HPV
and Martina Feichter, medical editor and biologistFlorian Tiefenböck studied human medicine at the LMU Munich. In March 2014, he joined as a student and has supported the editorial team with medical articles ever since. After receiving his medical license and practical work in internal medicine at the University Hospital Augsburg, he has been a permanent member of the team since December 2019 and, among other things, ensures the medical quality of the tools.
More posts by Florian TiefenböckMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
The abbreviation HPV stands for the human papillomavirus. The pathogen causes sexually transmitted diseases and can manifest itself through warts on the skin and in the genital area. Most HPV infections heal unnoticed, but malignant tumors can occur long after infection. Men and women can contract HPV equally. Read more about HPV here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. A63B07
HPV: quick reference
- Contagion: mainly through direct skin or mucous membrane contact (sexual intercourse); Virus transmission via infected objects (sex toys, towels, etc.) as well as during birth (from the infected mother to the child) is also possible
- Possible secondary diseases: Depending on the HPV type, mainly skin warts, genital warts (genital warts), tissue changes (potential precancerous stages) and cancer (such as cervical cancer, mouth and throat cancer, anal cancer)
- Common symptoms: depending on the clinical picture; e.g. with genital warts reddish, brownish or whitish papules in the genital and anal region, possibly with sensation of wetness and itching; in cervical cancer, vaginal discharge and unexplained vaginal bleeding
- Investigations: physical examination, cell smear, colposcopy (in women), HPV test, biopsy (analysis of a tissue sample)
- Treatment: Depending on the clinical picture, icing, laser therapy, electrocautery, medication, surgical interventions
HPV: causes and risk factors
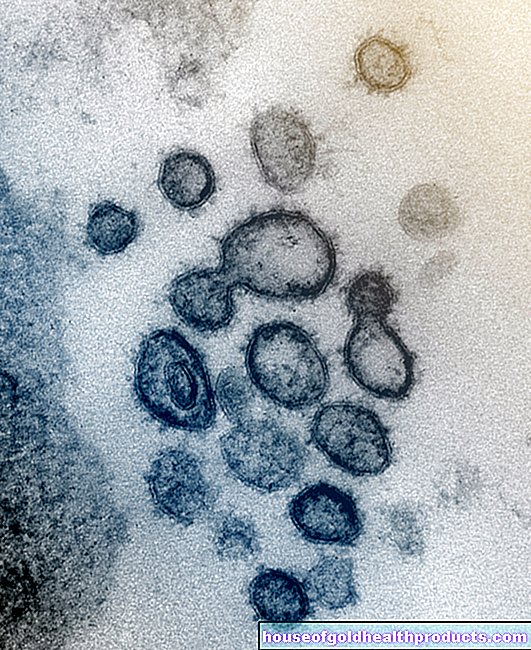
The human papilloma viruses (HPV) belong to the DNA viruses. Like the human genome, your genetic information is stored on a strand of DNA. HPV viruses need human cells to multiply. The infection works like this:
HPV viruses smuggle their genetic material into a human host cell (skin or mucous membrane cell) and force it to continuously produce new viruses. At some point the host cell bursts open (and dies in the process), releasing the many new viruses. They can then, in turn, attack new human cells.
HP virus life cycle
At the same time, with an HPV infection, the human genome can be changed in such a way that uncontrolled growths of the skin or mucous membranes (tumors) develop. They can become malignant cancer. The risk of cancer depends on the type of HPV.
The condylomata plana are flat varieties of genital warts on the external and internal genitals. HPV viruses 16, 18, 31 and 33 are considered to be the main culprits. They can lead to cell changes known as intraepithelial neoplasms. These cell changes are considered potential precursors of cancer and are classified according to where they occur:
- Cervical intraepithelial neoplasia (CIN): on the cervix (cervix = cervix)
- Vulvar intraepithelial neoplasia (VIN): on the vulva (= labia, clitoris and mons)
- Vaginal intraepithelial neoplasia (VAIN): in the vagina (vagina)
- Penile intraepithelial neoplasia (PIN): on the penis
- Perianal intraepithelial neoplasia (PAIN): in the anus region
- Anal intraepithelial neoplasia (AIN): in the anus
If you want to know more about the development and treatment of condylomas, read the article genital warts.
Cervical cancer
If mucosal cells on the cervix are chronically infected with high-risk HPV types, they can degenerate over time and form a malignant tumor.This does not happen with every infection, but rather rarely: According to statistics, fewer than one in 100 women infected with a high-risk HPV type will develop cervical cancer - an average of 15 years after the HPV infection.
