Palliative medicine treatments
Nicole Wendler holds a PhD in biology in the field of oncology and immunology. As a medical editor, author and proofreader, she works for various publishers, for whom she presents complex and extensive medical issues in a simple, concise and logical manner.
More about the experts All content is checked by medical journalists.Just as a coat (lat. "Pallium") protects the body from the cold, palliative treatment aims to protect the quality of life and self-determination of critically ill people. Most of these are cancer patients, but other incurable diseases are also treated with palliative care.

The term "palliative" is used when the disease can no longer be assumed to be cured. This is the case, for example, when a tumor or remnants of it can no longer be removed or there are daughter tumors (metastases). That doesn't always mean death is imminent. Despite an incurable disease, a patient can easily reach old age. Palliative therapy is not necessarily limited to the last phase of life, but can begin at an early stage of the disease. Palliative care units in clinics as well as inpatient and outpatient palliative and hospice services offer palliative care.
Goals of palliative care
The focus of palliative medicine is the person. Doing everything so that he can make the most of the remaining life time is a priority. Life extension is not the ultimate goal. Usually a conflict arises automatically in this difficult situation, because life-extending measures do not always go hand in hand with a better quality of life. The demands on life and the assessment of what is worth living depend on personal ideas that the doctor and patient have to develop individually. The final decision is made by the patient.
Other goals of palliative treatment in addition to quality of life and independence can be:
- Preservation of vital organ functions (e.g. intestinal obstruction due to the tumor)
- Avoidance of life-threatening complications (e.g. shortness of breath)
- Reduction of metastases
- Relief from pain
- Treating depression, fear of death, or the dying process
- Symptom relief in the case of shortness of breath, cough, nausea, vomiting, confusion, restlessness, etc.
- Wound care
Medical Palliative Treatments - Benefit or Harm?
Palliative medicine uses procedures that are also used curatively, i.e. for healing. Each of these measures burdens the body and is usually associated with side effects (in the case of cancer, for example, headache, nausea, vomiting, hair loss, etc.). Here, benefits and burdens have to be weighed up in each individual case.
A palliative operation is not directed against the cause of the disease, but is intended to prevent complications, for example if a growing tumor or daughter tumors (metastases) block vital organ functions. If a tumor closes the intestine (ileus), an artificial anus (anus praeter) must be placed. Even if the surgeon cannot correct a congenital heart defect, but creates a circulatory situation that enables survival, it is called a palliative operation. However, every intervention is itself associated with a risk. Various factors (old age, poor general or nutritional condition) can speak against an operation.
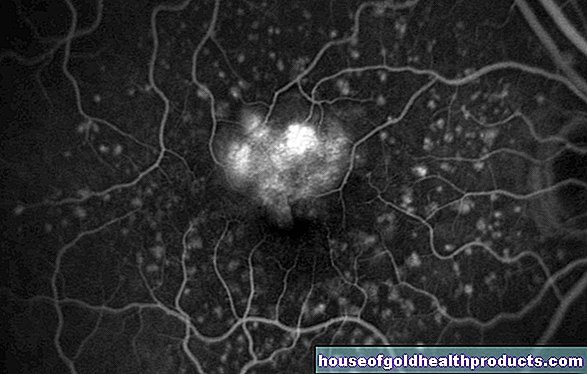
Palliative radiation therapy is intended to combat metastases or reduce the size of a tumor. Bone metastases, such as those common in breast, prostate, and lung cancers, penetrate the bone and are associated with severe pain and the risk of fractures. Radiation can relieve the suffering and increase bone strength. If a tumor presses on the windpipe or the superior vena cava (for example in lung cancer), the result is shortness of breath, a feeling of suffocation or a blocked return flow of the blood to the heart. Then, too, radiation can help. Metastases often form in the brain as the disease progresses. The failure of brain functions leads to neurological symptoms such as blindness, paralysis, cramps. Since brain metastases often occur more frequently, whole-brain radiation is useful. However, individual brain metastases can also be irradiated in a targeted manner.
