bacteria
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Some bacteria are important pathogens for infectious diseases. Most bacteria, however, do not cause illness in humans, but are in some cases even useful. For example, many "good" bacteria in our intestines help digestion. Read more about bacteria here: What is the structure of a bacterial cell? How big are bacteria? What types of bacteria are there? What are the main bacterial infectious diseases?
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. A01A37A56J14A36A39A54A74A55A00A15A35A02
Brief overview
- Bacteria - definition: microscopic unicellular organisms without a nucleus
- Are bacteria living things? Yes, because they meet the necessary criteria (such as metabolism, growth, reproduction).
- Bacteria reproduction: asexual through cell division
- bacterial diseases: e.g. tetanus, diphtheria, whooping cough, scarlet fever, chlamydial infection, gonorrhea, bacterial tonsillitis, bacterial pneumonia, bacterial otitis media, salmonellosis, listeriosis, tuberculosis, cholera, typhoid, plague
- Treatment of bacterial infections: antibiotics
- Vaccination against bacteria: possible e.g. for diphtheria, whooping cough, tetanus, meningococcal and pneumococcal infections, cholera, typhoid
What are bacteria
Bacteria are microscopic, unicellular organisms and the oldest living things on earth. They occur in many different ways and can be found virtually anywhere in the world - in the air, in water and in the ground, deep inside the earth's crust and on the tops of the highest mountains, in hot springs, and in the Arctic and Antarctic.
Countless bacteria cavort on the outer and inner surface of the human body (as well as other living beings), for example on the skin, in the oral cavity and in the intestines. This is normal and very important for our health. The "good" bacteria on the skin, for example, ensure that pathogenic germs cannot spread there. The bacteria in the intestine do the same and also help digest food.
Bacteria make up by far the largest proportion of the normal human flora (plus a few others such as fungi and parasites). The normal flora describes all microorganisms that naturally colonize the body. If experts only consider a certain place of colonization, they speak, for example, of intestinal flora (totality of all natural bacteria in the intestine).
There are also a few bacterial species that can cause diseases in humans. These types of human pathogenic bacteria only make up about one percent of all known types of bacteria.
Build up of bacteria
The size of bacteria is between 0.1 and 700 micrometers (one micrometer = one thousandth of a millimeter). This makes bacteria much larger than viruses, but in most cases still smaller than human cells.
Cell wall and flagella
A bacterial cell (like plant cells) usually has a cell wall. Their basic structure is formed by murein - a compound made up of two different sugars that are cross-linked by protein building blocks (amino acids). With some bacteria there is only one murein layer in the cell wall, with others several such layers. This, together with other differences in the structure of the cell wall, causes bacteria to take on different colors when using the so-called Gram staining method (see below: classification according to color).
In many cases the bacterial cell wall is rigid and gives the bacteria a fixed shape (e.g. spherical and rod-shaped bacteria). There are also screw-shaped bacteria with a thinner and relatively flexible cell wall. This allows the bacterial cell to move with helical (and other) movements. Bacteria with a rigid cell wall, on the other hand, usually have long, thread-like flagella, with which they are mobile (see below: classification according to flagella).
There are also a few bacteria without a cell wall. Examples are the mycoplasmas (bacteria living parasitically, which can nevertheless multiply themselves) and ThermoplasmSpecies (heat-loving bacteria with a stable plasma membrane that live in volcanic soils, for example).
capsule
Most bacteria also surround themselves on the outside with a capsule (see below: Classification according to encapsulation). This is a very dense protective layer made of sugars or protein components (amino acids), which is relatively sharply demarcated from the outside.
Another form of protection that some bacteria can develop independently of a capsule is a biofilm - a sticky substance that the bacteria secrete to attach to each other or to cells or objects. It can protect the germs from antibiotics. In addition, food residues can stick to the biofilm that caries bacteria form on the teeth (called plaque or plaque), which the bacteria can break down and use.
Cell membrane and cytoplasm
A cell membrane is attached to the inside of the cell wall of a bacterial cell, as is found with a similar structure in animal (including human) cells. Some bacteria also have an outer cell membrane. It surrounds the cell wall.
Inside the cell, i.e. in the cell plasma, also known as the cytoplasm, there are various other cell structures (such as the so-called ribosomes for protein synthesis), the genetic material of the bacterial cell, the so-called bacterial genome. Sometimes bacteria contain additional genetic material in the form of plasmids.
