Cerebral hemorrhage
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Cerebral hemorrhage occurs when a blood vessel in the skull bursts. The result can be a stroke, also known as a hemorrhagic cerebral infarction. Depending on the location of the cerebral hemorrhage, doctors differentiate between intracerebral hemorrhage, subarachnoid hemorrhage and epidural hemorrhage. Read more about the topic here: How can a cerebral hemorrhage be recognized? What can it trigger? How is cerebral haemorrhage diagnosed and treated? What is the prognosis?
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. I61I62S06I60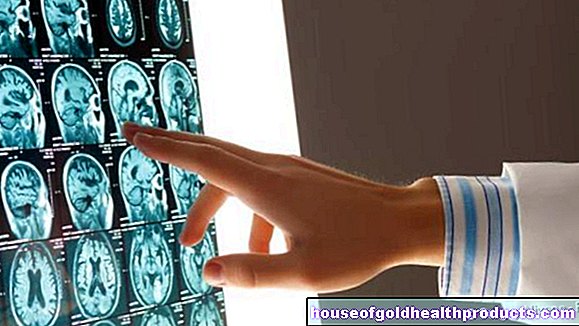
Brief overview
- Cerebral haemorrhage - Definition: Bleeding in the skull as a result of a ruptured blood vessel. Can cause a stroke (hemorrhagic infarction).
- Forms: intracerebral hemorrhage (ICB), subarachnoid hemorrhage (SAB), epidural hemorrhage, subdural hemorrhage
- Causes & risk factors: e.g. high blood pressure and arteriosclerosis, smoking, obesity, unhealthy diet, congenital vascular malformations, bleeding disorders, head injuries, etc.
- Symptoms: Depending on the location and severity, including acute severe headaches, nausea, vomiting, impaired consciousness, neurological deficits such as paralysis, speech, language and visual disorders, dizziness, seizures.
- Diagnosis: mainly neurological examination, computed tomography (CT), magnetic resonance imaging (MRT), angiography
- Treatment: Depending on the type and severity with bed rest, stabilization of the vital functions (such as breathing), medication (e.g. against pain, cramps, brain swelling), catheter to drain off congested cerebral fluid, surgical clearing out of the accumulation of blood.
- Course & prognosis: A cerebral haemorrhage is a medical emergency with high mortality in some cases! Therefore, early treatment is extremely important.
Cerebral haemorrhage: definition
Cerebral haemorrhage is the colloquial term for bleeding within the skull (intracranial bleeding), triggered by a ruptured blood vessel. A stroke can result from such bleeding, namely when the accumulation of blood leads to functional disorders in a brain area with partial death of brain cells. Doctors speak of a hemorrhagic stroke or hemorrhagic cerebral infarction.
The vast majority of all strokes are not caused by a cerebral hemorrhage, but by an acute hypoperfusion of a brain area (ischemic stroke). This is usually caused by the fact that a blood clot or vascular calcification (arteriosclerosis) severely constricts or closes a brain vessel.
Strictly speaking, cerebral hemorrhage is an umbrella term that encompasses various clinical pictures. Depending on where the hemorrhage takes place, doctors differentiate between the following types of cerebral hemorrhage:
- intracerebral haemorrhage (intracerebral hematoma)
- subarachnoid hemorrhage (subarachnoid hemorrhage)
- epidural bleeding (epidural bleeding, epidural hematoma)
- subdural hemorrhage (subdural hemorrhage, subdural hematoma)
Hemorrhagic stroke results from either intracerebral or subarachnoid cerebral haemorrhage
Intracerebral haemorrhage (intracerebral hematoma)
An intracerebral hemorrhage (ICB) is a bleeding into the brain tissue (brain parenchyma). Usually it is due to high blood pressure, especially in combination with hardening of the arteries (arteriosclerosis), when a brain vessel bursts and causes parenchymal bleeding. Because an intracerebral hemorrhage usually affects a relatively large area of the brain, medical professionals also speak of brain mass hemorrhage. The term "intracerebral hematoma" (= bruise in the brain tissue) is often used.
