Neuroborreliosis
and Martina Feichter, medical editor and biologistFabian Dupont is a freelance writer in the medical department. The human medicine specialist is already doing scientific work in Belgium, Spain, Rwanda, the USA, Great Britain, South Africa, New Zealand and Switzerland, among others. The focus of his doctoral thesis was tropical neurology, but his special interest is international public health and the comprehensible communication of medical facts.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Neuroborreliosis is a form of Lyme borreliosis. It develops when the Borrelia bacteria spread in the body and attack the brain or nerve tracts. The resulting symptoms are varied. This can make diagnosis difficult. Here you can find out more about the symptoms, diagnosis and treatment of neuroborreliosis.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. M01G01A68
Neuroborreliosis: symptoms and course
Doctors differentiate between early and late (chronic) neuroborreliosis. With early neuroborreliosis the symptoms last weeks to months, with later neuroborreliosis months to years.
Early neuroborreliosis: symptoms
Early neuroborreliosis is present in probably more than 98 percent of all neuroborreliosis patients. The first symptoms appear within a few weeks to a few months after infection with the borreliosis pathogen (via a tick bite).
Typically, painful, non-purulent inflammation of the meninges and nerve roots of the spinal cord develops. Doctors speak of meningopolyradiculitis here. It manifests itself with excruciating nerve pain.Those affected describe the pain as burning, piercing, biting or tearing and suffer from it especially at night.
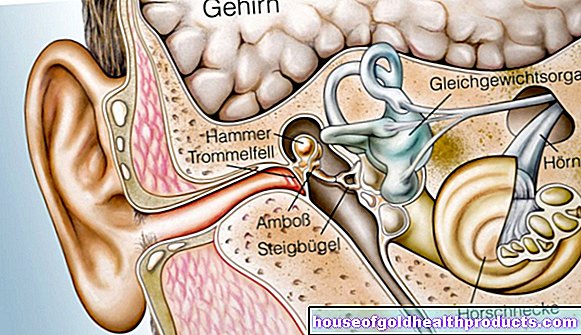
Paralysis and flaccid paralysis can also occur. For example, early neuroborreliosis is often associated with unilateral or bilateral facial paralysis (facial paralysis). It is based on inflammation of the 7th cranial nerve (facial or facial nerve). More rarely, other cranial nerves are inflamed in neuroborreliosis. The possible consequences include paralysis of the eye muscles, hearing loss and dizziness.
In children with early neuroborreliosis, one often only sees isolated facial paralysis or acute meningitis (meningitis). The latter can be accompanied by symptoms such as headache, stiff neck, photophobia, nausea, vomiting, and emotional lability.
Late neuroborreliosis: symptoms
Late (chronic) neuroborreliosis is rare. In those affected, the neurological symptoms develop insidiously over months or years, typically leading to a chronic, progressive inflammation of the brain and spinal cord (encephalomyelitis).
Those affected usually have no pain, but suffer from gait disorders and problems with emptying the bladder. In addition, late neuroborreliosis can cause symptoms such as speech and language problems, hearing loss, coordination difficulties, sensory disorders and symptoms of paralysis.
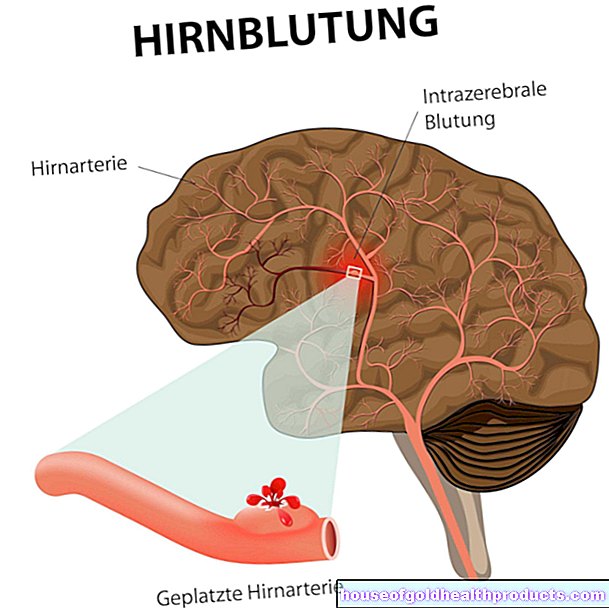
Epilepsy or an organic psychosyndrome (with impaired concentration and consciousness as well as hallucinations) rarely develop in later neuroborreliosis. Blood vessels in the brain also rarely become inflamed (cerebral vasculitis), which can lead to a stroke. Isolated meningitis (meningitis) occurs very rarely.
Post Lyme Disease Syndrome
Experts differentiate a disease state from confirmed late neuroborreliosis, which can be differentiated using different terms such as "Post-Lyme-Disease-Syndrome" or "Post-Treatment Lyme-Disease-Syndrome" (PTLDS), sometimes also "(Post-) Lyme-Encephalopathy" or unspecific "Chronic Lyme Disease" is called.