Bacteria genome
The bacterial genome contains all the genetic information of the bacterial cell that is necessary for life (information on structure, metabolism, reproduction). It consists of double-stranded DNA (English abbreviation for deoxyribonucleic acid), i.e. a double-stranded chain made up of certain sugar and other building blocks. The genetic material of animal cells is also made up of DNA. There are, however, essential differences between animal and bacterial cells:
- Animal cells: The DNA genome is separate from the rest of the cytoplasm in a separate, membrane-enclosed compartment - the cell nucleus. In addition, it is organized linearly, so it is in the form of individual chromosomes (quasi individual DNA threads).
- Bacterial cells: Their DNA genome is exposed in the cytoplasm, usually as a single ring-shaped (circular) structure. This is called the bacterial chromosome (also known as the nuclear equivalent or nucleoid) and is attached to a point on the cell membrane.
Plasmids
In addition to the bacterial chromosome, the cytoplasm of some bacteria also contains other small, double-stranded DNA rings in singles or plural, so-called plasmids. They contain genetic information that a bacterial cell does not need under normal living conditions, but which under certain circumstances ensure a survival advantage for it under difficult conditions.
This can, for example, be the blueprint for a poison (toxin) that kills other bacteria. The ability of a bacterial cell to be resistant to a specific antibiotic can also be stored in plasmids.
Antibiotics are drugs that are specifically effective against bacteria. They are therefore part of the standard therapy for bacterial infection.
Plasmids are replicated independently of the bacterial chromosome and, when a bacterium multiplies by cell division, distributed more or less randomly to the two daughter cells.
In addition, a bacterium can split its double-stranded plasmid into its two single strands and pass one of them on to another (plasmid-free) bacterium via a brief tunnel-like connection. This process is called conjugation. In both bacterial cells - the "donor" and the "recipient" - a matching second strand is then formed to match the individual plasmid strand, so that ultimately a complete circular plasmid is present in both bacterial cells. In this way, bacteria can, for example, pass on antibiotic resistance genes to one another.
The conjugation takes a few minutes, but is only possible between certain types of bacteria.
Bacteria vs. viruses
The most important difference is that bacteria have a metabolism and can multiply on their own - this does not apply to viruses. You can read more about the comparison between viruses and bacteria in the article Viruses.
What bacteria are there?
About 5,000 types of bacteria are currently known. In fact, there are probably many more: Experts suspect that there are hundreds of thousands of different types of bacteria in the world.
The germs can be classified according to various criteria; the most common are:
Classification according to the color
Bacteria can be classified according to the color they take on when they come into contact with certain stains. The most common staining method used to identify bacteria is called Gram staining. Accordingly, one differentiates:
- Gram-positive bacteria: they turn blue when a certain chemical substance is added. Examples of this are diphtheria and anthrax pathogens, pneumococci (trigger e.g. pneumonia, meninges, paranasal sinuses and otitis media) and streptococci (possible triggers, including pneumonia and tonsillitis).
- Gram-negative bacteria: They take on a red color when Gram staining. Examples of this are whooping cough, typhoid, cholera and plague pathogens.
The different coloring is based on the fact that the cell wall of the respective bacterial cells has a different structure. The most important difference is: The cell wall of gram-negative bacteria consists of a single murein layer, that of gram-positive bacteria consists of several murein layers.
The different wall structure also has practical consequences for medicine, specifically when it comes to the treatment of bacterial infections: some antibiotics only work against gram-positive bacteria, others only against gram-negative bacteria.
Classification according to the shape
There are three basic forms of bacteria:
- Globular bacteria: These round to oval bacteria (also called cocci) often cluster together in a typical way: in groups of two, four or eight, in larger clusters (staphylococci) or as more or less long chains (streptococci).
- Rod-shaped bacteria: The slender or clumsy rod-shaped bacteria can be present individually (like typhus bacteria) or in different positions to one another (like diphtheria bacteria). Rod bacteria, which need oxygen to live (aerobic) and can form spores (see below), are also called bacilli (e.g. anthrax bacteria).
- Helical bacteria: According to their exact appearance, these bacteria are divided into four groups - spirilla (e.g. the pathogen of rat bite fever), borrelia (e.g. borreliosis pathogen), treponema (e.g. syphilis bacteria) and leptospira (e.g. pathogen of leptospirosis).
Classification according to pathogenicity
Of the many different types of bacteria, only very few cause disease in humans and are therefore pathogenic (disease-causing). Specialists differentiate:
- Facultative pathogenic bacteria: These bacteria only cause disease under certain circumstances, for example when the immune system is weakened.