The hematoma can form in different areas of the brain:
- in the basal ganglia
- in the lobes of the brain (this is called lobar bleeding)
- in the brain stem
- in the cerebellum
- in the cavity system of the brain (ventricular system)
The intracerebral hemorrhage accounts for around 10 to 15 percent of all strokes.
Subarachnoid hemorrhage
The subarachnoid hemorrhage (SAB) arises below ("sub") the Arachnoid (middle meninges) - i.e. between this and the soft (innermost) meninges that lie directly on the brain tissue. The result can be a stroke. About five percent of all strokes can be traced back to SAB.
Read everything you need to know about this form of cerebral hemorrhage in the article Subarachnoid Hemorrhage!
Epidural bleeding (epidural bleeding, epidural hematoma)
With epidural bleeding, blood collects above ("epi") the Dura mater (hard meninges). It is the outermost of the three meninges and lies below the skull bone. An epidural haemorrhage is a bleeding between the skull bones and the hard meninges. This form of cerebral hemorrhage is usually the result of an external force (i.e. trauma-related), for example in the event of an accident. It usually occurs in connection with a skull fracture (skull fracture).
Subdural bleeding (subdural bleeding, subdural hematoma)
With a subdural hemorrhage, blood collects underneath ("sub") the Dura mater - i.e. between the outer (hard) meninges and the middle meninges (cobweb skin, Arachnoid). Here, too, the cause is usually an external force (trauma) that ruptures blood vessels. Depending on how quickly a subdural hematoma becomes noticeable with symptoms, it is referred to as acute, subacute or chronic:
- acute: symptoms develop within minutes or a few hours.
- subacute: symptoms develop over several hours or days.
- chronic: symptoms develop slowly over weeks, months, or even years.
The three meninges continue as spinal cord membranes in the spinal canal, where they enclose the spinal cord. Bleeding above or below the Dura mater - i.e. epidural or subdural bleeding - can therefore also occur in the spinal cord. Such bleeding is called "spinal". They are much less common than epidural or subdural bleeding in the skull.
Cerebral haemorrhage: symptoms
The symptoms of a cerebral haemorrhage arise either from the fact that the leaked blood directly irritates the sensitive meninges or presses on neighboring brain regions, or because some of the brain cells no longer receive blood due to the bursting of the vessel and consequently dies. The specific symptoms that occur depend largely on the type, location and extent of the cerebral haemorrhage and the extent to which brain cells are affected. Cerebral haemorrhage can trigger very different types of signs, which are also usually very similar to those of a "classic" stroke (stroke caused by acute hypoperfusion). For example:
- Sudden, very severe headache
- Neck stiffness (meningism), especially with subarachnoid hemorrhage
- Nausea, vomiting
- Sudden weakness (hemiparesis) or paralysis (hemiplegia) limited to one side of the body, especially of an arm, leg or face
- Numbness (hypoesthesia)
- Speech disorders (aphasia), speech disorders (dysarthria)
- Difficulty swallowing (dysphagia)
- Visual disturbances: double vision (diplopia), blurred vision, temporary loss of vision in one eye, loss of field of vision on one side
- Dilation of the pupil (mydriasis)
- Dizziness with unsteady gait, balance or coordination problems
- sudden disturbance of consciousness: confusion, drowsiness up to and including loss of consciousness and coma
- Seizures
How noticeable the signs are in a cerebral hemorrhage can vary widely. For example, intracerebral haemorrhage very often causes sudden severe headache, impaired consciousness, nausea and vomiting. However, if the bleeding into the brain tissue is only very small, consciousness can remain unaffected. Headaches and nausea can also be minimally absent.
Typically, the signs of a cerebral haemorrhage appear suddenly, i.e. within a short time - unless there is a chronic subdural hematoma: Here, as mentioned above, the symptoms develop very gradually over the course of weeks to years.As soon as they are finally noticed, the subdural hematoma is usually quite extensive.
