Hepatitis vaccination
and Sabine Schrör, medical journalist and Martina Feichter, medical editor and biologistDr. med. Mira Seidel is a freelance writer for the medical team.
More about the expertsSabine Schrör is a freelance writer for the medical team. She studied business administration and public relations in Cologne. As a freelance editor, she has been at home in a wide variety of industries for more than 15 years. Health is one of her favorite subjects.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
The hepatitis vaccination (hepatitis vaccination) protects against certain forms of virus-related liver inflammation (virus hepatitis). It enables your own immune system to react effectively to an infection with the pathogen in question. A hepatitis vaccination is only possible against hepatitis A and B. No vaccine is available against hepatitis C and other forms of viral hepatitis. Find out more about hepatitis vaccination here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. K73B19B18K75B16B17B15
What is the hepatitis vaccination?
There are different forms of viral hepatitis: Hepatitis A, B, C, D and E. Currently only one vaccination against hepatitis A and B is available. There are individual vaccinations (hepatitis A vaccination, hepatitis B vaccination) and a combined hepatitis A and B vaccination (hepatitis A-B combination vaccine). There is also a combination vaccination against hepatitis A and typhoid. Doctors typically administer them before traveling to risk areas.
In Germany there is no compulsory vaccination for hepatitis vaccinations. The Standing Vaccination Commission (STIKO) at the Robert Koch Institute (RKI) recommends hepatitis vaccination in some cases.
Depending on the mode of action, experts differentiate between active and passive hepatitis vaccination:
Active hepatitis vaccination
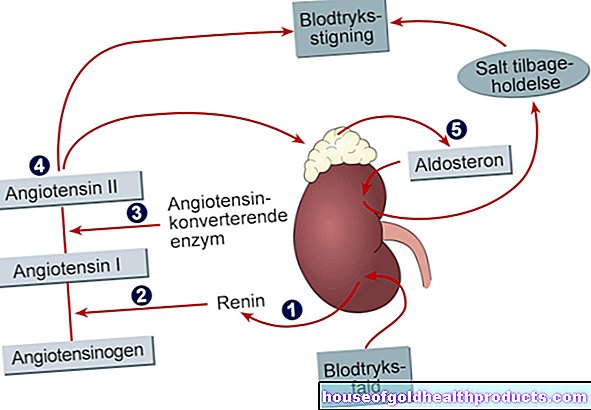
In the active hepatitis vaccination, components of the hepatitis A or hepatitis B virus are injected into the body, usually into the muscle of the upper arm. This stimulates the immune system to form specific antibodies against the respective pathogen. If there is later a “real” infection with the virus in question, the antibodies intercept it. This is how an outbreak of disease can be prevented.
The vaccines that are used in active hepatitis vaccinations are called dead vaccines. The hepatitis A vaccine usually contains killed viruses. It is therefore a whole particle vaccine. The hepatitis B vaccination, on the other hand, usually contains virus components (HBs antigen). Doctors speak of a split vaccine here.
After the active hepatitis vaccine has been given, it will take some time for the immune system to produce the specific antibodies. The vaccination protection is not given immediately. In return, it remains in place for years.
Passive hepatitis vaccination
The passive hepatitis vaccination consists of ready-made antibodies against the relevant hepatitis virus. They are usually obtained from the blood of infected patients and processed into a highly purified hepatitis vaccine.
The passive hepatitis vaccination gives immediate vaccination protection. However, this only lasts for a few weeks - until the body has broken down the administered (foreign) antibodies. This makes the passive hepatitis vaccination suitable, for example, for people who have recently had contact with sick people and may have become infected (post-exposure prophylaxis).
At the same time, they will be given the first dose of the active hepatitis vaccination (a single vaccine, as there are not enough hepatitis antigens in combination vaccines). Until this takes effect, the vaccinee is usually largely protected from disease thanks to passive immunization.
Before traveling to countries with an increased incidence of hepatitis, doctors only give the passive hepatitis vaccination in exceptional cases. Due to the longer incubation period, the active vaccination usually unfolds its effect before the disease is caused by the infection.
Hepatitis vaccination: costs
In many cases, the health insurance company will cover the cost of a hepatitis vaccination. The hepatitis B vaccination is a standard vaccination for all children. It is paid for by the statutory health insurance according to the vaccination guideline. The same applies to adults with a health and / or occupational risk of hepatitis infection.
The assumption of costs for a hepatitis A vaccination also depends on the respective indication. However, it is not a standard vaccination. The hepatitis A vaccination costs are usually covered if, as an employee of a medical laboratory, you are exposed to an increased risk of infection.
Many health insurance companies also cover the costs of a hepatitis vaccination for trips to risk countries. It is best to contact your health insurance company to find out more about the coverage of vaccination costs.
Hepatitis A vaccination
The hepatitis A vaccination is given intramuscularly, i.e. injected into a muscle. The doctor usually chooses the upper arm muscle for this.
Hepatitis A vaccination: who should be vaccinated?