So it takes a long time for the malignant tumor to develop. Women should therefore regularly go to the gynecologist for a check-up once a year: The so-called Pap smear from the cervix can reveal suspicious cell changes at an early stage.
Read more about the development, symptoms, treatment and prognosis of cervical cancer in the text cervical cancer.
Other cancers
In cervical cancer, the link to the HPV virus has been clearly demonstrated. But the development of cancer through HPV is also being investigated elsewhere. Oral intercourse, for example, can increase the risk of malignant growths in the throat and throat (such as throat cancer). Cancer growths in the genital and anal area such as vaginal cancer, vulvar cancer, penile and anal cancer can also be favored by an infection with high-risk HPV types. All of these cancers are much rarer than cervical cancer.
Skin warts
Some HPV viruses cause common skin warts called verrucae vulgares. They are the most common type of warts. There are various special forms of it, such as the butcher's wart. It occurs when working with raw meat in a damp and cold environment (especially with butchers) and is associated with the HPV virus type 7.
If an infection with HPV causes warts on the soles of the feet, they are usually plantar warts (verrucae plantares). The trigger is usually HPV 1. If plantar warts appear in large numbers in the form of wart fields, dermatologists speak of mosaic warts.
The flat warts that often appear in children are caused by HPV 3 or 10. Their technical name is Verrucae planae juveniles.
Warts in the mouth
Sometimes individual warts form in the mouth. They are called oral papillomas. Some of them have been shown to be linked to an HPV infection.
If warts or wart-like structures appear in the mouth, it may also be Heck disease (Heck disease or focal epithelial hyperplasia). These benign skin growths always occur in clusters and not individually. Its development is related to HPV 13 or 32. Heck's disease is rare among the European population, but occurs more frequently in other populations, for example among the indigenous peoples of Central and South America.
Epidermodysplasia verruciformis
This rare disease is a chronic HPV infection of the skin. It is also known as Lewandowsky-Lutz syndrome after its discoverer. It occurs in families and is one of the hereditary skin diseases. Due to a genetic defect, the HPV viruses can spread more easily among those affected. Various HPV types play a role in the development of epidermodysplasia verruciformis, including HPV 3, 5, 8 and 10.
HPV: signs (symptoms)
The human immune system can fight HPV viruses quite well in many cases, so that no or hardly any HPV symptoms occur. In the case of a latent HPV infection, the human papillomavirus can only be detected in the laboratory. In the case of a subclinical HPV infection, the virus-related skin / mucous membrane changes can only be made visible using special techniques.
If, on the other hand, HPV symptoms are visible to the naked eye, doctors speak of clinical HPV infection. The symptoms that HPV viruses cause depend on the type of virus and the disease in question.
Symptoms of genital warts (condylomata acuminata)
Genital warts or pointed condylomas can develop three to eight weeks (incubation period) after infection with certain HPV viruses. These are reddish, gray-brownish or whitish papules of the skin or mucous membrane of the genital and anal region. Their size varies between the size of a pinhead and several centimeters. Often the individual condylomas are close together and form so-called papillombeets.
In women, such HPV signs are mainly found in the area of the labia, at the posterior junction of the two large labia (posterior commissure) and in the anal region. The genital warts can also develop in the vagina and on the cervix. In men, these signs of HPV infection affect the penis and anal region.
Genital warts hardly cause any complaints. Sometimes, however, wetness and itching, burning and bleeding after intercourse are possible symptoms of HPV-caused genital warts. Pain, on the other hand, is only reported occasionally.
In rare cases, genital warts that have existed for years develop into so-called Buschke-Löwenstein giant condylomas (Condylomata gigantea). These cauliflower-like growths displace and destroy the surrounding tissue. The cells can degenerate and become cancer cells (verrucous carcinoma).
Symptoms of Condylomata Plana
Those affected develop inconspicuous, flat raised thickenings (warts) on the external genitals, in the anal canal and (in women) in the vagina and cervix. The warts usually appear in large numbers and are gray-white to reddish in color (like the mucous membrane).
Symptoms of intraepithelial neoplasia
Intraepithelial neoplasms cause no symptoms in many people. This applies, for example, to cervical intraepithelial neoplasia (CIN). In other cases there may be more or less obvious discomfort. For example, intraepithelial neoplasia in the vulva (VIN) can be accompanied by itching, burning and pain during sexual intercourse (dyspareunia), but it can also be symptom-free. Anal or perianala intraepithelial neoplasia (AIN and PAIN) causes itching in the anus area, as well as discreet bleeding from the anus and pain when defecating. Cell changes on the penis (PIN) can cause a velvety, irregular, shiny reddening in the area of the glans or the foreskin.
