Hepatitis B.
and Carola Felchner, science journalistDr. med. Mira Seidel is a freelance writer for the medical team.
More about the expertsCarola Felchner is a freelance writer in the medical department and a certified training and nutrition advisor. She worked for various specialist magazines and online portals before becoming a freelance journalist in 2015. Before starting her internship, she studied translation and interpreting in Kempten and Munich.
More about the experts All content is checked by medical journalists.Hepatitis B (also: liver inflammation type B) is a viral infection of the liver. It is usually transmitted through sexual contacts. The disease can be both acute and chronic. Symptoms include fatigue, jaundice, or discoloration of urine and stool. Sometimes infected people show no symptoms at all. Read more about ways of infection, symptoms, therapy, prognosis and prevention of hepatitis B here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. B18B16

What is hepatitis B?
Hepatitis B is one of the most common liver infections caused by viruses (viral hepatitis) worldwide. Most patients become infected with the pathogen during sexual intercourse. The infection can be acute or chronic. According to the World Health Organization WHO, around 240 million people are chronically infected with hepatitis B worldwide.
In endemic areas such as sub-Saharan Africa and the East Asian region, the infection rate is five to ten percent of the population. In Germany, however, hepatitis B is comparatively rare, with a proportion of less than one percent. Nevertheless: 55 percent of the hepatitis cases reported in this country are type B infections. Around 780,000 people worldwide die each year from the disease and its consequences (cirrhosis of the liver, liver cancer).
Hepatitis B is notifiable. This means: The attending physician must report the names of patients who are suspected of having hepatitis B or who have been proven to have such an infection to the responsible health authority. Deaths from hepatitis B must also be reported by name to the health department. The office forwards the data to the Robert Koch Institute, where they are recorded statistically.
Hepatitis B: symptoms
Hepatitis B is usually not that easy to recognize for those affected. Many signs of infection are non-specific (such as tiredness, nausea). Often there are no symptoms at all (asymptomatic infection). This is particularly tricky because the highly contagious hepatitis B virus can then unwittingly be transmitted to many healthy people.
Note: About a third of all infected adults show no symptoms. Another third have symptoms such as tiredness, poor appetite, nausea, and muscle and joint pain, but no jaundice. In the last third, jaundice is also present (along with the other complaints).
Hepatitis B incubation period
The time between infection and the appearance of the first symptoms in hepatitis B (incubation period) is 30 to 180 days. On average, it takes 60 to 120 days (two to four months) for the disease to break out.
Acute hepatitis B: symptoms
Acute hepatitis B begins with unspecific symptoms such as loss of appetite, aversion to certain foods, nausea and vomiting, muscle and joint pain and a slight fever.
After about three to ten days, jaundice (jaundice) can - but does not have to - occur: the skin, mucous membranes and the whites of the eyes (sclera) turn yellow. This is often seen in young children and people with weak immune systems. Furthermore, the stool can discolour and the urine can become dark.
Chronic hepatitis B: symptoms
Hepatitis B is called chronic if specific antibodies against the pathogen can be detected in the blood for more than six months. Symptoms do not necessarily occur in those affected. If so, then they show up, among other things, in the form of:
- fatigue
- Joint and muscle pain
- Loss of appetite
- Weight loss
- occasional sensations of pressure under the right costal arch
In about one percent of patients, the chronic inflammation develops into liver cancer or shrunken liver (cirrhosis of the liver). The risk of liver cancer in hepatitis B patients is around 100 times higher than in the "normal population"! The development of cirrhosis of the liver is favored by alcohol abuse and an additional hepatitis C infection.
Additional infection with hepatitis D.
Hepatitis B patients can also become infected with hepatitis D. With this so-called superinfection, the liver disease is more severe than with hepatitis B infection alone. In addition, the additional infection with virus type D increases the risk of liver cirrhosis even further. Liver cancer is also favored: in a combined infection with hepatitis B and D, the malignant tumor forms earlier than in a B infection alone.
