Frostbite
Tanja Unterberger studied journalism and communication science in Vienna. In 2015 she started her work as a medical editor at in Austria. In addition to writing specialist texts, magazine articles and news, the journalist also has experience in podcasting and video production.
More about the experts All content is checked by medical journalists.Chilblains (also perniones) are inflamed, red-bluish, itchy and painful skin changes (e.g. swelling) that are caused by the cold and reduced blood flow. They often appear on the hands and feet, especially the fingers and toes. Chilblains usually heal on their own within a few weeks. Sometimes the doctor will prescribe vasodilator drugs and nourishing ointments. Read more about the topic here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. T69

Brief overview
- Description: Reddish-bluish, itchy and painful skin changes caused by cold and humid climates. Mostly appear on toes and feet as well as hands and ears.
- Causes: Chilblains occur when the blood vessels contract due to the cold and the tissue is not adequately supplied with blood.
- Treatment: Chilblains usually heal on their own, but the use of vasodilating drugs and nourishing ointments is advisable depending on the severity. Warmth (e.g. warm clothing) supports healing.
- Course: Chilblains are usually harmless and will heal on their own within a few weeks. However, complications such as pain, scars and infections are possible, which last significantly longer.
- Symptoms: The skin is swollen, reddish to bluish in color (spots). The skin itches, burns and hurts. In some cases, blisters appear on the skin and, rarely, ulcers.
- Diagnosis: Talk to the doctor, examine the skin for changes such as swelling, discoloration, deformation and injuries.
- Prevention: wearing warm clothing, getting enough exercise, refraining from alcohol and smoking.
What are chilblains?
Chilblains or pernions (Latin Perniones) are red-bluish, mostly itchy and painful changes in the skin, e.g. swellings, spots or nodular thickenings (papules) that are caused by the cold. Therefore, they often occur in the cold season.
Frostbite already occurs at temperatures around freezing point, for example during winter sports.
Chilblains are the result of circulatory disorders. Areas of the body with less blood flow, such as the hands and feet, especially the fingers and toes, are therefore particularly prone to chilblains. Colloquially, chilblains are also called "winter toes". But the face, ears and nose as well as the heels, thighs and lower legs are often affected by chilblains.
A distinction is also made between chilblains, which occur acutely, i.e. a short time or a few hours after exposure to the cold, and chilblains, which occur chronically when the body is repeatedly exposed to the cold.
Chilblains are not frostbite in which ice crystals form in the tissue and are usually harmless.
How do frostbite develop?
Chilblains are a reaction of the body to cold temperatures and humid climates. Frostbite is particularly common when the outside temperature is around freezing point. In damp, cold weather, the blood vessels contract due to the cold. The tissue is then no longer adequately supplied with blood - and therefore also not with oxygen. Due to the lack of oxygen, the tissue is damaged and inflamed, which causes the typical skin changes.
Often there is no apparent cause why some people are prone to chilblains. However, it is possible that chilblains may occur due to other medical conditions. Chilblains are known to be the result of the autoimmune disease lupus erythematosus. In addition, chilblains occur in connection with neurological disorders such as Aicardi-Goutières syndrome (ABS), a rare hereditary disease of the brain.
Studies also indicate that chilblains-like skin changes occur in some people during or after an infection with SARS-CoV-2 (so-called "COVID toes" or "Corona toes"). However, further investigations still have to show what connections there are here.
What are the risk factors?
In addition to the cold, high humidity and wind encourage frostbite to develop. People who spend more time outdoors (e.g. when riding, cycling or motorcycling) are more likely to suffer from chilblains. Those who do not protect themselves adequately from cold, damp weather (e.g. with gloves, hat) or wear clothes that are too tight (e.g. shoes that are too tight) also promote the development of frostbite.
People with poor circulation are also more likely to develop chilblains. People who smoke and drink alcohol are also at increased risk of developing chilblains. Women are also more often affected than men. Low body weight and BMI also seem to increase the risk of chilblains.
What can you do about chilblains?
Most of the time, chilblains heal on their own. However, depending on the severity, the use of vasodilator drugs and nourishing ointments prescribed by the doctor is advisable. In addition, warmth supports healing. On the other hand, those affected are better off avoiding the cold.
warmth
Basically, frostbite will go away on its own within a few weeks. Warmth is a reliable means of relieving symptoms and preventing further frostbite. At the first signs of frostbite, it is best to warm the affected area immediately.