Cerebral haemorrhage: diagnosis
A quick diagnosis and a quick start of therapy are very important with a cerebral haemorrhage. Therefore you should call the emergency doctor immediately if someone shows symptoms like the above!
Conversation and neurological examination
A neurological examination is part of the diagnosis of a cerebral haemorrhage or a stroke (regardless of whether it is caused by cerebral haemorrhage or insufficient blood flow). The doctor checks the patient's level of consciousness and the function of various nerves. It is also important for the doctor to know how the signs of the (possible) cerebral hemorrhage have developed, as well as information on accompanying circumstances (such as a fall, taking medication, drug consumption, etc.). However, since people with a fresh cerebral hemorrhage are often unable to concentrate and cannot give precise information, an accompanying person should be on site if possible and describe the course of events to the doctor as best he can.
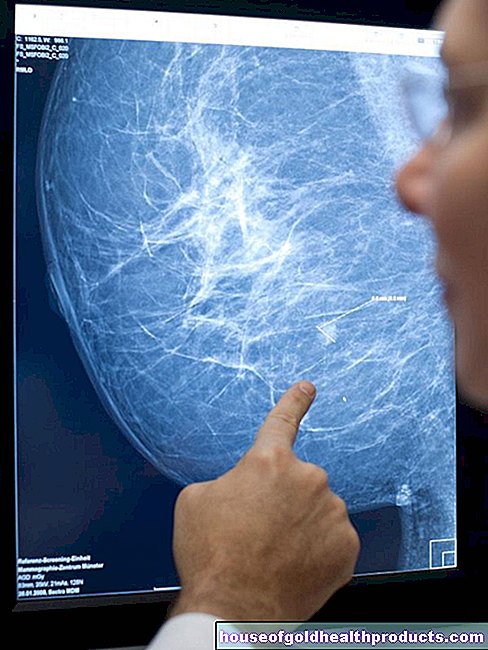
CT or MRI
The most important imaging method for cerebral hemorrhage is computed tomography of the head (cerebral computed tomography, cCT). With their help, a cerebral haemorrhage can be detected immediately after it occurs: The doctor recognizes the leaked blood on the detailed images as a "light spot" and can thus determine the exact location and extent of the cerebral haemorrhage. In addition, a stroke caused by cerebral haemorrhage (hemorrhagic stroke) can be distinguished from a stroke due to vascular occlusion (ischemic stroke) - both cause very similar symptoms (see above).
An alternative to cCT is magnetic resonance imaging (magnetic resonance imaging) of the head (cerebral MRI, cMRT). As with CT, the images show a patch-like change in the brain if there is a cerebral hemorrhage.
Vascular x-ray
Vascular x-ray (angiography) in the area of the skull, i.e. an x-ray of the cerebral vessels using a contrast medium, is also informative in the case of cerebral hemorrhage. Even clearer images are created when angiography is combined with computed tomography or magnetic resonance tomography. Doctors then speak of CT angiography or MR angiography:
Both methods provide significantly more detailed images than a simple vascular X-ray. In this way, the doctor can see more precisely which cerebral vessel has burst where, where the bleeding is extensive and also whether the bleeding is still going on (recognizable by the leaked X-ray contrast agent). Any vascular malformations such as congenital sac-like protuberances (aneurysms) are also clearly recognizable. They tear easily and are therefore a possible cause of a cerebral haemorrhage.
Further investigations
Further examinations may be useful as required. Measuring the blood flow (perfusion) in the brain sometimes provides important information when diagnosing a stroke. Like angiography, it can be combined with computer or magnetic resonance tomography, which is then referred to as CT perfusion or MRT perfusion.
If the doctor suspects subarachnoid hemorrhage in the patient, but the CT or MRI images of the brain are inconclusive or inconspicuous, he usually takes a sample of the cerebral spinal cord fluid (liquor) from the patient in the lumbar spine (lumbar puncture). It will be examined in the laboratory. If blood can be detected in the CSF, this speaks in favor of SAB.
