Varicocele
Clemens Gödel is a freelancer for the medical team.
More about the experts All content is checked by medical journalists.A varicocele (varicose vein hernia, varicocele testis) is the formation of varicose veins on the scrotum. The venous plexus at this point is palpably or visibly widened. Pain and a feeling of heaviness on the affected side of the testicle may or may not occur. The varicocele can usually be treated with a small operation. Find out more about the causes, symptoms, diagnosis and treatment of varicocele here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. I86
Varicocele: description
The varicocele is a varicose vein-like extension of the venous plexus (pampiniform plexus) of the testicle. In almost 90 percent of cases, the enlargement is on the left side of the testicle. The main causes of a varicose vein hernia are a weakness of the venous valves, which are supposed to prevent the blood from flowing back, or an obstacle to drainage. In addition to this so-called primary form of the varicocele, there is also a secondary (or symptomatic) form that is an expression of another disease such as a tumor.
The left and right branches of the testicular vein (vena spermatica or V. testicularis) drain the blood from the testes into the inferior vena cava - either directly (right testicular vein) or indirectly via the left renal vein (left testicular vein). If this drainage is disturbed at any point, the blood builds up in the testicles. This causes the vessels to expand and a varicose vein develops.
Testicular varicose veins can lead to infertility if left untreated. A third of all infertility cases are caused by a varicocele.
Varicocele: incidence
A total of 30 percent of men have a varicocele. Men aged 14 to 25 are particularly affected. The varicocele is rather rare in childhood. In elderly patients with a varicocele, a precise diagnosis is necessary, as these are mostly so-called secondary or symptomatic varicoceles. In this case, a tumor must be excluded as the cause of the varicose vein hernia.
Varicocele: symptoms
The varicocele is often asymptomatic and an incidental finding on examination.
In some sufferers, however, the typical varicocele symptoms also appear: a (felt) heavy, tense and full scrotum. The varicocele pain is particularly intense when standing. Worm-like swellings can be seen on the scrotum, which are visible either with or without increased abdominal pressure when pressing. The testicle on the affected side may be smaller, especially in children, due to inhibition of growth. This is an indication of impaired sperm production. In extreme cases, no sperm are produced at all (complete infertility).
Varicocele: causes and risk factors
Doctors differentiate between a primary and a secondary varicocele.
Primary (idiopathic) varicocele
The primary (idiopathic) varicocele is genetic. It makes up the vast majority of all cases of varicose vein hernia and occurs mainly on the left. The reason: the left testicular vein joins the left renal vein at a right angle (which then continues to the inferior vena cava), which makes blood flow more difficult and favors backflow. The right testicular vein, on the other hand, joins the inferior vena cava at a more acute angle (the acute angle is more favorable for blood flow).
A frequent cause of the blood backlog is a defect in the venous valves in the testicular vein or a congenital weakness of the vascular wall. A venous outflow disorder due to increased vascular pressure can also lead to a primary varicocele. The increase in pressure can come about because the left renal vein is pinched between two large arteries (nutcracker phenomenon). The resulting backlog of blood can damage the testicular veins.
Secondary (symptomatic) varicocele
The secondary or symptomatic varicocele can be bilateral. It is mostly caused by a drainage backlog caused by tumors. This is, for example, a tumor of the kidney, the renal pelvis or the ureter. A blood clot (thrombus) or tear (rupture) in the testicular veins is also a possible cause of a secondary varicocele.
infertility
In both the primary and the secondary form, there is a decreased blood return from the testes. The blood in the testicle flows more and more slowly. This causes the testicle to heat up, which affects sperm production and quality. Infertility can arise.
In addition, the axis of testicular-associated hormones (such as FSH - follicle-stimulating hormone) can be disturbed. On the other hand, through the backflow of blood or even blood backflow, hormones of the adrenal gland can get into the testicles and cause damage there.
Varicocele: examinations and diagnosis
The urologist is a specialist in diseases of the testicle and thus also for the varicocele. In a conversation with the patient (anamnesis), he first records the symptoms. Possible questions are, for example:
- Do your testicles feel heavy or swollen?
- Are the symptoms worse when standing?
- Do you have pain?
Physical examination
Then the doctor will first examine the testicle while standing. Due to the force of gravity, the varicocele is usually clearly visible. If this is not the case, the patient is asked to increase the pressure in the abdomen by pressing or tensing the abdominal muscles. This often makes the swelling of the vessels more visible.