To do this, for example, place your warm, dry hands on the frostbite or run lukewarm water over it. You should absolutely avoid water that is too hot or direct contact with a hot heater. This additionally damages the already attacked skin areas.
Warm clothing such as gloves, thick socks, earmuffs or a blanket can also help against frostbite. Warming teas and soups are also recommended for frostbite. They warm the body from within. It is also best to avoid the cold as much as possible until the chilblains have healed.
Never rub the frostbite with snow! This makes the symptoms even worse and there is a risk of the skin becoming severely inflamed.
Move
Exercise also helps to stimulate blood circulation in the vessels. Endurance sports are particularly suitable: hiking, long walks, swimming or cycling not only ensure better blood circulation, but also strengthen the immune system.
Home remedies
The effectiveness of home remedies for chilblains has not yet been adequately documented. In general, it is advisable to integrate alternating showers, Kneipp showers and more exercise into your everyday life in order to promote blood circulation. Ointments containing extracts of marigolds or lanolin nourish the skin.
To alleviate the symptoms of chilblains, some people swear by home remedies such as oak bark and horsetail baths, healing earth bandages or rubbing with tea tree oil.
Before using home remedies for chilblains, ask your doctor for advice.
Other measures
Avoid alcohol and smoking whenever possible. These substances damage the blood vessels. If pain occurs (usually when you warm up the affected areas of the skin), short-term pain relievers (e.g. ibuprofen) will help. It is best to ask your doctor which agent and which dosage is suitable for you.
When to the doctor
Most of the time, chilblains are harmless and do not need to be treated by a doctor. If there are no additional discomfort or severe pain, the chilblains will heal on their own.
In severe cases, however, inflammatory wounds develop on the affected areas of the skin. To avoid further complications such as infections or ulcers, consult a doctor immediately in these cases. If you keep getting swelling due to the cold, a visit to a doctor is also recommended. This is because it is possible that the tissue will deteriorate over time or that you suffer from a disease that promotes chilblains (e.g. an autoimmune disease such as lupus erythematosus). If the chilblains spread or if it takes longer than two weeks to heal, it is also advisable to see a doctor.
If the affected areas are severely inflamed, the doctor usually prescribes ointments and creams containing cortisone, which you apply several times a day yourself. In severe cases, take the medication as a tablet. Depending on the severity, the doctor supplies the skin inflammation with sterile wound dressings. If the itching is severe and painful, he gives antihistamines.
In pronounced cases, the doctor treats chilblains with vasodilator drugs (e.g. calcium channel blockers such as nifedipine or diltiazem). However, the effectiveness of this has so far only been insufficiently investigated.
If an underlying disease such as arteriosclerosis ("hardening of the arteries") is responsible for the circulatory disorders, the doctor treats it and recommends measures to promote blood circulation (e.g. more exercise, alternate showers). Sometimes he prescribes anticoagulant drugs such as acetylsalicylic acid in low doses (e.g. 100 mg per day), which the patient takes permanently.
It is important that you go to your follow-up visits until the chilblains have completely healed to reduce the risk of complications.
How long do you have frostbite?
As a rule, chilblains are harmless. The itchy, painful swellings usually resolve on their own within one to two weeks (a maximum of six weeks). However, if the endangered parts of the body are repeatedly exposed to the cold without protection, chronic swellings may develop, which will cause recurring complaints years later.
In some cases, severe disease can lead to complications such as ulcers, infections and inflammation of the subcutaneous fat (cold panniculitis). It usually takes significantly longer for these to heal. As a result, scars, thinning skin or flaky skin changes are also possible. In rare cases, the skin on the affected area dies.
Be sure to have a doctor clarify chilblains, especially if they have occurred several times!
What do frostbite look like?
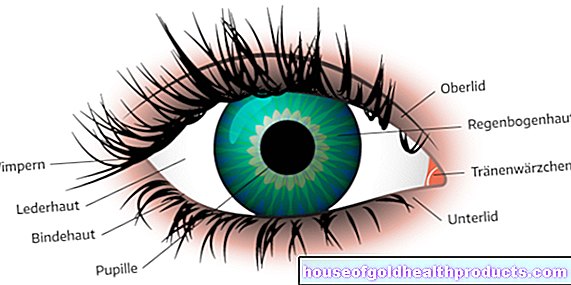
Chilblains usually look reddish or bluish at the beginning. Later on, the affected areas of the skin are often swollen and painful. The skin feels cold and damp (doughy). When heated, the frostbite usually itches and burns. Sometimes it tingles and feels furry. Those affected often report abnormal sensations in the affected area, such as the feeling of "pins and needles" on the skin.