- Obligatory pathogenic germs: In sufficient quantities they always cause a disease, for example salmonella.
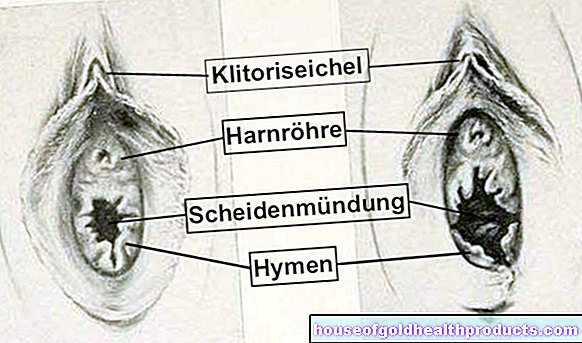
Bacteria that occur naturally in the body can also make you sick - for example if they spread excessively as a result of a weak immune system or end up in the wrong places in the body (e.g. intestinal bacteria that get into the urethra or vagina due to incorrect toilet hygiene). They are therefore among the facultative pathogenic bacteria.
Classification according to flagellation
Most bacteria have flagella on their outside, which help them to move. Experts differentiate between the following forms of flagellation:
- monotonic flagellation: only a single flagellum, e.g. cholera bacteria
- lophotric flagellation: several flagella, arranged in one or two tufts, e.g. Pseudomonas species
- perithric flagella: several flagella distributed over the entire outside of the bacterial cell (all around flagella), e.g. salmonella (pathogen of salmonellosis and typhus)
Classification according to encapsulation
Some bacteria surround themselves with a protective capsule. This prevents the germs in our body from being eliminated by certain defense cells (phagocytes). The fight against encapsulated bacteria is therefore generally more difficult for the immune system than against unencapsulated species.
The bacterium Haemophilus influenzae, for example, is encapsulated. It can cause meningitis, otitis media, bronchitis, pneumonia and - as Haemophilus influenzae type B (HiB) - laryngitis.
The pneumococci (Streptococcus pneumoniae) also belong to the encapsulated forms of bacteria. They typically cause pneumonia, but sometimes other bacterial infectious diseases as well.
Classification according to spore formation
Under unfavorable living conditions, some bacteria can develop permanent forms with a massively reduced metabolism - so-called spores. In contrast to metabolically active (vegetative) cells, these can withstand extremely unfavorable environmental conditions such as heat and cold and remain viable for years or even decades. As soon as the conditions improve again, the spore turns back into a vegetative bacterial cell.
Spores are practically sleeping bacteria.
The spore-forming bacteria include mainly representatives of the genera Bacillus and Clostridium, for example the anthrax pathogen (Bacillus anthracis) and the pathogens causing tetanus (Clostridium tetani) and botulism (Clostridium botulinum).
Classification according to the ratio to oxygen
Obligatory aerobic bacteria (aerobes) absolutely need oxygen to generate energy (aerobic respiration) and thus to live and grow. So-called microaerophilic bacteria also need oxygen. In contrast to obligatory aerobics, however, they only tolerate low oxygen pressure (lower than that in normal air).
The obligate anaerobic bacteria (anaerobes) are the exact opposite of the obligate aerobes: They cannot grow and thrive in the presence of oxygen - even small traces of oxygen can kill these bacteria in a short time.Unlike aerobes, they cannot eliminate toxic oxygen radicals (aerobic bacteria have special enzymes such as catalase for this). Obligatory anaerobic bacteria obtain their necessary energy either through fermentation or through so-called anaerobic respiration.
Facultative anaerobic bacteria are tolerant of oxygen: they can grow with or without oxygen. When oxygen is available, they get the energy they need through "normal" (aerobic) cellular respiration, just like aerobic bacteria and animal and human cells do. In an oxygen-free environment, on the other hand, their energy production takes place via fermentation or anaerobic respiration.
Aerotolerant bacteria can thrive in the presence of oxygen, but cannot use it for energy.
Chlamydia bacteria are special when it comes to energy generation: they cannot produce energy themselves, but have to use the energy from host cells. Therefore, they can only operate their metabolism and multiply within host cells. Outside of this, chlamydia can only survive as so-called elementary particles.
