Lyme disease test
and Martina Feichter, medical editor and biologistFabian Dupont is a freelance writer in the medical department. The human medicine specialist is already doing scientific work in Belgium, Spain, Rwanda, the USA, Great Britain, South Africa, New Zealand and Switzerland, among others. The focus of his doctoral thesis was tropical neurology, but his special interest is international public health and the comprehensible communication of medical facts.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
A reliable Lyme disease test or even a Borreliosis rapid test has been researched for a long time. Because a reliable Lyme disease diagnosis is not easy because of the often unspecific symptoms. Borreliosis is easy to treat, especially if it is discovered early. Here you can find out more about the diagnosis of Lyme disease and possible tests!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. M01G01A68
Lyme disease diagnosis: symptoms show the way
The most important indication of a Lyme disease diagnosis is the typical rash at the tick bite site: the "wandering red" (erythema migrans). It is considered to be the leading symptom of early Lyme disease and occurs in many patients. For this reason, you should keep an eye on the surrounding skin area for several weeks after a tick bite. It often helps to write a little note in the calendar every week to check the position again. If you notice a change in your skin, you should see a doctor.
Unfortunately, a tick bite often goes unnoticed or is forgotten. If you or your doctor still suspects Lyme disease, consider whether there is a general possibility of a tick bite - for example through frequent walks in the forest, picnics in the meadow, regular forest / gardening or jogging in summer. Your doctor will ask about this as part of the anamnesis (medical history).
Sometimes a borreliosis infection goes undetected for a long time and only makes itself felt months or years later with late manifestations such as joint inflammation (Lyme arthritis), late neuroborreliosis or chronic skin inflammation (acrodermatitis chronica atrophicans). Even with such complaints, the doctor thinks of a Lyme disease infection, among other things.
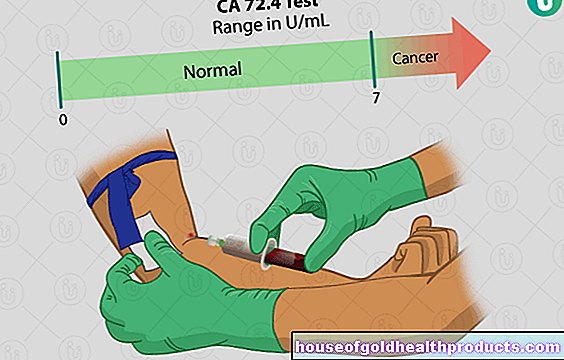
Lyme disease test for antibodies
If Lyme disease is suspected, laboratory tests are necessary for clarification. Various borreliosis tests are available for this. Many of them focus on specific antibodies against the borreliosis pathogens (Borrelia). Doctors summarize these antibody tests under the term Borrelia Serology.
Detection of antibodies in the blood
These borreliosis tests (1st stage: ELISA, 2nd stage: immunoblot) look for specific antibodies against Borrelia in a patient's blood sample. However, a positive result alone is not sufficient to diagnose Lyme disease. Lyme disease symptoms must also be present. In addition, both false negative and false positive test results are possible.
False negative result
A Borreliosis test for antibodies in the blood can show a Borrelia infection only a few weeks after the infection. Only then does the immune system develop specific antibodies against the Borrelia. At the time of the characteristic rash ("wandering redness"), the borreliosis test can therefore still be negative (in about half of the cases).
Otherwise, a negative test result does not necessarily mean that the patient does not have Lyme disease. In some people, the immune system produces little or no antibodies against Borrelia. Sometimes this is due to a genetic predisposition, in other cases to a weakened immune system.
Borreliosis tests can also be falsely negative in patients who are being treated with immunosuppressants for another illness. Immunosuppressants are drugs that suppress the immune system.
False positive result
The antibody borreliosis tests can also show false positive results. This is the case, for example, if the patient actually suffers from syphilis (syphilis). Because both syphilis and borreliosis pathogens are among the screw bacteria (spirochetes). The tests then confuse the pathogens due to their similar structure.
Viral infections with EBV (glandular fever), hepatitis or varicella (chickenpox and shingles) and some autoimmune diseases can also cause false-positive results.
A positive Lyme disease test alone is not conclusive
If a Lyme disease test is positive, it usually only means that the patient has been infected with Borrelia at some point in time. However, a positive antibody test alone does not allow a statement to be made as to whether it is a florid infection (with actual symptoms) or a latent ("hidden") infection. In the second case, the patient has become infected with Borrelia, but these are kept in check by the immune system so that the disease does not break out.
A Lyme disease blood test can also still be positive if an infection was long ago and has long been healed - either with the help of the body's defenses alone or through antibiotic therapy. Borrelia antibodies are often still detectable in the blood.
A positive Lyme disease blood test may only be interpreted as evidence of Lyme disease in connection with typical symptoms and the patient's history (tick bite).