Further examinations can also help to track down the cause of a cerebral hemorrhage. For example, blood tests can be used to detect an increased tendency to bleeding, which has led to cerebral haemorrhage. This bleeding tendency can be caused by the blood disease (haemophilia), the use of blood-thinning medication or an advanced liver disease (cirrhosis of the liver).
Cerebral haemorrhage: course & prognosis
The course and prognosis of a cerebral haemorrhage depend on various factors. These include, for example, the location and extent of the bleeding, any accompanying injuries and underlying diseases of the patient, as well as their age. Treatment as early as possible is also extremely important: the earlier the intracranial hemorrhage is detected and properly treated in the hospital, the better the prognosis. This is especially true in the case of extensive cerebral hemorrhage - the chances of survival can then decrease rapidly within a short period of time!
Intracerebral haemorrhage is usually extensive and associated with high mortality. Up to 50 percent of patients die within the first three months and up to 60 percent within a year. If you survive such a cerebral hemorrhage, permanent consequences are not uncommon. In fact, even most survivors do not regain all brain functions.
Subarachnoid hemorrhage is also very dangerous. In most patients, intracranial bleeding is caused by a rupture (rupture) of an aneurysm in the brain. Around 35 percent of those affected die as a result of the first rupture, and another 15 percent within a few weeks as a result of another rupture. In survivors, this form of cerebral hemorrhage can also have long-term consequences - even with optimal treatment. Read more about it here.
An acute subdural hematoma is often associated with other severe brain injuries. That explains the high mortality rate of 30 to 50 percent. With the chronic variant of this cerebral hemorrhage, the chances of recovery are better. People usually get better or at least stop getting worse after a while. If the chronic accumulation of blood under the meninges has been surgically removed, there is a high risk of relapse (10 to 30 percent).
The prognosis for epidural bleeding is better than for acute subdural bleeding. The mortality is about 20 percent. If the affected brain area is relieved of pressure from the overlying bruise at an early stage and there are only minor neurological deficits (such as impaired consciousness, hemiplegia), the prognosis is good.
Cerebral haemorrhage: treatment
The treatment of a cerebral hemorrhage depends primarily on the size, location and cause of the hemorrhage. As a rule, patients need to be hospitalized as quickly as possible, usually in the intensive care unit. But they can be continuously monitored and stabilized as needed, for example with regard to blood clotting, blood pressure and / or breathing. The latter sometimes requires artificial respiration.
Conservative treatment of symptoms and complications
The symptoms of a cerebral hemorrhage, as well as any complications, are treated as needed. For example, severe headaches can be brought under control with painkillers, high fever with fever reducers and seizures with anticonvulsants. Vascular spasms (vasospasms), such as those that can develop with subarachoid hemorrhage, can also be treated with medication.
Preventing or treating swelling of the brain (cerebral edema), which can result from major cerebral hemorrhage, is also particularly important. The swelling can cause a dangerous increase in pressure in the skull - with the risk that the highly sensitive brain cells will be compressed and die. In order to prevent or treat brain swelling or increased intracranial pressure, conservative measures are sometimes sufficient. These include the administration of medication and the elevation of the upper body. In other cases, surgery is necessary.
Surgical interventions
Depending on the location and extent, a cerebral hemorrhage often has to be treated surgically. Surgery may also be necessary to stop the source of bleeding (e.g. in the case of a ruptured aneurysm) and / or to drain off any cerebral fluid. More on this below:
Intracerebral haemorrhage
The surgical removal of an intracerebral hematoma is considered very carefully. There is a risk that the surgery itself will damage brain tissue, which can result in severe disability or even death of the patient. In certain cases, the surgical treatment of the cerebral hemorrhage can also be life-saving, for example in the case of a major hemorrhage in the cerebellum.