Note: A hepatitis D infection is only possible in the presence of hepatitis B viruses.
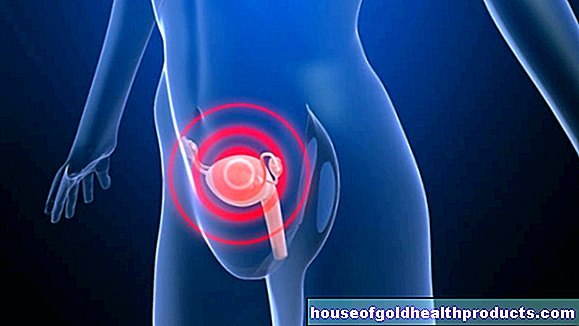
Hepatitis B: transmission
Hepatitis B viruses are very often passed on through sexual contact - via semen, vaginal secretions or saliva. But other body fluids such as breast milk, tears or blood can also transmit the pathogens. The disease is often passed on via infected blood. Therefore, people who handle blood and needles or other sharp objects are particularly at risk of hepatitis B infection. This includes:
- medical staff
- Dialysis patients
- drug addicts
- Patients who receive blood products or blood plasma (today blood products are strictly controlled before they are administered)
- People who have their ears pierced, tattoos or pierced under unsanitary conditions
Attention: Infection is also possible via shared toothbrushes and from mother to child (during pregnancy or childbirth and when breastfeeding). If a mother is known to be infected with hepatitis B, the child will therefore be vaccinated within 12 hours of birth.
Hepatitis B: examinations and diagnosis
To diagnose hepatitis B, the doctor takes blood from the patient. The laboratory examines whether it contains direct and / or indirect evidence of hepatitis B viruses:
- Virus DNA: The genetic makeup of the hepatitis B virus (HBV DNA) is an important indicator of type B liver inflammation.
- Virus antigens: These are specific components of the protein envelope of viruses (HBs-Ag, HBc-Ag and HBe-Ag). They allow (like virus DNA) a direct pathogen detection.
- Specific antibodies: In the case of hepatitis B infection, the immune system produces specific antibodies against the pathogen (such as anti-HBc). Their presence is indirect evidence of the pathogen.
The doctor can draw valuable conclusions from the presence or absence of antigens and antibodies. Some examples:
A current hepatitis B infection is present if the genetic makeup of the virus, the virus antigen HBs-Ag and the antibody type anti-HBc can be detected in the patient's blood. The antibody type anti-HBs is missing in this case.
When hepatitis B has healed, antibodies of the anti-HBc type (and usually anti-HBs as well) circulate in the blood. In contrast, the virus antigen HBs-Ag cannot be detected.
If only antibodies of the anti-HBs type are found in the blood, but no other antibodies and also no antigens from hepatitis B viruses, this indicates that the person concerned has an effective vaccination against hepatitis B.
Further investigations
Other parameters are determined in the patient's blood sample. Elevated liver values (such as GPT, GOT, Gamma-GT) can indicate liver damage.
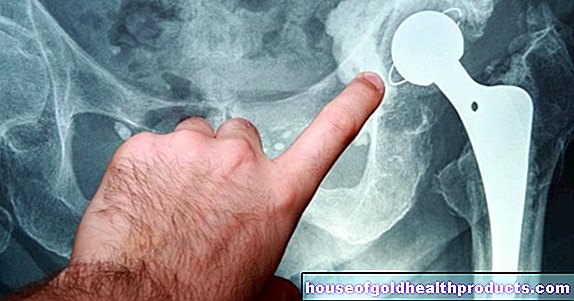
The doctor can use an ultrasound scan to assess the structure and size of the liver. In the case of chronic hepatitis B, tissue samples can also be taken from the liver (liver biopsy) to determine the extent of the tissue damage.
Hepatitis B: treatment
In the case of an acute infection, no specific hepatitis B therapy is usually necessary - the disease almost always heals spontaneously on its own. However, if necessary, the doctor can treat the symptoms.
