effective pain relievers (analgesics) is necessary. The World Health Organization (WHO) has developed a step-by-step scheme for this drug-based pain therapy, which is intended to help doctors treat patients optimally according to their needs.
Pain Management: WHO DNA Rule
WHO experts recommend the so-called DNA rule for drug pain therapy:
- D = By mouth: Oral painkillers should be preferred as far as possible (for example over painkillers that have to be injected). Administration via the anus (rectal), under the skin (subcutaneous), or as an infusion into a vein (intravenous) should be considered if oral administration is not possible.
- N = After the clock: The painkillers should be given at fixed time intervals depending on the duration of action - whenever the effect of the previous administration ends.
- A = analgesic scheme: When prescribing painkillers, the so-called WHO level scheme should be taken into account.
WHO level scheme for pain therapy
The WHO graduated plan for drug pain therapy is intended to provide assistance in the treatment of tumor pain and other chronic pain. It provides for such pain to be relieved initially with painkillers of the first stage. If this does not succeed, analgesics of the second stage are used (possibly in addition). If this does not produce the desired result, doctors prescribe third-stage pain relievers (also often together with first-stage analgesics).
Level 1 pain relievers
The first stage provides simple painkillers - so-called non-opioid, i.e. non-morphine-like painkillers. In contrast to the opioids of WHO levels 2 and 3, non-opioid analgesics do not have a narcotic (anesthetic) effect and do not impair the patient's ability to perceive. In addition, they do not run the risk of becoming dependent. Some of these pain relievers are therefore also available without a prescription.
Examples of non-opioid pain relievers are paracetamol, metamizole and the so-called NSAIDs (nonsteroidal anti-inflammatory drugs) such as acetylsalicylic acid (ASA), diclofenac and ibuprofen. They have various degrees of pain-relieving (analgesic), fever-reducing (antipyretic) and anti-inflammatory (anti-inflammatory) effects.
Paracetamol and acetylsalicylic acid are not suitable for use in cancer pain according to the current practice guidelines of the German Society for Pain Medicine.
When dosing non-opioid analgesics, the so-called ceiling effect must be taken into account: Above a certain dose, the pain relief cannot be increased any further - at most, the risk of side effects increases if the dose is increased further.
The side effects of non-opioid analgesics (depending on the active ingredient or group of active ingredients) include, for example, impaired blood clotting, gastrointestinal ulcers and bleeding, nausea, dizziness or skin reactions.
Level 2 pain relievers
According to the WHO, the second stage of pain therapy is weak to moderately strong opioid pain relievers such as tramadol, tilidine and codeine. Opioids are good pain relievers, but have a narcotic effect, so they can impair perception and also make you addicted. Other side effects of weakly effective opioids are mainly constipation, nausea, vomiting, dizziness and fatigue.
According to the German Society for Pain Medicine, tramadol and tilidine should only be given briefly for days or weeks until a level III preparation should be changed.
A combination of weak opioids with first-level pain relievers can be useful because these have a different mode of action than opioids. This can significantly improve the overall pain relieving effect.
As with first-stage pain relievers, the ceiling effect can also occur with weak opioids.
Level 3 pain relievers
The third level of WHO pain therapy includes powerful opioids such as morphine, buprenorphine, fentanyl, methadone, oxycodone and hydromorphone. With the exception of buprenorphine, no ceiling effect is to be expected here, which means: The dose can be adjusted if necessary without an upper limit dose, which is very important, especially in the case of the most severe tumor pain. Hydromorphone is currently preferred because it has a good balance of potency and side effects. Morphine is also available in fast-acting forms such as nasal sprays or lozenges that can be used to treat sudden peaks in pain.
Highly effective opioids can be given along with first-stage pain relievers, if necessary. However, they should not be combined with one another (e.g. morphine and fentanyl) or with weak opioids of the second stage.