The Standing Vaccination Commission (STIKO) recommends hepatitis A vaccination only as an indication vaccination for certain risk groups. This includes:
- People who have an increased risk of infection due to their sexual behavior (such as homosexual men)
- Patients who often receive blood components due to certain medical conditions (such as haemophilia)
- Patients with behavioral disorders or brain damage (such as stroke patients) who live in psychiatric facilities or comparable care facilities
Have an occupational indication for hepatitis A vaccination:
- Healthcare employees who are exposed to an increased risk of infection (laboratory employees, etc.)
- People who come into contact with wastewater at work (such as sewer workers, sewage treatment workers)
- Employees in day-care centers, children's homes, workshops for the disabled, asylum seekers' homes, etc. (including kitchen and cleaning staff)
In addition, experts recommend a hepatitis A travel vaccination for people who want to travel to regions where hepatitis A is more common (such as the Mediterranean region, Eastern Europe, many tropical regions).
Hepatitis A vaccination: how often do you have to vaccinate?
Two injections are required for the primary vaccination with the active hepatitis A vaccination: After the first vaccination, doctors give the second dose every six to twelve months. Two syringes are sufficient for the hepatitis A-typhoid combination vaccination.
Attention: The combined hepatitis A and B vaccination requires three vaccine doses (see below)!
Hepatitis A vaccination: booster
Long-term protection is achieved with the two vaccine doses of the hepatitis A primary vaccination series. It lasts for at least 12 years in adults, and possibly 20 to 30 years. In any case, experts assume that people with a healthy immune system do not need a hepatitis A booster after the basic vaccination course has been completed.
Only in certain cases, such as people with a weakened immune system, experts may advise titer control by means of blood tests - in other words, a measurement of the specific antibodies formed as a reaction to the hepatitis vaccination. A booster may be necessary if the antibody level is too low. The same applies if you suffered from hepatitis years ago.
Passive hepatitis A vaccination
You can also passively vaccinate against hepatitis A viruses. The finished antibodies administered offer protection against hepatitis A infection for about three months.
During this time, vaccinations with live vaccines (such as the vaccination against measles, mumps and rubella = MMR vaccination) should not be carried out. Their effectiveness can be weakened by the administered hepatitis antibodies.
Hepatitis B vaccination
The active hepatitis B vaccine was the world's first recombinantly produced vaccine. "Recombinantly produced" means that the constituents of the hepatitis B virus (HBV) contained therein are artificially produced with the help of genetically modified organisms.
The hepatitis B vaccine, like the hepatitis A vaccine, is injected into the muscle (intramuscularly, IM), usually the muscle of the upper arm. Then this hepatitis vaccination is most effective according to studies.
Hepatitis B vaccination: who should be vaccinated?
This hepatitis vaccination has been recommended by STIKO as the standard vaccination for all infants and young children since 1995. Hepatitis B disease is rare in these age groups, but carries a high risk of becoming chronic: acute hepatitis B only becomes chronic in around ten percent of cases in adults, but in around 90 percent of cases in infants and small children .
In adulthood, the STIKO recommends vaccination against hepatitis B as an indication vaccination for certain risk groups. These include, for example:
- People for whom a hepatitis B illness would likely be severe (this includes patients with an existing or expected immune deficiency or a pre-existing illness, e.g. hepatitis C patients, HIV-infected people, dialysis patients)
- People who live in the family or in shared apartments with people infected with hepatitis B
- People whose sexual behavior carries an increased risk of infection (for example because the sexual partner is changed frequently)
- Drug addicts who inject their addictive substance
- Pretrial detainees and convicts
- Job-related hepatitis B vaccination: People who are exposed to an increased risk of infection for hepatitis B in their job (such as medical staff, company first-aiders, police officers, social workers, etc.)
- Hepatitis B travel vaccination: travelers who stay for a long time in countries with high levels of hepatitis B virus infection or who have close contact with the local population
According to the current state of knowledge, anyone who has already had a hepatitis B infection cannot be infected again with hepatitis B viruses. A hepatitis vaccination against this type of virus is then not necessary.
Hepatitis B vaccination: how often do you have to vaccinate?
The hepatitis B vaccine can be administered to infants and young children as part of the six-fold vaccination together with the vaccines against diphtheria, tetanus (tetanus), polio, whooping cough (pertussis) and Haemophilus influenzae type b (Hib). According to current STIKO recommendations, three vaccination appointments are planned for basic immunization. According to the so-called 2 + 1 vaccination scheme, infants receive the injection syringes at the age of two, four and eleven months.
The STIKO recommends four vaccinations for premature babies, as was customary in the past. With the then valid 3 + 1 vaccination schedule, the doctor injects an additional hepatitis B vaccination in the third month of life.
Not all vaccines intended for primary immunization are approved for the reduced 2 + 1 vaccination schedule. Then the vaccination is given according to the 3 + 1 vaccination scheme (in months of life 2, 3, 4 and 11)!
The hepatitis B vaccine can also be given as a single vaccine. If the primary vaccination was missed in infancy, this hepatitis vaccination should be obtained before the child's 18th birthday.
Three doses are also provided for the indication vaccination for certain risk groups in adulthood: The second and third dose of the hepatitis vaccination against HB viruses are administered one month and six months after the first.