Nonspecific chronic complaints such as persistent fatigue, lack of drive and poor concentration are associated with an earlier Lyme disease infection - without an inflammatory-infectious process being able to be proven in laboratory diagnostics according to generally accepted criteria.
Therefore, one should first think of other clinical pictures such as another chronic infection, an autoimmune disease or depression.
Antibiotic therapy does not make sense in post-borreliosis syndrome.
Neuroborreliosis: examination and diagnosis
If a patient has any of the above symptoms and reports a previous tick bite, the doctor suspects neuroborreliosis. This also applies if a patient does not remember a tick bite, but the possibility of one existed or exists (through walks in the forest, gardening, etc.).
Laboratory tests
The doctor can carry out various laboratory tests to clarify the suspicion.
Detection of Borrelia antibodies
This test can examine the patient's blood and cerebrospinal fluid (nerve fluid or CSF) for specific antibodies against Borrelia bacteria. However, the results of such tests cannot always be clearly interpreted. One of the reasons for this is that Borrelia antibodies can still be detected even if the infection was a long time ago and has long since healed.
Detection of inflammatory CSF changes
If Borrelia antibodies are actually found in the nerve fluid sample (liquor sample), this is not enough for a reliable diagnosis. It must also be possible to detect inflammatory changes in the nerve water. These include an increased number of white blood cells and an increase in total protein.
Direct pathogen detection
To support the diagnosis of neuroborreliosis, the pathogen can also be detected directly in the nerve water (in specially trained laboratories). To do this, a CSF sample is taken from the patient and an attempt is made to use it to grow Borrelia bacteria (culture) or to detect fragments of the pathogen's genetic material (using polymerase chain reaction = PCR).
However, this only works in relatively few cases. In addition, a Borrelia culture is very time-consuming. In addition, only special laboratories can reliably carry out these tests.
Therefore, the direct detection of borreliosis pathogens in suspected neuroborreliosis is usually only recommended in exceptional cases. It can be helpful, for example, if a patient can hardly produce antibodies due to an immunodeficiency, so that antibody tests are not very meaningful.
CXCL13 measurement
For some years now, the neuroborreliosis diagnosis has been supported in individual cases by measuring the CXCL13 level in the nerve water. The CXCL13 is one of the so-called chemokines. These are small proteins that are released in response to an infection or injury and are involved in controlling individual defense cells of the immune system.
In almost all patients with acute neuroborreliosis, the CXCL13 level in the nerve water increases significantly - even before the body has formed specific antibodies against the borreliosis pathogen. And it usually falls with the start of antibiotic treatment.
However, the CXCL13 level also increases in other diseases. In addition, there is still no standardized procedure for determining this protein in CSF. Therefore, the CXCL13 measurement in the nerve water is only recommended if someone shows symptoms of early neuroborreliosis, but the number of white blood cells is (still) normal and / or no Borrelia antibodies can (yet) be detected.
Further investigations
Common blood parameters are also routinely determined if neuroborreliosis is suspected. These include the erythrocyte sedimentation rate (ESR), white blood cells (leukocytes) and C-reactive protein (CRP). These values are normal or slightly increased in neuroborreliosis and can generally indicate a (systemic) infection that affects the whole body. The main purpose of determining such blood parameters is to exclude other causes for the possible signs of neuroborreliosis.
In certain cases, the doctor will carry out additional tests. If he suspects that the Borrelia have caused an inflammation of the brain vessels (cerebral vasculitis), he will arrange for a magnetic resonance imaging (MRI, magnetic resonance imaging) to be carried out.
Neuroborreliosis: Therapy
Neuroborreliosis (like normal borreliosis) is treated with antibiotics. The following antibiotics are available:
- Doxycycline (as a tablet)
- Ceftriaxone (as an infusion)
- Cefotaxime (as an infusion)
- Penicillin G (as an infusion)
Which antibiotic the doctor chooses for neuroborreliosis therapy in each individual case depends on individual patient aspects. Among other things, how old the patient is, whether they are known to be allergic to one of the antibiotics, or whether they are pregnant, all play a role. For example, pregnant women and children under nine years of age should not be treated with doxycycline.
The duration of antibiotic therapy depends on whether you have early or late neuroborreliosis: In the case of early neuroborreliosis, the antibiotics are usually given for 14 days, in later neuroborreliosis usually for 14 to 21 days.
Experts advise against even longer antibiotic therapy for two reasons: On the one hand, there is no evidence that longer antibiotic therapy is more effective than the recommended two-week (early neuroborreliosis) or two to three-week (late neuroborreliosis) therapy. On the other hand, long-term antibiotic therapy can have serious side effects.
In patients who still have debilitating symptoms six months after antibiotic therapy, doctors re-examine a sample of the cerebrospinal fluid. If the white blood cell count is still high and there is no other explanation than neuroborreliosis, repeat antibiotic therapy.
Tags: desire to have children eyes prevention