Symptoms of HPV-Associated Cancer
The most common cancer that HPV viruses are involved in developing is cervical cancer. Most affected women show no symptoms in the early stages of the disease. In other women, vaginal discharge and bleeding after intercourse, between menstrual bleeds, or after menopause indicate a possible tumor disease. However, these symptoms can also have other causes.
In the advanced stages of cervical cancer, women often report pain in the lower back or pelvis, urination, or bowel movements. Lymph congestion in the legs can also occur.
Sometimes other cancers are also linked to HPV. Symptoms depend on the location of the tumor and the stage of the disease. In the case of penile cancer, skin changes such as swelling or hardening of the glans or foreskin, easily bleeding areas of skin on the penis and sometimes foul-smelling discharge can occur. Vaginal cancer only becomes noticeable at an advanced stage with symptoms such as bloody discharge or vaginal bleeding (e.g. after sex).
Symptoms of skin warts
Skin warts can usually be recognized without any problems. As a rule, they do not cause any discomfort, apart from occasional itching, pressure or tension. Warts on the soles of the feet can also cause pain. Sometimes warts (like plantar warts) have small black spots. It is clotted blood from tiny skin capillaries.
Common verrucae are the size of a pinhead to a pea and have a rough, scaly surface. They tend to form on the back of the hand, on the fingers and nail edges as well as on the feet.
Plantar warts on the soles of the feet are pressed inward like nails by the weight of the body when walking or standing. This can cause such pain that those affected can barely walk.
Mosaic warts are about the size of a pinhead and white. They grow especially on the balls of the feet or under the toes. In some patients, they also cover the entire underside of the foot. Because they are flatter than plantar warts, they usually do not cause pain when walking or standing.
The verrucae planae juveniles, which occur mainly in children, are flat, skin-colored warts. They develop particularly on the face and back of the hands. When children scratch it, they spread the HPV virus in lines, so that the warts are also often arranged in lines.
Symptoms of warts in the mouth
Oral papillomas are single, cauliflower-like wart structures in the mouth. They are found preferentially on the hard or soft palate or on the uvula.
With Heck's disease, several round or oval papules develop on the oral mucosa. Children and young people are particularly affected.
Symptoms of Epidermodysplasia Verruciformis
In this disease, an abnormally large number of skin lesions that resemble flat, irregular warts (verrucosis) develop in a generalized manner, i.e. all over the body. The slightly scaling papules or plaques are reddish to brownish in color. Adolescents are particularly affected, and older adults less often. The risk of developing skin cancer is significantly increased, especially on open skin areas that are exposed to the sun.
HPV: diagnosis and examination
In most cases, HPV symptoms cannot be found with an infection. For the most part, the infection goes unnoticed. However, if the HPV viruses trigger signs of disease, these are usually typical changes in the skin or mucous membrane. However, some manifestations are so inconspicuous that they can only be made visible through special procedures. The necessary examinations are usually carried out by specialists, i.e., depending on the clinical picture, either dermatologists, gynecologists, urologists or ear, nose and throat specialists.
Medical history (anamnesis)
First, the doctor asks the patient about any symptoms that might be related to an HPV infection, for example:
- Where exactly are the complaints or skin changes?
- Is there genital itching or burning?
- Has there been any inexplicable bleeding?
Since sexual activity plays a decisive role in HPV, the doctor will also formulate specific questions about this: Has the sexual partner been changed frequently? Have you noticed any changes in the mucous membrane, possibly significant warts?
General risk factors such as smoking or medication are also noted. The doctor also asks about known previous illnesses. These may weaken the immune system and thereby promote an HPV infection.
Physical examination
The doctor usually examines the whole body. Most of the symptoms of HPV, namely warts on the skin, are easy to spot. Further examinations are then usually not necessary. If a skin wart appears suspicious, the doctor removes it and sends it to a laboratory for further examination.
Changes in the female genital area are usually discovered during preventive examinations. The vagina is scanned and then examined with a speculum ("mirror"). Palpation is important because specula sometimes cover deep-seated growths such as those caused by HPV viruses.
