Hospital infections (nosocomial infections)
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Some patients get even sicker in a hospital than they were before: The term "nosocomial infections" refers to infections that a person gets in a health care facility - especially in hospitals, which is why one also speaks of hospital infections. By definition, all infections detected 72 hours or later after admission to the clinic are classified as nosocomial.

Nosocomial infections are one of the most common complications that arise in the treatment of hospital patients. Nationwide, around 500,000 patients get a nosocomial infection every year. An estimated 15,000 patients die each year from hospital infections.
Doctors and clinics are obliged to precisely document nosocomial infections. In addition, such infections (as well as the suspicion of them) must be reported to the health department.
Development of nosocomial infections
The causes of hospital infections can essentially be divided into four groups:
»Patient factors: The diseases or health problems to which patients owe their inpatient stay also make those affected more susceptible to infectious agents. If, for example, the patient's immune system is weakened due to cancer or diabetes, germs that are already in the body have an easy job and can multiply rapidly. In addition, other personal factors such as malnutrition and surgical wounds can increase the likelihood of hospital infections. Age also plays a role. Older and very young patients (such as premature babies) are more susceptible to nosocomial infections.
»Environment: Many sick people in a relatively small space, contaminated medical instruments and devices, nurses or doctors with non-disinfected hands - the clinical environment itself carries a certain risk of infections in the patients.
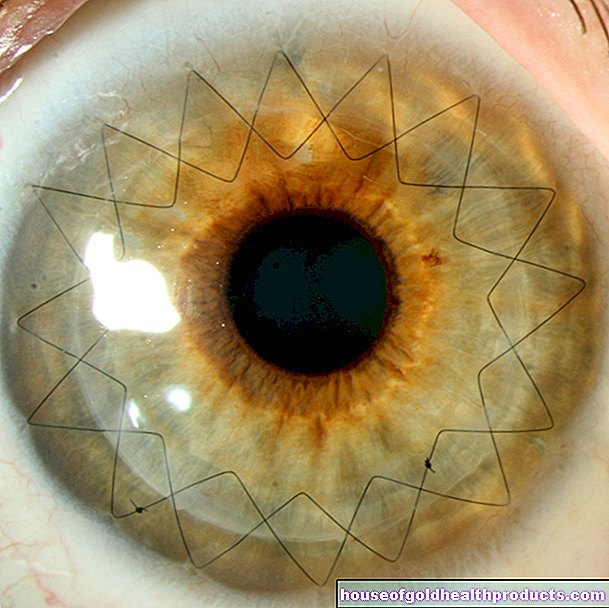
»Technology: Modern medical technology makes it possible to monitor and care for patients better. The devices (e.g. catheters, dialysis or ventilation devices) offer infectious agents but also additional entry points into the patient's body.
»Human factors: High work pressure can mean that the nursing staff and doctors no longer have enough time for adequate hygiene measures.
The likelihood of a nosocomial infection also depends heavily on the type of pathogen. Above all, its virulence (ability to cause disease), its ability to survive in the hospital environment and its resistance properties are decisive. So are the bacteria, for example Staphylococcus aureus and Pseudomonas aeruginosa frequent pathogens of hospital infections because they are very virulent and insensitive to many antibiotics (multi-resistance).
The main pathogens
Nosocomial infections are caused by bacteria in about 71 percent of cases, while viruses are the triggers in about 21 percent. The rest is due to fungi and parasites.
The main bacterial pathogens causing hospital infections are Staphylococcus aureus, Escherichia coli, Pseudomonas aeruginosa and so-called enterococci. Many of them also occur on or even in the body of healthy people, but do not cause any damage because the immune system keeps them under control. In sick or immunocompromised people, the penetration of such pathogens can trigger a nosocomial infection.
MRSA
This becomes particularly problematic when the germs have become insensitive to appropriate drugs (antibiotics) - they are then difficult to fight. MRSA plays an important role among these multi-resistant bacteria. These are bacteria of the type Staphylococcus aureusthat have become resistant to methicillin and many other common antibiotics (MRSA = methicillin-resistant / multi-resistant S. aureus).