Classification according to temperature requirements
Depending on which temperature range bacteria prefer or tolerate, a distinction is made between three groups of bacteria:
- psychrophilic bacteria: They do best at five to ten degrees Celsius. The minimum temperature they can still tolerate is -5 to -3 degrees, depending on the type of bacteria, and their maximum temperature, depending on the type, is 15 to 20 degrees.
- Mesophilic bacteria: Their optimum temperature is 27 to 37 degrees. The temperature may drop to a maximum of 20 to 25 degrees. On the other hand, the temperature must not rise to more than 42 to 45 degrees.
- thermophilic bacteria: they feel most comfortable at 50 to 60 degrees. Depending on the type of bacteria, the temperature must not drop below 40 to 49 degrees and not rise to more than 60 to 100 degrees.
Classification according to the taxonomy
Like other living beings, bacteria are also classified according to scientific criteria into various hierarchical levels such as families, genera and species. Some types of bacteria can also be divided into different types (bacterial strains) - depending on the genetic factors and chemical composition.
How do bacteria multiply?
Bacteria multiply asexually through cell division:
First, the bacterial cell enlarges and doubles its genetic makeup (i.e. the bacterial chromosome). Then a new cell wall is drawn in between these two identical chromosomes until two identical (so to speak cloned) daughter cells have emerged from one bacterial cell. Basically, a bacterial cell simply constricts itself in the middle after doubling its genome.
How fast bacteria can multiply depends on the type of bacteria and the environmental conditions. Under optimal conditions, many bacteria can double their numbers in just twenty minutes.
When we talk about bacterial growth, we mean the increase in the number of bacterial cells. It is determined as the number of cells per milliliter.
What diseases are caused by bacteria?
There are a wide variety of diseases caused by bacteria. Here is a small selection:
- Scarlet fever: This very contagious bacterial infectious disease is triggered by the gram-positive, spherical A-streptococci (Streptococcus pyogenes).
- Other streptococcal infections: Streptococci A can also cause otitis media and tonsillitis, erysipelas, pneumonia and rheumatic fever. B streptococci (S. agalactiae) are possible triggers of meningitis and wound infections. Other streptococci can occur as caries bacteria.
- Pneumococcal infections: Pneumococci are also streptococci, which usually occur in pairs (diplococci). More precisely, it is Streptococcus pneumoniae. This bacterium is a typical cause of pneumonia, but can also cause meningitis, middle ear or sinusitis, among other things.
- Staphylococcal infections: They manifest themselves, for example, as wound infections, inflammation of the inner lining of the heart (endocarditis) or sepsis (bacterial "blood poisoning"). Infection with Staphylococcus aureus strains, which are resistant to methicillin and other antibiotics (MRSA), is particularly feared. These germs are often the cause of hospital infections.
- Meningococcal infections: Meningococcal bacteria are Neisseria meningitis. Infections with these germs usually appear in the form of meningitis (meningitis) or bacterial "blood poisoning" (sepsis).
- Gonorrhea (gonorrhea): This sexually transmitted disease is also caused by Neisseria bacteria, this time by Neisseria gonorrhoeae (also called gonococci). Treated in good time, gonorrhea usually heals without consequences. Otherwise there is a risk of permanent long-term effects such as infertility.
- Chlamydia infections: There are different types of chlamydia (sometimes with subgroups) that can cause different clinical pictures, for example conjunctivitis, infections of the urinary and genital organs (such as urethritis, cervical or prostate inflammation) and pneumonia.
- Whooping cough: Behind this "childhood disease", which is also increasingly occurring in adolescents and adults, is usually the gram-negative bacterium Bordetella pertussis.
- Diphtheria: The symptoms such as barking cough, swallowing difficulties and sweetish-putrid bad breath are caused by the toxin of the gram-positive rod bacterium Corynebacterium diphtheriae.
- Tetanus (tetanus): This dangerous disease is caused by bacteria of the type Clostridium tetani. The spores of these bacteria are mainly found in the soil (worldwide). People can get infected through small wounds on their hands while gardening, for example. In the body, the poison of the bacteria causes severe muscle spasms that can lead to death from suffocation.
- Tuberculosis: Mycobacterium tuberculosis is the most common cause of this serious, reportable infectious disease.
- E. coli infections: Escherichia coli is a gram-negative bacterium of which there are different strains. Some of them live naturally in the intestines of healthy people. Other E.coli strains, on the other hand, can cause infections, for example in the digestive or urinary tract (such as diarrhea and cystitis).