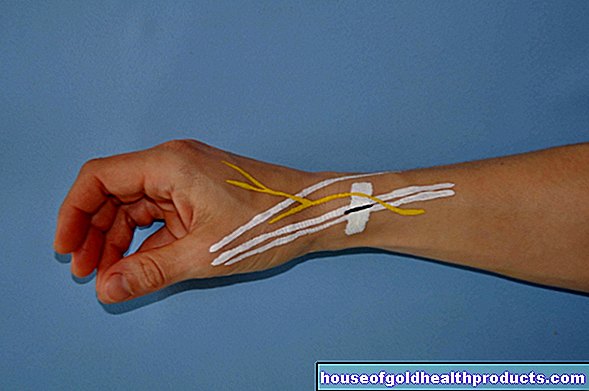
HPV-suspicious manifestations in the male genital area are usually recognizable and unambiguous with the naked eye. The specialist for this region of the body, the urologist, examines the glans of the penis, the urethral outlet (Meatus urethrae externus) and its enlargement located there (Fossa navicularis). Under certain circumstances, he spreads this area open so that the last two centimeters of the urethra can be examined.
HPV can also be found in the anal area. Since HPV-induced tumors can reach into the anal canal, some doctors perform a mirroring of the anal canal (proctoscopy).
Cell smear
In women over the age of 20, gynecologists regularly take a swab from the cervix for the early detection of cervical cancer. The surface of the cervix is first wiped off with a kind of brush using circular movements. The doctor takes the second smear from the cervical canal. The smears are then fixed on a glass plate with the help of a high-percentage alcohol solution, then colored and examined. This is not a special HPV smear to detect the virus, but an examination for suspicious cell changes that may result from an HPV infection (or for other reasons).
A scale developed by the Greek doctor Georges Papanicolaou is used to assess possible cell changes. This is why this examination is also called the Pap test.
Colposcopy
The colposcopy is to be understood as an extended reflection of the vagina. During this examination, the gynecologist also uses a so-called colposcope (Kolpo = vagina; scopie = observation), a kind of microscope. With up to 40x magnification, the doctor can see the smallest changes or bleeding in the cervix, cervix, vaginal walls and vulva. With the extended colposcopy, the doctor dabs two to three percent acetic acid on the mucous membrane. Changed upper cover layers swell up and stand out whitishly from the rest of the mucous membrane.
Another step is the so-called Schiller iodine test. The vaginal mucous membrane is dabbed with an iodine solution (four percent Lugol iodine solution). The healthy mucous membrane then turns brown-red due to the starch (glycogen) it contains. In contrast, cell layers that have been altered by HPV, for example, remain unstained.
biopsy
If the doctor discovers abnormalities during the smear or colposcopy, he can specifically remove tissue from the female genital area and examine it (biopsy). Depending on the location of the diseased mucous membrane, the tissue sample is scraped out with a sharp spoon (curettage) or a cone is cut from the vaginal tissue (conization).
HPV test
This test is used to detect an HPV infection and identify the type of virus. Its use on the cervix is best tested: the test result helps diagnose the malignant tumor or its precursors. The test is much less suitable for detecting an HPV infection in other parts of the body.
The HPV test is available in different versions. For the early detection of cervical cancer, it is currently only recommended for women aged 30 and over together with the Pap test. If you have an abnormal Pap test at a young age, a test for human papilloma viruses can also be useful. It can also help to monitor the success of therapy after treatment for precancerous stages of the cervix.
If you would like to know more about the procedure, significance and costs of this examination, please read the article HPV test.
HPV: treatment
HPV infections usually heal spontaneously because the immune cells kill the HPV viruses. Sometimes, however, existing diseases weaken the immune system and thus the fight against HPV. Hence, these need to be dealt with.
In general, the choice of HPV therapy depends on the type and extent of the HPV symptoms. Symptoms such as condylomas or skin warts can be treated in different ways. The HPV viruses themselves are rarely completely eradicated. As a result, relapses are common.
Icing (cryotherapy)
This HPV treatment option is used for superficial condylomas and skin warts. The doctor applies liquid nitrogen to the affected area of the skin with the help of a spray or a stick (cotton wool, metal), which kills the tissue. Sometimes a small bubble also forms. The application is usually repeated every one to two weeks. However, the HPV virus survives this procedure. In many cases, new warts form as a result.
Electrocautery
This treatment is also carried out by a doctor. Like icing, electrocautery can be used for condylomas and warts of the skin. The tissue changed by HPV is destroyed by an electric current. However, here too the HPV virus remains in the body and can trigger new skin changes at any time.