Rapid hepatitis B vaccination
An accelerated vaccination scheme is available for exceptional cases (when things have to go quickly, for example before unplanned trips): The three vaccine doses are administered at shorter intervals, for example within 21 days. The exact time intervals between the individual vaccine doses depend on the particular preparation. This accelerated vaccination schedule is not as effective and long-lasting as the normal vaccination schedule. An additional fourth dose after six to twelve months is therefore recommended for long-term protection.
Hepatitis B vaccination: booster
According to the Robert Koch Institute, a hepatitis B booster is generally not necessary if a complete basic immunization was carried out in childhood. It is assumed that the protection of this hepatitis vaccination will last for at least ten to 15 years, possibly even for life.
Even after a hepatitis B vaccination in adulthood, no booster vaccinations are usually necessary. In people with a weakened immune system (such as dialysis patients), however, it can make sense to check the level of hepatitis B antibodies in the blood regularly (titer control). If the antibody count falls below 100 IU / L (international units per liter), a booster vaccination is advisable.
In the case of people with a high risk of infection (such as certain occupational groups in the health care system) who received full basic immunization as a child, the vaccination protection is also checked and, if necessary, refreshed (check every ten years).
Hepatitis B vaccination: protection of newborns
Women who are infected with the hepatitis B virus (HBV) can transmit the pathogen to the child during pregnancy, childbirth or breastfeeding. Therefore, the babies of such mothers receive the first dose of the active hepatitis vaccine and a passive hepatitis vaccination against HBV (simultaneous vaccination) within twelve hours after birth. The other doses of the active vaccination will follow later (after one month and then again after five months at the earliest).
The newborn also receives this simultaneous vaccination for mothers with unknown hepatitis B vaccination status. There is a high probability that this will prevent infection in the child.
Hepatitis A and B vaccination in combination
Hepatitis A vaccination and hepatitis B vaccination can be given as a combined vaccine. There are three injections for the combination vaccine: The first two are given every four weeks. Doctors give the third vaccination about six months later. The combined hepatitis A & B vaccination can be injected from the age of two.
The combination vaccine hepatitis A & B is not suitable for people who may have been infected through contact with hepatitis A / B patients and who now want to protect themselves with a vaccination.
For this post-exposure prophylaxis, doctors always use a single hepatitis vaccine (plus a passive hepatitis vaccine). The reason: combination vaccines contain less hepatitis A antigen (with hepatitis B the concentration remains the same).
No hepatitis C vaccination yet
Like hepatitis B, hepatitis C can be chronic and lead to liver cirrhosis and liver cancer. Because the hepatitis C virus can change very quickly, scientists have not yet succeeded in bringing a vaccine against it onto the market. There is currently no vaccination against other forms of viral hepatitis either. The hepatitis E vaccine available in China is not approved in Europe.
Hepatitis vaccination: side effects
All drugs can have undesirable effects, including vaccinations such as the hepatitis vaccine. In this case, side effects usually consist of harmless and temporary reactions in the area of the vaccination site, such as:
- Redness
- swelling
- pains
- Hardening of the puncture site
- Swelling of the adjacent lymph nodes
In addition, side effects that affect the whole body may occur after a hepatitis vaccination:
- Exhaustion
- Gastrointestinal complaints
- fever
- Headache and pain in the limbs
- Allergic reaction
In detail, the following side effects are possible from the hepatitis A vaccination and hepatitis B vaccination:
Hepatitis A vaccination: side effects
The side effects of the hepatitis A vaccination include redness and painful swelling around the puncture site in around 10 to 20 percent of cases. In addition, general well-being can be impaired for a short time. Sometimes the vaccinee also develops fever, fatigue, head and body aches. Allergic reactions are rare.
Hepatitis B vaccination: side effects
Slight vaccination reactions such as redness, swelling, pain around the vaccination site and swollen lymph nodes are also evident with a hepatitis B vaccination. Side effects of other kinds, such as a slight fever, headache and body aches, or tiredness, rarely occur. In individual cases, allergic reactions occur.
Hepatitis vaccination & multiple sclerosis
The Hernán study in 1990 attracted particular attention: the hepatitis B vaccination was a possible trigger for multiple sclerosis (MS). The assumption was later examined in further studies, but has not yet been scientifically proven.
According to current expert opinion, the hepatitis B vaccination cannot trigger any flare-ups in existing MS.
Hepatitis vaccination: pregnancy & breastfeeding
Both hepatitis vaccinations can be given during pregnancy if there is an increased risk of infection. This can be the case, for example, if the pregnant woman comes into contact with the pathogens of hepatitis A or B at work (e.g. as a laboratory worker).
In principle, a hepatitis vaccination is also possible during breastfeeding. As a precaution, the following also applies here: The vaccination should only be carried out if it is really necessary.
Hepatitis vaccination: contraindications
Doctors do not give the hepatitis vaccines if they have an acute febrile infection. Known severe allergic reactions to the vaccine and / or its other ingredients are also contraindications for a hepatitis vaccination.
Tags: alcohol hair smoking