In the next step, the patient lies down. In the case of a primary varicocele, the vascular markings on the testicle will spontaneously diminish when you lie down, which means that the vessels empty due to gravity. If this is not the case, it can be suspected that it is a secondary varicocele.
Ultrasound examination
Another important step in the diagnosis of a varicocele is an ultrasound examination (sonography) of the testicle. The doctor can assess the varicocele more precisely. In addition, the kidneys and the abdomen should be examined with ultrasound - in search of possible explanations for the drainage disorder. In order to confirm the blood congestion or even backflow, an examination using Doppler sonography, a special form of ultrasound examination, should be carried out.
Hormone and sperm tests
If you want to have children or if you suspect infertility, further examinations should be carried out. The determination of hormones and a more detailed examination of the sperm status (spermiogram) is recommended in patients with testicular varicose veins. Testicles play an essential role in fertility.
Vascular x-ray (phlebography)
If a vascular malformation is suspected, a so-called phlebography is carried out: With the help of X-ray contrast media, an X-ray image of the vessels is made in order to examine their course and condition.
Varicocele: severity classification
A varicose vein on the testicle can be divided into three degrees of severity:
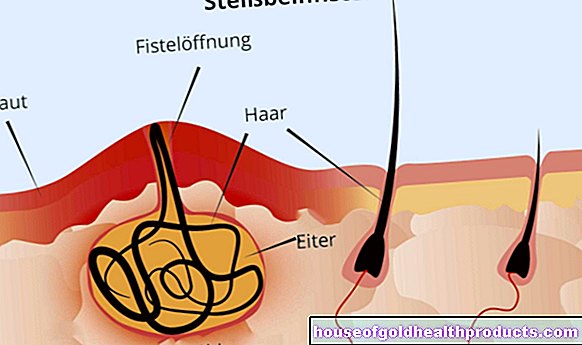
- Grade I: palpable expansion of the venous plexus in the testicle when pressing while standing; Vessel size <1 centimeter.
- Grade II: vasodilatation that can be felt without additional pressure; Vessel size 1 to 2 centimeters.
- Grade III: palpable and visible vascular tangle; Vessel size> 2 centimeters.
Varicocele: treatment
Treating a varicose vein in the testicle is important for several reasons. For one thing, the symptoms can be very uncomfortable, and for another, there is an increased risk of infertility.
There are no drugs against a varicocele. Instead, the therapy of choice is mostly a minor surgical procedure. It should be carried out when:
- there is repeated pain
- the testicle volume has decreased
- it is a grade III varicocele
- the varicocele is perceived as a disability
There are a number of different procedures available to treat primary varicocele. The therapy of the secondary varicocele depends on the underlying disease, for example the tumor.
Varicocele sclerotherapy
The enlarged vessels in the testicle can be sclerosed. This means that a substance is injected into the vessels, which "desolates" them. The blood can flow well through other blood vessels.
The sclerosing agent can be introduced via a catheter. In what is known as retrograde transcatheter sclerotherapy, a catheter is pushed through an inguinal vein and renal vein to the venous plexus in the testicle under local anesthesia. The sclerosing agent is then injected through the catheter. In around 30 percent of cases, however, this form of varicocele therapy is unsuccessful.
You can also make a small incision at the base of the penis and insert the catheter directly into the venous plexus. Here, too, a sclerosing agent is injected. This is then known as antegrade or anterograde sclerotherapy.
Vascular occlusion through embolization
Another treatment option for a varicocele is to artificially close the affected vessel. To do this, you can either insert tissue glue into the vessel or insert a tiny spiral.
Operative procedures
As a final treatment option, surgical procedures are available for a varicocele. The affected vessel is tied off and severed. This can be done as part of a larger, open varicocele operation or by means of buttonhole surgery (laparoscopy): In this, only several small incisions are made, through which the surgical instruments are inserted.
Varicocele: disease course and prognosis
It is very important to start therapy early and therefore in good time with a varicocele. The prognosis after successful treatment is usually good. Although increased vigilance is required, the danger of sterility is mostly averted.
An untreated varicocele leads to severe damage to sperm formation, reduced testicular volume and decreased function of the testicular cells (Leydig cell function). However, symptom-free varicoceles that have no effect on sperm quality need not be associated with these complications.
In the case of severe sperm damage (azoospermia, oligo-astheno-teratozoospermia), surgical therapy is not promising. In these cases alternative fertilization techniques should be advised.
A good therapy of the varicocele leads to freedom from pain and an increase in testicular volume in over 80 percent of patients. It is assumed that the sperm quality will also increase again.
Tags: therapies nourishment desire to have children