Sometimes the circulation of the nerve fluid (liquor) in the cavity system of the brain (ventricular system) is disturbed as a result of intracerebral hemorrhage. Then nerve water can build up, which increases the pressure in the brain and causes a "water head" (hydrocephalus). To prevent this, the doctor can place a catheter (shunt) through which excess nerve water can drain from the ventricular system.
Subarachnoid hemorrhage
If - as is usually the case - a torn vascular sac is the origin of the subarachnoid hemorrhage, a surgeon will in some cases clamp the aneurysm ("clipping"). More often, however, one chooses the so-called "coiling" as a treatment method. As part of an angiography, a small platinum coil is advanced over the inguinal artery to the brain aneurysm. It fills the vascular sac and stops the bleeding.
As with an intracerebral hemorrhage, the following also applies here: Sometimes a shunt has to be placed in order to drain pent-up nerve water from the brain (for example into the abdominal cavity) so that a "water head" with an increase in intracranial pressure can be prevented or eliminated.
Read more about the treatment of subarachnoid hemorrhage here.
Subdural hematoma
A small subdural hematoma in adults often does not require treatment - the blood that leaks between the outer and middle meninges is absorbed by the tissue on its own.
Larger subdural hematomas, on the other hand, are surgically removed in order to reduce the increased pressure on the brain caused by the accumulation of blood. Sometimes one or more small drill holes in the top of the skull are sufficient for this, through which the leaked blood is drained. In other cases, a larger opening of the skull is necessary to clear a subdural hematoma. In the course of the procedure, the surgeon usually places a drainage tube for a few days, through which any blood that has leaked can drain away - the subdural bleeding can occur again.
In young children, a subdural hematoma is almost always operated on - if only for visual reasons. The skull bones of small children are still soft and pliable. Therefore, the cerebral hemorrhage leads less to an increase in intracranial pressure than to an increase in the circumference of the head (similar to a "water head" = hydrocephalus).
Epidural hematoma
Any accumulation of blood between the skull and the outer meninges is immediately removed surgically. This has to be done as quickly as possible, especially with larger epidural hematomas, in order to reduce the pressure on the brain area below. To do this, the surgeon usually drills one or more holes in the top of the skull so that the blood that has leaked can drain off. It may also be necessary to temporarily remove part of the skull to clear out the epidural hematoma. The surgeon also looks for the source of the bleeding and stops it.
Cerebral haemorrhage: rehabilitation
After the acute treatment of a cerebral haemorrhage, rehabilitation often follows - especially if the cerebral haemorrhage has caused a stroke (hemorrhagic stroke). The aim of rehab is to eliminate or at least reduce mental and / or physical consequential damage. This is intended to prepare the patient for life after a cerebral haemorrhage with possible long-term consequences.
Rehabilitation - individually adapted teamwork
The rehabilitation is individually adapted to the needs of the patient. It usually takes place in a specialist clinic. There the patient is cared for by a rehabilitation team made up of various specialists such as doctors, physiotherapists, speech and occupational therapists. The relatives can also support the patient in many situations. The earlier rehabilitation begins after a stroke caused by cerebral haemorrhage (or vascular occlusion), the better the chances of success. Whether long-term rehabilitation is necessary depends on the extent of the nerve damage suffered as a result of the cerebral haemorrhage.
An intracranial hemorrhage can result in movement disorders. With suitable training methods such as Bobath or Vojta, the therapists try to reverse such physical functional restrictions as much as possible during rehabilitation.
Attempts are also made to improve disorders of language (aphasia), speech (dysarthria), vision, memory and attention. In addition, the stroke patient's independence is promoted in rehab. Some sufferers have to learn again to wash, dress or cook by themselves.
Some patients recover completely relatively quickly after the cerebral hemorrhage, while others take months to years before they can regain control of their everyday activities. Often, however, the physical functions that were impaired by the cerebral haemorrhage cannot be improved again despite intensive rehabilitation. Then it is a matter of developing strategies together with the patient so that he can cope better with the restrictions. In the case of swallowing disorders (dysphagia), for example, special body and head postures are practiced to prevent swallowing.