If there are no typical Lyme disease symptoms or only unspecific symptoms such as tiredness, malaise, headache and body aches or fever, the doctor usually does not carry out a Lyme disease test. Because the test result would have no consequences.
Neuroborreliosis: detection of antibodies in the CSF
If, based on your symptoms and the information from the anamnesis, you suspect neuroborreliosis, the doctor will take a sample of the cerebrospinal fluid (nerve fluid, liquor) from you. This is done as part of a liquor puncture. In the laboratory, the liquor sample is then examined for antibodies against Borrelia, among other things.
However, the detection of specific antibodies in the nerve water (in connection with typical symptoms) is not sufficient to be able to make a diagnosis of "neuroborreliosis". In addition, the nerve water must show certain inflammatory changes. You can find out more about the diagnosis of Borrelia infestation in the nervous system in the article Neuroborreliosis.
Direct pathogen detection
The detection of specific antibodies is very important for the diagnosis of Lyme disease. As a support, the Borrelia can be detected directly in the patient's sample material - on the one hand by cultivating the bacteria, on the other hand by detecting the Borrelia genome.
Borrelia culture
Here one tries to cultivate the bacteria from the patient sample. The sample can, for example, come from the pathologically altered skin or the cerebral / spinal cord fluid (if neuroborreliosis is suspected).
If such a Borrelia cultivation from sample material is successful, it is definite evidence of borreliosis. However, this process is very time-consuming and laborious and is only carried out in a few special laboratories.
Borrelia PCR
Alternatively, the genetic material of the Borrelia can be detected in the patient samples. Genetic fragments can be reproduced by means of PCR (polymerase chain reaction) and then detected. This is faster than a Borrelia cultivation. The doctor initiates this type of Lyme disease test especially if the doctor suspects a borreliosis-related joint inflammation (Lyme arthritis) or neuroborreliosis.
Both Lyme disease tests are used if previous examinations could not provide clear results - for example, if the person affected does not develop enough Borrelia antibodies due to a weak immune system.
The professional societies do not recommend (routine) direct pathogen detection from the blood or urine!
Borrelia detection in the tick
Some laboratories offer Lyme disease tests for submitted ticks. The detection is usually carried out by means of the polymerase chain reaction (PCR), which is why the term tick PCR is often used for short.
A positive test result does not automatically mean that the bacteria were also transmitted to humans. If an infected tick has sucked blood on a person for less than 24 hours, the likelihood of Borrelia transmission is very low. There is a high probability that the person affected does not have Lyme disease.
In addition, some laboratories generally test the ticks for the genetic makeup of Borrelia burgdorferi sensu lato: This is a large group of closely related Borrelia genospecies, some of which cause Lyme disease, but others do not - at least according to the current state of knowledge. If the tick borreliosis test is positive, the affected tick may only be infected with Borrelia, which does not cause Lyme disease in humans.
The detection of Borrelia in ticks is not suitable for making therapy decisions.
The doctor does not treat patients with antibiotics solely on the basis of a positive tick test result. The doctor adheres to the current guideline recommendations. You speak out against a tick PCR.
Non-recommended Lyme disease tests
In addition to the detection of Borrelia in ticks, there are a number of other Borreliosis tests that the specialist societies do not recommend based on the current state of knowledge. In most cases, there is a lack of meaningful scientific studies that prove the benefit of the respective tests. These include:
- Lymphocyte transformation test (LTT Borrelia; it can also be positive in people who have never been in contact with Borrelia)
- Lymphocyte population CD57 + / CD3- (similar to LTT)
- Antigen detection from various body fluids (no reliable informational value)
- Xenodiagnosis (this involves letting the tick larvae suck up blood from alleged Lyme disease infected people and then examining the larvae for Borrelia, not proven benefit, very time-consuming)
- Light microscopic detection (risk of confusion)
- Visual Contrast Sensitivity Test (grayscale test; measurement of the detection of gray tones under the assumption that a special Borrelia neurotoxin is harmful to the eye, but not guaranteed)
- Over the counter tests (too imprecise)
Conclusion: Lyme disease diagnosis is difficult
Lyme disease can be very diverse in terms of its symptoms and course. This makes diagnosis more difficult, especially in later stages of the disease. In addition, symptoms such as those that occur with Lyme disease can also have other causes (differential diagnoses).
For example, a supposed "wandering redness" can actually be a non-specific reaction of the skin to an insect bite, rubella (in children) or erysipelas. Neurological symptoms, such as those shown in neuroborreliosis, can also occur with TBE (early summer meningoencephalitis), a herniated disc or multiple sclerosis.
That means: Lyme disease is first of all a clinical suspicion diagnosis. The assumption, in turn, arises from the patient's symptoms and medical history. Positive results from borreliosis test procedures corroborate the suspicion. If the doctor can also rule out other possible causes for the symptoms, the diagnosis of Lyme disease is considered confirmed.
Tags: pregnancy travel medicine laboratory values