Almost all potent opioids cause persistent constipation as a side effect. Nausea and vomiting are also common. Other side effects include respiratory depression, sedation, itching, sweating, dry mouth, urinary retention or involuntary muscle twitching. Most side effects occur primarily at the start of therapy and when increasing the dose.
Co-analgesics and adjuvants
At all levels of WHO pain therapy, so-called co-analgesics and / or adjuvants can be given in addition to painkillers.
Co-analgesics are active ingredients that are not primarily used as pain relievers, but still have a good analgesic effect in certain forms of pain. For example, anticonvulsants are given for cramp-like or colic-like pain. Tricyclic antidepressants can help with (neuropathic) pain caused by nerve damage, which is accompanied by paresthesia and often burning.
The term adjuvants includes drugs that are used against side effects caused by painkillers. For example, laxatives for constipation and anti-emetics can help against nausea and vomiting - all three gastrointestinal symptoms are common side effects of opioids.
Efficient pain relievers
Opioids are the most effective pain relievers in palliative medicine. However, pain therapy with these highly potent active ingredients carries risks: Opioids can be addictive - less psychologically than physically (physically). There is a risk of addiction especially with highly effective opioids, i.e. painkillers of WHO level 3. They are therefore subject to the Narcotics Act (Germany, Switzerland) or the Addiction Act (Austria): Their prescription and dispensing are therefore very strictly regulated.
In contrast, the weakly effective opioids of WHO level 2 (at least up to a certain dose) can be prescribed on a normal drug prescription - with the exception of tilidine: Due to its high abuse potential, drugs containing tilidine with rapid release of active ingredients (i.e. especially drops and solutions) are dropped ) under the Narcotics Act or the Narcotics Act.
An exception applies in the German Narcotics Act for solid preparations with the active ingredient combination tilidine and naloxone, if tilidine is released with a delay (sustained-release preparation) and per divided form (approximately per prolonged-release tablet) no more than 300 mg tilidine (calculated as base) and at least 7, It contains 5 percent naloxone hydrochloride. The naloxone cancels the opioid effects of tilidine if the drug is improperly injected. In the case of (intended) oral use, on the other hand, it is broken down immediately on the way through the liver (first-pass metabolism), the main active ingredient tilidine can then develop its effect.
Palliative sedation
In palliative medicine, sedation is the drug-related reduction in a patient's level of consciousness (in extreme cases, up to unconsciousness). It can be a side effect of pain relief with opioids or it can be brought about in a targeted manner in order to spare patients unbearable pain, fear and other stresses in the last phase of life as far as possible. In the second case, doctors call this "palliative sedation". In the past, the term "terminal sedation" was also used for this because it was feared that sedation would shorten the patient's life. However, this is not the case, as studies have since shown.
Palliative sedation should, if possible, only be carried out with the consent of the patient and only if there is no other means of alleviating the patient's symptoms.
Various groups of active substances can be used for sedation: benzodiazepines (such as midazolam), neuroleptics (such as levomepromazine) or anesthetics (anesthetics such as propofol). Palliative sedation can be continuous or intermittent, i.e. with interruptions. The latter is to be preferred because it has the advantage that the patient experiences more awake phases in between, which make communication possible.
Palliative medicine: pain therapy carefully examined
The WHO generally recommends (i.e. also in palliative medicine) to make pain therapy as simple as possible. Patients should only be given pain medication if the symptoms cannot be relieved by other measures (such as physiotherapy, psychotherapy, etc.). The selection, dosage and duration of use of the analgesics depend on the needs of the patient and should be checked regularly for their (further) necessity. The advantages and disadvantages of administering various painkillers are carefully weighed up against each other.
This is especially true with regard to the risk of addiction (and the risk of other serious side effects) with opioids. The aim of palliative medicine is to make the last phase of life as pleasant as possible for seriously ill people. Pain management with opioids is sometimes the only way to achieve this goal - in consultation with the patient and his relatives.
Tags: first aid drugs stress