Read more about rehab after a stroke caused by cerebral hemorrhage or reduced blood flow here.
Cerebral haemorrhage: causes and risk factors
Intracerebral haemorrhage
In most cases, intracerebral haemorrhage is caused by chronic high blood pressure. This promotes vascular calcification (arteriosclerosis), also in the small arteries in the brain. The wall of the vessels is weakened as a result, which means that the increased blood pressure can easily burst them - resulting in intracerebral hemorrhage.
Various factors can promote arteriosclerosis and high blood pressure and thus also contribute to intracerebral bleeding in the manner described. These include:
- smoking
- Obesity
- unhealthy diet high in calories, saturated fat, and trans fats
In some patients, cocaine or amphetamine use has temporarily raised blood pressure so high that intracerebral bleeding has occurred.
Rarer causes of this type of cerebral hemorrhage include:
- Vascular malformations (such as aneurysms)
- Head injury
- Brain tumors
- Inflammation of the blood vessels (vasculitis)
- Bleeding disorders
- high-dose use of anticoagulants (anticoagulants)
Subarachnoid hemorrhage
In most cases, this form of cerebral hemorrhage is the result of a head injury, i.e. it is traumatic. A distinction must be made between spontaneous subarachnoid hemorrhages. They are usually caused by the rupture of an aneurysm. More rarely, there are other causes behind it, such as other vascular malformations, inflammation of the arteries (arteritis), bleeding disorders or cocaine use.
Only spontaneous, non-traumatic subarachnoid hemorrhage is considered a hemorrhagic stroke.
Epidural hematoma
An epidural hematoma in the head usually results from a head injury, more precisely a traumatic brain injury (TBI). For example, this type of cerebral haemorrhage can occur after a fall while doing sports without a protective helmet (e.g. while skiing).
Spontaneous epidural bleeding due to a specific vascular malformation in the brain (AV dural fistula) is less common.
Subdural hematoma
Acute and subacute subdural hemorrhages usually occur as part of a severe traumatic brain injury suffered by the person, for example, from a fall or a car accident. Sometimes they also form in people with a bruised brain or an epidural hematoma.
Chronic subdural hematoma is often seen in alcoholics and the elderly - both groups tend to fall and often ignore or forget about minor or moderately severe head injuries. If these injuries result in subdural bleeding, it can become chronic.
The chronic variant of this form of cerebral hemorrhage is also often found in people who take anticoagulants.
Cerebral haemorrhage: prevention
Certain factors that can lead to cerebral haemorrhage cannot be prevented - for example congenital vascular malformations (such as aneurysm). But there are many other things you can do:
In order to prevent intracerebral hemorrhage and the resulting stroke, you should first and foremost have an existing high blood pressure treated appropriately - and contribute to it yourself: Measure your blood pressure regularly and take the prescribed medication consistently - even if you are doing well .
Regular exercise (at least 30 minutes several times a week) and a healthy body weight are just as important for healthy blood pressure. If you are overweight, you should discuss with your doctor how you can best reduce your fat deposits. The most important starting points are a lack of exercise and an unhealthy diet (e.g. many ready meals, sweets, high-fat snacks).
Smoking increases the risk of both types of stroke - cerebral hemorrhage and acute hypoperfusion - as well as many other health problems (such as cancer). So there are many good reasons to give up tobacco. You can find out more about the different smoking cessation methods here.
Drinking too much alcohol is another fine-tuning tool you can use to prevent stroke caused by intracerebral bleeding. By avoiding too much alcohol, you also avoid falls caused by intoxication, which can lead to a chronic subdural hematoma.
Head injuries - during exercise, for example - are also the most common cause of acute and subacute subdural bleeding, epidural bleeding and subarachnoid bleeding. With a protective helmet for sports such as skiing, mountain biking, climbing and horse riding, but also when cycling, you can significantly reduce your risk of cerebral haemorrhage in the event of an accident.
Tags: menopause parasites foot care





.jpg)