- Salmonellosis (Salmonella poisoning): The term describes infectious diseases and food poisoning caused by a certain subgroup of Salmonella bacteria. These include typhoid and paratyphoid fever.
- Listeria infection (listeriosis): This food poisoning is caused by gram-positive bacteria of the species Listeria monocytogenes. It is accompanied by nausea, vomiting, and diarrhea. You can become infected by eating contaminated foods such as dairy products, raw vegetables or meat that has not been sufficiently heated.
- Cholera: The gram-negative bacterium Vibrio cholerae is responsible for the severe diarrheal illness that occurs mainly in areas with poor hygienic conditions.
- Plague: The pathogen Yersinia pestis is also one of the gram-negative bacteria and is transmitted to humans by rat fleas. After several plague epidemics claimed millions of lives in the past, the disease is rare today.
Bacteremia and sepsis
Usually there are no bacteria in the blood. If so, it is called bacteremia. It can arise, for example, when someone gets bleeding gums from vigorously brushing their teeth or cuts themselves with a pocket knife. Bacterial infections (such as bacterial pneumonia) or during a dental or medical procedure can also get bacteria into the bloodstream.
Bacteremia does not always cause symptoms if the immune system clears the bacteria quickly.
Especially in people with a weakened immune system, the bacteria, if they romp in the blood for a long enough time and in large numbers, can also cause an infection (e.g. an inflammation of the inner lining of the heart = endocarditis). The result can be a very violent reaction throughout the body called sepsis ("blood poisoning"). In the worst case, it can lead to death. However, the risk of death varies considerably in individual cases. It depends, among other things, on the type of bacteria involved and how quickly the patient is treated.
Bacteria: transmission or infection
There are various ways in which people can become infected with pathogenic bacteria. Some bacteria can be transmitted via infectious droplets that are expelled by infected people, for example when they cough or sneeze (droplet infection). This is possible, for example, with scarlet fever and meningitis caused by meningococci.
For example, you can get infected with salmonella through smear infection: If people with salmonella-related diarrhea do not wash their hands thoroughly after using the toilet, they can transfer the germs to objects (such as doorknobs, cutlery). If a healthy person touches these objects and then grabs his mouth, nose or eyes, he can become infected. Direct person-to-person infection through smear infection is also possible if the infected person shakes hands with a healthy person with contaminated hands.
Salmonella is mainly transmitted through contaminated food. This path of infection also exists with some other bacteria such as listeria (pathogen of listeriosis) and representatives of the genus Campylobacter (pathogen of contagious diarrheal diseases).
The latter, like salmonella and some other bacteria, can also be transmitted via contaminated water.
In some cases, infection through sexual intercourse is possible, for example with chlamydia and the causative agent of gonorrhea (gonococci).
Bacterial infection: treatment
Bacterial diseases are treated with antibiotics as standard. These drugs specially developed against bacteria attack the cell wall or the metabolism of the bacteria. As a result, the germs are either killed or prevented from multiplying. In the second case, the immune system then has the chance to get the bacterial infection under control and eliminate the invaders.
Some antibiotics are effective against many different types of bacteria (broad-spectrum or broad-spectrum antibiotics), others are targeted against specific groups of bacteria (narrow-spectrum or narrow-band antibiotics).
Well-known groups of antibiotics are for example penicillins, cephalosporins, tetracyclines and macrolide antibiotics.
Not every bacterial infection requires antibiotic treatment. As an alternative or in addition, other measures may be useful that do not target bacteria, but at least alleviate the symptoms (e.g. pain relievers and anti-inflammatory drugs).
Vaccination against bacteria
Some infectious diseases caused by bacteria can be prevented with a vaccination. The administered vaccine stimulates the immune system to develop specific antibodies against the bacterial pathogen in question (active immunization). This means that the immune system is armed in the event that a "real" infection with these bacteria occurs later. The infection can be nipped in the bud at an early stage or at least weakened.
Examples of available vaccinations against bacteria:
- Diphtheria vaccination
- Whooping cough vaccination
- Tetanus vaccination (also available as passive immunization, in which finished antibodies are injected)
- Haemophilus influenzae type b vaccination (HiB vaccination)
- Meningococcal vaccination
- Pneumococcal vaccination
- Cholera vaccination
- Typhoid vaccination
Some of these vaccines are available as combination products of various compositions. For example, the Td vaccine protects against tetanus and diphtheria bacteria at the same time.
Tags: alternative medicine diet sports fitness