In addition, patients should keep bed rest, take physical care, and eat high-carbohydrate but low-fat foods. It is also very important not to use alcohol - detoxifying it would put additional strain on the sick liver. For the same reason, liver-damaging drugs such as pain relievers and female sex hormones (pill) should not be taken if possible.
Chronic hepatitis B is usually treated with antiviral drugs. These include:
- Nucleoside and nucleotide analogs: They inhibit the multiplication of the hepatitis viruses. For example, lamivudine, entecavir, telbivudine or tenovovir dipivoxil are used. The active ingredients are taken as tablets.
- Interferon-α and pegylated interferon α (PEG-interferon α): They also have an antiviral effect and also stimulate the immune system. It is used as a syringe.
The goal of drug therapy is to lower the amount of virus in the blood as much as possible. This reduces the risk of cirrhosis of the liver and liver cancer as a result of chronic hepatitis B. However, the disease is usually not curable with medication.
Note: In some patients with chronic hepatitis B, the viruses reproduce only slightly, the liver values are often normal and the liver is (still) little damaged. Therapy is then often limited to regular check-ups.
If the chronic inflammation of the liver has led to severe liver cirrhosis, the last treatment option is a liver transplant.
Hepatitis B: course and prognosis
In about nine out of ten adults with acute hepatitis B, the inflammation of the liver heals spontaneously and without consequences within a few weeks. It is only rarely very violent and difficult (fulminant course).
In up to ten percent of adult patients, the acute infection develops into chronic hepatitis. People with a weakened immune system are particularly susceptible to this: With them, a hepatitis B infection becomes chronic in 30 to 90 percent of cases.
In children, hepatitis B almost always takes a chronic course (around 90 percent).
Possible consequences of chronic hepatitis B are liver cirrhosis and liver cancer.
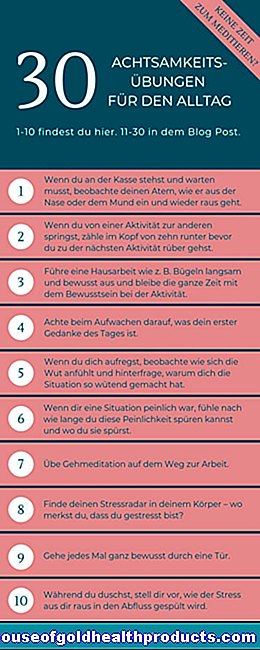
Hepatitis B: Prevention
The most effective way to avoid getting hepatitis in the first place is to get a hepatitis vaccination. The active hepatitis B vaccination stimulates the immune system to produce specific antibodies against the pathogen. It is available as a single vaccine or as part of combination vaccines (e.g. together with the hepatitis A vaccine). Depending on the vaccine and vaccination schedule, three or four vaccine doses are necessary for long-term protection (basic immunization). Talk to your doctor about what makes sense in your case and ask him and your health insurance company whether the costs of the vaccination will be covered.
Note: Antibody formation takes some time. The doctor can then check whether the vaccination was successful by doing a blood test one to two months after the vaccination. This is particularly important for medical staff, for example.
In contrast to the active vaccination, the passive hepatitis B vaccination offers immediate protection against the pathogen. This is because finished antibodies against hepatitis B are administered. This can be necessary, for example, when healthy people have come into contact with infected blood of a patient (e.g. in the case of needlestick injuries). The immediately effective passive vaccine then bridges the time until the concurrent active vaccine develops its protective effect.
Newborns from hepatitis B infected mothers also receive an active and a passive vaccine against hepatitis B viruses within 12 hours of birth.
Note: Passive vaccination does not last long. The administered (foreign) antibodies are broken down by the organism over time.
Further protective measures
To prevent hepatitis B, you should always use a condom during sexual intercourse. This is especially true if the sexual partner changes frequently.
In addition, healthy people and those infected with hepatitis B should not share toothbrushes, nail scissors or razors.
Tags: anatomy teeth prevention