These resistant germs like to colonize skin surfaces and mucous membranes (e.g. in the nose, throat, groin). If they manage to enter the body through an open wound or a urinary catheter, for example, they can make you sick. For treatment, the affected person receives antibiotics to which the germ is not yet "immune". In addition, the affected person is isolated from other patients because MRSA can easily be transmitted through the hands. Thanks to its resilience, the pathogen can survive for a long time on objects such as doctor's coats or medical instruments. Therefore, strict hygiene measures are necessary when handling and caring for MRSA patients.
The most common nosocomial infections
Urinary tract infections are the most common form of nosocomial infections. More than 80 percent of them are caused by a urinary catheter. This is a thin plastic tube that is pushed through the urethra or abdominal wall into the bladder and is used to drain the urine (e.g. in the case of voiding problems). The longer a catheter is in the bladder, the more likely it is to develop a urinary tract infection.
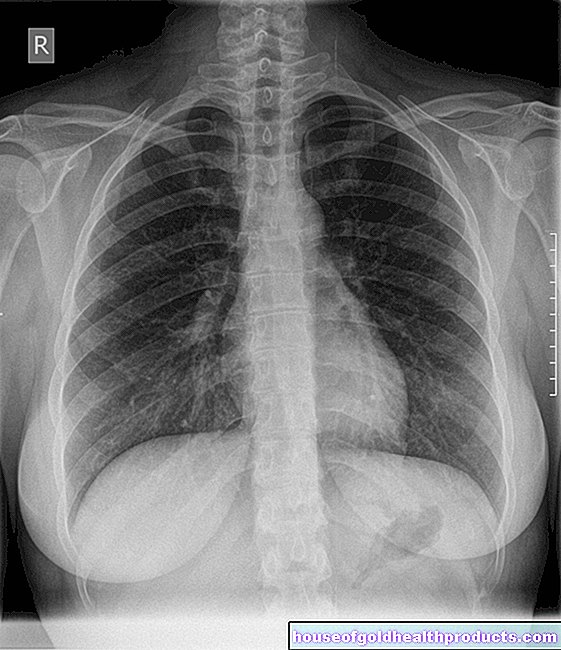
Respiratory infections are the second most common type of hospital-acquired infection. The most important is pneumonia, which is very feared due to its high mortality rate (up to 50 percent). Some groups of patients in hospitals are particularly prone to nosocomial pneumonia. This applies, among other things, to patients who:
- are in an intensive care unit,
- be artificially ventilated,
- Receiving antibiotics or drugs that suppress the immune system (immunosuppressants)
- have had major surgery on the abdomen or chest or
- are of advanced age.
The third most common hospital infection is wound infections after surgery. Every year around 160,000 postoperative wound infections are diagnosed in German clinics.
Other diseases that patients can catch in hospital are the infiltration of bacteria or fungi into the bloodstream (bacteremia, fungemia). They are triggered, for example, by pathogens that enter the body via the intestinal tract or a catheter. Sometimes bacteria or fungi are also introduced directly into the bloodstream (e.g. with prolonged intravenous feeding). Bacteremia can also develop secondarily in the course of other infections (such as pneumonia, pelvic inflammation). If the bacteremia or fungemia causes clinical symptoms, doctors speak of blood poisoning (sepsis).
Infections transmitted by blood and blood products are particularly problematic (blood products are, for example, stored blood). Such infections are mainly hepatitis B and C and HIV.
Consequences of nosocomial infections
Hospital infections can make a patient's condition significantly worse and delay the healing process. As a result, those affected have to stay longer in the clinic. This also means an increase in treatment costs. Sometimes hospital-acquired infections (such as sepsis or pneumonia) can also become life-threatening and lead to the death of the patient. For example, the risk of death for operated patients doubles if they develop a hospital infection.
Prevention of nosocomial infections
Hand washing is one of the most important measures to prevent healthcare-associated infections. Nursing staff are required to clean their hands thoroughly before and after each patient contact. This is particularly important in sensitive areas such as intensive care units and departments for blood cancer patients (hematological-oncological wards). Visitors should also pay attention to cleanliness and hygiene (hand disinfection is mandatory before entering the intensive care unit).
Hygiene is of course also very important in the hospital environment, with medical devices and instruments. Corresponding hygiene regulations for the prevention of hospital infections are therefore laid down in the Infection Protection Act.
Tags: hospital elderly care sports fitness
.jpg)