The skin is usually bulged, bulges slightly upwards and reacts painfully to pressure. Sometimes blisters form on the skin. In severe cases, it is also possible that ulcers develop that extend into the subcutaneous fatty tissue. If the chilblains do not heal properly, scars remain.
Where does frostbite often occur?
Chilblains most often appear on the outside of the fingers and toes, as well as the back of the hands and feet. The face, ears (especially the ear lobes) and nose, as well as the front and outer sides of the lower thighs and thighs, are also frequently affected by chilblains.
How does the doctor diagnose frostbite?
If the person concerned notices painful or unusual skin changes, the family doctor is the first point of contact. If necessary and for further examinations, he will refer you to a dermatologist.
Talk to the doctor
Before examining the skin, the doctor will have a detailed discussion with the person concerned (anamnesis). In the anamnesis interview, for example, he asks questions about when the skin changes occurred, whether they occurred suddenly or have developed over a longer period of time and whether they have already occurred several times.
He also asks about possible triggers, such as whether you have been outside in the cold for a long time or whether you have other diseases (e.g. lupus erythematosus, arteriosclerosis).
Physical examination
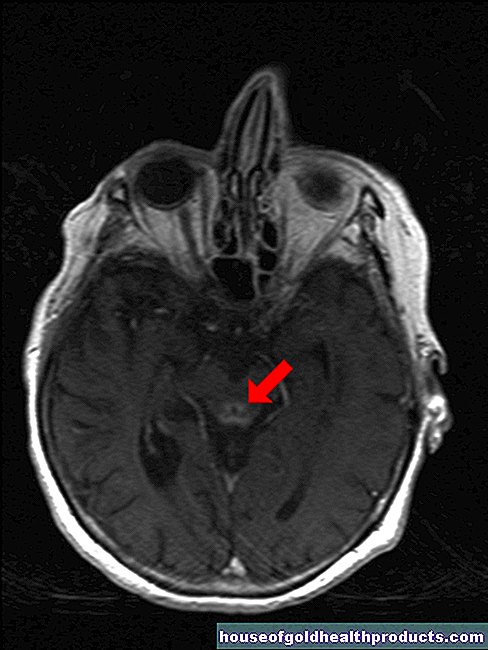
The doctor then examines the skin for any visual abnormalities (e.g. deformations, injuries, swellings, discoloration). He examines the skin closely (e.g. with a special skin magnifier or a microscope) and, if necessary, scans it.
The doctor often diagnoses the chilblains based on the typical skin changes (so-called eye diagnosis). He also uses palpation to check the texture of the skin and the underlying tissue and whether the changes in the skin are painful.
Most of the time, based on the symptoms described and the physical examination, the doctor can tell quite quickly whether it is chilblains.
If the symptoms indicate another illness, it is necessary to carry out further examinations in order to track down the basic problem (e.g. blood tests).
How do you prevent chilblains?
The best protection against chilblains is to avoid the cold. Protect your body with warm clothing (e.g. gloves, hat, socks) that do not constrict. Use waterproof and breathable clothing in cold, damp weather.
When it comes to clothing, make sure that you cover your head well. This is where the body radiates most of the heat. Avoid tight shoes or gloves. They cut off the blood supply in the vessels and are more likely to encourage chilblains to develop. Constricting bracelets, stockings or belts also inhibit blood flow.
Exercise on cold days helps prevent chilblains. You should therefore exercise regularly, even in the cold, to stimulate the blood circulation in your body. It is important that you get back into the warmth quickly after exercising in the fresh air, as the evaporative cooling that occurs when you sweat cools your body down.
Also refrain from alcohol and smoking. Both substances damage your blood vessels and have a negative effect on your immune system.
After treating the chilblains, it is advisable that you continue to care for the damaged skin areas with creams so that the skin damage is limited. In cold and wet weather, the best way to protect your facial skin is with a thick oil or cold cream. Ask your doctor or pharmacist which creams are right for you as some can irritate your skin.
Tags: medicinal herbal home remedies Diagnosis sex partnership