Atorvastatin
Updated onBenjamin Clanner-Engelshofen is a freelance writer in the medical department. He studied biochemistry and pharmacy in Munich and Cambridge / Boston (USA) and noticed early on that he particularly enjoyed the interface between medicine and science. That is why he went on to study human medicine.
More about the experts All content is checked by medical journalists.The active ingredient atorvastatin belongs to the so-called statins - a group of active ingredients that can lower high cholesterol levels. Too much cholesterol in the blood encourages hardening of the arteries, which can lead to coronary artery disease and stroke, among other things. Here you can read everything you need to know about the cholesterol lowering drug atorvastatin, side effects and use.
This is how atorvastatin works
Atorvastatin is a member of the statins - a group of drugs that can lower high cholesterol levels.
Cholesterol is an essential substance that the body needs, among other things, to build cell membranes and to form hormones and bile acids (for fat digestion). The body produces around two thirds of the required amount of cholesterol in the liver. The remaining third is obtained from food.
In order to lower high cholesterol levels, one can reduce the body's own production with medication on the one hand and change unfavorable eating habits on the other.
Atorvastatin reduces the body's own cholesterol production: it is a complex process that involves many steps. An important and rate-limiting step depends on a specific enzyme called HMG-CoA reductase. This enzyme inhibit statins like atorvastatin. This reduces self-production and lowers the cholesterol levels in the blood.
This applies above all to the blood values of the "bad" LDL cholesterol (LDL = low-density lipoprotein), which can lead to hardening of the arteries. The blood values of the "good" (vascular protecting) HDL cholesterol (HDL = high-density lipoprotein), on the other hand, sometimes even increase.
The total amount of cholesterol and the amount of triglycerides (TG) - another type of blood lipid level - are also reduced by the effects of atorvastatin.
Uptake, breakdown and excretion
Atorvastatin is quickly absorbed into the body after it has been taken by mouth (orally). Unlike other statins, it does not have to be converted into the active form in the liver first, but can take effect immediately.
The maximum effect is reached about one to two hours after ingestion. Since the body produces cholesterol most intensively during the night, atorvastatin is usually taken in the evening.
Due to its long duration of action, a once-daily dose is sufficient. Atorvastatin, which is metabolized in the liver, is mainly excreted in the stool.
When is atorvastatin used?
Atorvastatin is mainly used to treat high levels of cholesterol in the blood (hypercholesterolaemia). In general, cholesterol-lowering drugs such as atorvastatin are only prescribed if non-drug measures to lower cholesterol (healthy diet, exercise and weight loss) have not been successful.
Atorvastatin is also approved for the prevention (prevention) of cardiovascular complications in patients with coronary artery disease (CHD) or at an increased risk of cardiovascular disease (such as those with diabetes). This application is independent of the level of cholesterol.
In both cases, it is used over the long term in order to permanently lower the cholesterol level to certain values. The lower the values achieved, the better.
This is how atorvastatin is used
Atorvastatin is usually taken as a tablet once a day in the evening. The dose is determined individually by the attending physician, but is usually between ten to eighty milligrams.
Regular intake is important for the success of the treatment, as the cholesterol levels in the blood usually change over a period of several weeks. The patients do not "notice" the effect of the cholesterol lowering agent directly, although it can be measured in the blood and is reflected in a reduced incidence of heart attacks and strokes.
Do not stop atorvastatin on your own just because you "don't see any effect" yourself.
If necessary, atorvastatin is combined with other drugs, for example with the colestyramine or ezetimibe (both also lower the cholesterol level).
What are the side effects of atorvastatin?
Common side effects (affecting one to ten out of a hundred patients) of atorvastatin therapy are:
- headache
- Gastrointestinal disorders (such as constipation, gas, nausea, diarrhea)
- changes in liver enzymes
- muscle pain
Notify your doctor if you have muscle pain or discomfort during atorvastatin therapy.