Palliative chemotherapy is designed to bring cancer to a standstill and slow down further growth or spread via metastases. Tumor tissue and metastases that the surgeon was not able to remove completely or not at all due to their location or size can possibly be reduced in size using chemotherapy. Intravenous palliative chemotherapy is based on so-called cytostatics, special drugs that have a (systemic) effect on the whole body. By combining various cytostatics, their effect can be increased.
Palliative antibody therapies have been possible in addition to chemotherapy for a number of years. By binding to receptors, antibodies prevent certain messenger substances in the body from transmitting a growth command to the tumor or from forming new blood vessels in the tumor.
Medicinal palliative therapy
With drug-based palliative therapy, side effects and physical stress can be kept to a minimum if the dosage and dosage form are optimal.
One of the most important factors for the quality of life of the seriously ill is effective pain therapy. Various groups of drugs are available for this, which are administered as tablets, juice, plasters or also subcutaneously or intravenously via so-called pain pumps. Opiates are often used. Helpful substances include cortisone, co-analgesics, and antidepressants. Since February 1st, 1999, a cannabis relative can be prescribed as a drug (dronabinol) in Germany as an anesthetic. Alternative methods such as acupuncture and physiotherapy complement pain therapy.
Drug therapy can also help with numerous other complaints, such as nausea, constipation, loss of appetite, depression, anxiety, restlessness and panic, increased intracranial pressure or shortness of breath.
What else helps
Many complaints such as pain, tension or shortness of breath can be reduced with the right physiotherapy. Which includes:
- Classical physiotherapy
- Respiratory therapy
- Exercise bath
- Complex physical decongestive therapy
- Transcutaneous electrical nerve stimulation, electrical stimulation
- Colon, connective tissue, foot reflexology and classic massage
- Fango, hot air, red light
Both the terminally ill and their relatives benefit from psychological support. Methods of palliative psychotherapy are:
- Talk therapy
- Crisis intervention
- Stress reduction
- Psychoeducation through education and training
- Relaxation procedure
- Art, creative and design therapy
- Mediation of self-help groups
Nutritional therapy plays a big role. Because of the disease and its treatment, those affected often struggle with loss of appetite, nausea, and vomiting. In addition, side effects such as oral mucosal inflammation or taste and swallowing disorders make it difficult to eat. The result is weight loss. In this stressful situation, however, the body is dependent on a good supply of energy. It can be done orally and artificially.
Eating and drinking normally is possible with oral nutrition. There are the following recommendations:
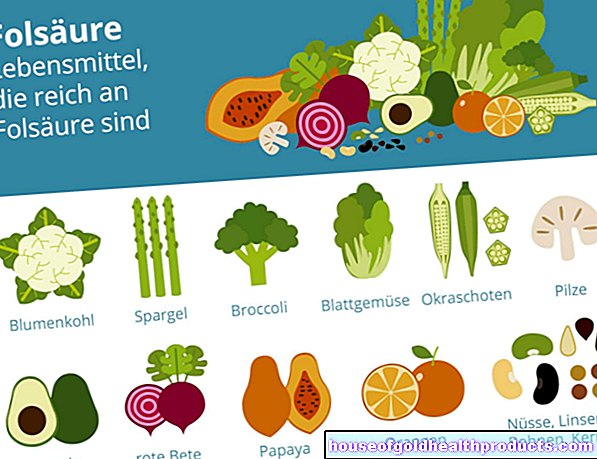
- Wholesome and vitamin-rich food, fresh food, plenty of fluids
- Refrain from alcohol, coffee and high-fat foods
- no diet: enough protein and fat!
- several small meals spread over the day
- appealing presentation
- Preparation and presentation adapted to individual restrictions (porridge, drinking food)
Artificial nutrition distinguishes between:
- enteral: feeding tube (stomach tube), the intestinal function is preserved
- parenteral: bypassing the digestive tract, supplying nutrients via infusions into the vein
Eating activates all the senses and should bring joy. Artificial nutrition therefore seldom increases the quality of life or lifespan, but it may occasionally be necessary. The patient must decide in good time which procedure he prefers. In principle, relatives should accept the patient's eating and drinking behavior. Artificial nutrition is rarely indicated in the last phase of life. It is usually part of the dying process that the dying person refuses to eat.
Tags: book tip desire to have children digital health



.jpg)















.jpg)