The electrocautery is also used after surgical removal of warts: the directly adjacent layers of skin and their vessels are charred. Although this reduces the risk of relapse, there is a high probability that a scar will form.
Operative procedures
Any HPV symptom can also be addressed surgically. Various instruments can be used for this. First, the affected area of the body is anesthetized locally. Then the growths can be cut out (excision) with a sharp spoon (curettage), an electric loop (loop electrosurgical excisional procedure, LEEP) or surgical scissors (scissors).
In the case of suspicious neoplasms (intraepithelial neoplasias, especially cervical) of the genital mucosa, a whole cone is often cut out (conization). Before that, however, you usually carry out several follow-up checks: the doctor checks every six months to see how the clinical picture is changing.If the abnormal area is enlarged and high-risk HPV has also been detected, the tissue must be removed. If the tumor has already been recognized as malignant, an operation will be carried out as soon as possible. However, if the patient is pregnant, attempts are made to delay the operation until after the birth. Depending on the stage of the cancer, the surgeon will extend the procedure accordingly. For example, in advanced cervical cancer, the entire uterus is removed (radical hysterectomy).
Some cancer patients receive radiation therapy and / or chemotherapy as an alternative or in addition to surgery.
Laser therapy
This possibility of treating HPV diseases is also one of the surgical procedures. The laser (e.g. CO2 or Nd: YAG laser) is used for all types of HPV warts. The growths are cut out and evaporated under local anesthesia. However, caution is advised: the smoke can spread the HPV viruses easily. It is therefore particularly important to provide adequate protection by means of a suction device and filter.
Medicines for HPV warts
There are some medications that can be used to treat genital or anal HPV warts. Some are administered by the doctor, others can be used independently by patients at home against the HPV symptoms. Careful and regular use of the medication is critical to the success of the therapy. Examples:
|
drug |
user |
Remarks |
|
Podophyllotoxin 0.15% cream |
patient |
|
|
Imiquimod 5% cream |
patient |
|
|
Trichloroacetic acid |
doctor |
|
In principle, there is a high risk of relapses (recurrences) with HPV infections. Therefore, the treated areas should be carefully checked and the doctor should be consulted at regular intervals.
HPV: disease course and prognosis
There is no classic HPV infection. It often goes unnoticed and heals without any consequences. If HPV symptoms occur, spontaneous healing is also possible. In general, most HPV infections heal within a few months. After two years, around 90 percent of all HPV infections are cured.
Certain HPV viruses last longer and even lead to cancer in only a few patients. This can happen years or decades after the HPV infection.
A healed HPV infection does not offer any protection against re-infection with the pathogen.
HPV: prevention
There is a lot of discussion about how to protect yourself from HPV infection. Prevention is not easy because HPV viruses are widespread and the risk of infection is therefore very high.
In general, it makes sense to ensure thorough hygiene and to strengthen the immune system. In order to reduce the risk of infection with normal skin warts, one should not walk around barefoot in swimming pools, saunas, public changing rooms and hotel rooms. If someone around has warts, you shouldn't share your towel, washcloth or socks (if you have warts on your feet) with them, for example.
To prevent HPV infections in the genital and anal area, you should always use a condom, especially if you have frequently changing sex partners. Safer sex does not offer reliable protection against HPV because the HPV virus can be transmitted by smear infection. However, condoms can reduce the risk of infection.
It has been established that the risk of HPV in men who are circumcised is lower than in those who are not.
HPV: vaccination
The Standing Vaccination Commission (STIKO) of the Robert Koch Institute recommends that all girls and boys between nine and fourteen years of age be recommended against HPV (preferably before their first sexual intercourse). Anyone who is still unvaccinated at the age of 15 should have the vaccination by their 18th birthday at the latest.
The main purpose of the HPV vaccination is to lower the risk of cervical cancer. It can also reduce the risk of some other cancers (vaginal cancer, penile cancer, etc.) and prevent genital warts from developing in both sexes.
It is not yet known exactly how long the vaccination protection lasts. Study results indicate that vaccinated girls / women are still effectively protected against HPV infection 12 years after vaccination. In conclusion, however, it is not yet possible to say whether the vaccination protection should not be refreshed at some point.
You can read more about the implementation, effectiveness and costs of this vaccination against HPV in the article HPV vaccination.
Support groups
Cancer information service: Cancer self-help groups and patient associations
Tags: Diagnosis hair gpp










.jpg)