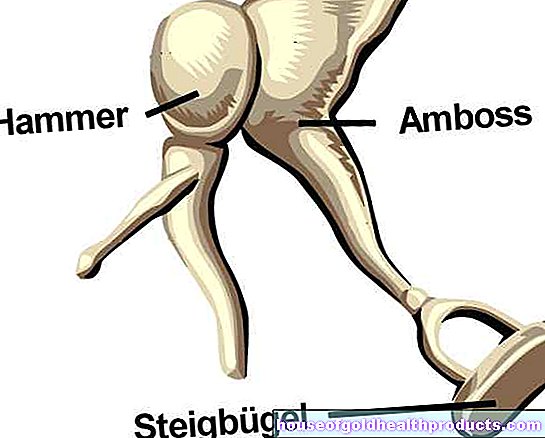
Uncommon side effects (i.e., side effects affecting less than one percent of people) include insomnia, weight gain, drowsiness, vomiting, abdominal pain, and rashes. A lack of blood platelets (thrombocytopenia), vision problems, hearing problems and angioneurotic edema (special form of edema) are even rarer.
What should be considered when taking atorvastatin?
Contraindications
Atorvastatin must not be taken if:
- severe liver dysfunction
- simultaneous treatment with certain drugs for hepatitis C therapy (glecaprevir and pibrentasvir)
Interactions
Since atorvastatin is broken down, among other things, by the enzyme cytochrome 3A4 (CYP3A4), inhibitors for this enzyme lead to increased levels and thus increased atorvastatin side effects. Such CYP3A4 inhibitors should therefore not be combined with atorvastatin:
- certain antibiotics: erythromycin, clarithromycin, fusidic acid
- HIV protease inhibitors (e.g. indinavir, ritonavir, nelfinavir)
- certain antifungal agents: ketoconazole, itraconazole, voriconazole
- certain heart medications: verapamil, amiodarone
Other drugs that should not be combined with the cholesterol lowering drug because of a possible increase in atorvastatin side effects are:
- Gemfibrozil (lipid lowering agent from the group of fibrates)
Grapefruit (juice, fruits) - also a CYP3A4 inhibitor - should also be avoided during atorvastatin therapy. Even a glass of grapefruit juice in the morning causes twice as high atorvastatin levels to be measured the following night as usual. The possible consequence is unexpected side effects.
Conversely, substances that stimulate the activity of the enzyme CYP3A4 (CYP3A4 inducers) can accelerate the breakdown of atorvastatin and reduce its effect. These include rifampicin (antibiotic), efavirenz (HIV drug), St. John's wort and some anti-epileptic drugs (e.g. carbamazepine, phenytoin).
Age restriction
The treatment of children and adolescents is only carried out in special cases and is subject to certain restrictions to be clarified by the doctor. In principle, atorvastatin is approved for the treatment of hypercholesterolemia from the age of ten.
pregnancy and breast feeding period
Pregnant and breastfeeding women should not take atorvastatin. If use during breastfeeding is absolutely necessary, breastfeeding should be discontinued before starting atorvastatin therapy.
How to get medication with atorvastatin
Atorvastatin requires a prescription in Germany, Austria and Switzerland and is available in pharmacies upon presentation of a doctor's prescription.
How long has atorvastatin been known?
After the biosynthesis of cholesterol was elucidated in the early 1950s, it quickly became apparent that by inhibiting important key enzymes, effective drugs against high cholesterol levels could be produced.
A first inhibitor called mevastatin was isolated from a fungus in Japan in 1976, specifically against the enzyme HMG-CoA reductase. However, this was never brought to market.
In 1979, scientists isolated lovastatin from a fungus. During the investigation, synthetically modified variants of lovastatin were also developed, whereby the compound MK-733 (later simvastatin) proved to be therapeutically more effective than the starting material.
Simvastatin, a so-called type 1 statin, was later used to develop the newer type 2 statins such as atorvastatin, which is two to three times more effective. It was approved in the USA in 1996 and launched in Germany in 1997.
Since the patent expired in 2011, numerous generic products have been developed, which has resulted in a sharp drop in the price of atorvastatin.
Tags: unfulfilled wish to have children laboratory values stress