Corneal transplant
Updated on All content is checked by medical journalists.With a cornea transplant (keratoplasty) the cornea of a deceased organ donor is transplanted into the patient. This is especially necessary if the cornea is cloudy after severe inflammation or injuries. Read everything you need to know about the transplant procedure, when it will be performed, and the risks involved.

What is a corneal transplant?
A corneal transplant is an operation in which a patient receives the cornea from a dead donor. The cornea forms the outer layer of the eye and is approximately 550 micrometers thick. It makes an important contribution to the ability to see. Opacities, such as those that occur after a severe corneal inflammation or injury, as well as abnormal bulges can therefore lead to loss of vision. In order to restore the function of the eye, the patient needs a corneal transplant.
What do you do with a cornea transplant?
If the ophthalmologist has determined the need for a corneal transplant, a suitable transplant is sought in a so-called corneal bank at eye clinics. However, not every patient has an immediate turn because the demand clearly exceeds the supply.
The actual operation is performed either under local or general anesthesia. Depending on how big the clouding is on the patient's cornea, the ophthalmologist will either completely or partially remove it. Then he cuts the donor cornea to size and sutures it to the patient's eye. The threads remain in the eye for several months to years because wounds there heal very slowly.
Further development of the classic corneal transplant
Corneal transplants have been around since 1905. In most cases, a transplanted cornea is not as perfectly shaped as the patient's natural one. That is why ophthalmologists (ophthalmologists) have been researching since the 1990s to separate and transplant only the innermost two of the five-layer cornea (the endothelium and Descemet's membrane). These two layers are only ten micrometers thick and can be cut to the exact size of the area to be transplanted. This further development of the classic corneal transplantation is called DMEK transplantation.
While visual acuity of around 30 percent can be achieved with the classic procedure, it is around 80 percent with DMEK transplantation.
What are the risks of a corneal transplant?
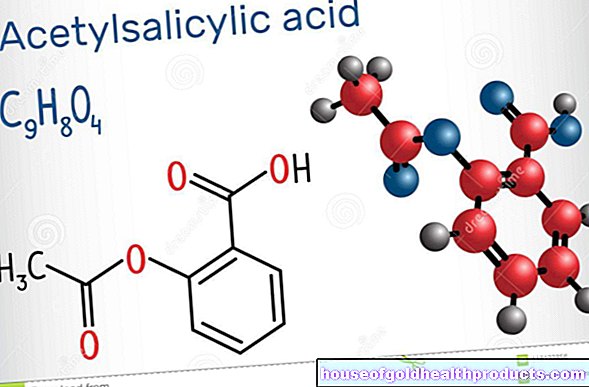
As with all transplants, there is also a risk of a rejection reaction with a corneal transplant if the immune system fights the foreign tissue. This can lead to renewed clouding and loss of vision. However, medication can prevent this reaction.
What do I have to consider after a cornea transplant?
Pay attention to symptoms such as tearing, redness and impaired vision and report any symptoms to your doctor as soon as possible. In addition, avoid mechanical irritation of the eyes, for example from rubbing. It is also important that you keep regular check-ups with your ophthalmologist. If the corneal transplant results in complications, these can be identified and treated as quickly as possible.
Tags: diet Diseases magazine