Breast cancer
and Maria Franz, M.Sc. Biochemistry and medical studentMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts
Maria Franz has been a freelance writer in the editorial team since 2020. After completing a master's degree in biochemistry, she is currently studying human medicine in Munich. With her work at she would like to arouse her own great interest in medical topics among the readers as well.
More about the experts All content is checked by medical journalists.Breast cancer (breast cancer) is the most common cancer in women. It rarely occurs in men. A genetic predisposition and older age promote the development of breast cancer. Alcohol, smoking, obesity and hormone preparations also increase the risk of the disease. Read more about the topic here: How do you recognize breast cancer? What favors its creation? How is it diagnosed and treated? How can you prevent breast cancer?
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. D05C50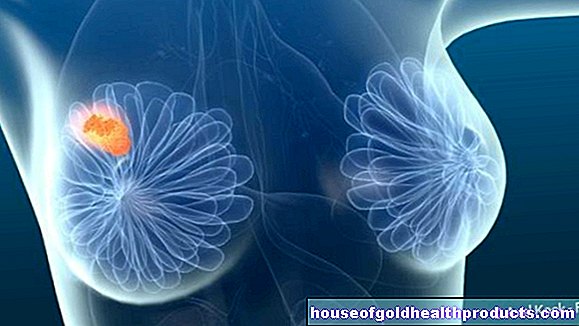
Brief overview
- What is breast cancer? Malignant tumor of the breast, also called breast cancer; most common cancer in women
- Frequency: One in eight women will develop breast cancer in their lifetime (lifetime risk). Men rarely get breast cancer: in the course of their life, it affects one in 800 men.
- Forms of breast cancer: invasive ductal breast cancer (starting from the milk ducts), invasive lobular breast cancer (starting from the glandular lobes), less common forms (e.g. inflammatory breast cancer)
- Risk factors: female gender, older age, genetic predisposition, hormonal factors (such as early first menstrual period plus late onset of menopause, taking hormone preparations, late first pregnancy / no pregnancy), alcohol, smoking, sedentary lifestyle, obesity, high-fat diet; in men, undescended testicles as well as previous inflammation of the testicles or epididymis
- Possible symptoms: Lumps or hardening in the breast, change in shape or size of a breast, change in color or sensitivity of the breast skin or nipple, retraction of the breast skin or nipple, discharge of clear, cloudy or bloody secretion from a nipple, reddening or scaling that does not subside the breast skin etc.
- Treatment options: surgery, radiation therapy, chemotherapy, anti-hormone therapy, targeted therapies (such as antibody therapy)
- Prognosis: If detected and treated in time, breast cancer is usually curable.
Breast cancer: general
Breast cancer (breast cancer, carcinoma mammae or Mamma-Ca for short) is a malignant growth in the breast. Doctors also speak of a malignant (malignant) tumor of the breast. Certain cells in the mammary gland change their genes and multiply in an uncontrolled manner. They grow into healthy tissue (invasive growth) and destroy it. In addition, individual cancer cells can spread in the body via the blood and lymphatic system and form new growths elsewhere (metastases).
Frequency of breast cancer
Breast cancer is the most common cancer in women. But what many do not know: Men can get breast cancer too! However, that rarely happens. They only make up one percent of all breast cancer cases. In 2020, however, over half a million women developed breast cancer in Europe.
The mean age of onset for women is around 64 years and for men around 72 years. About a quarter of patients die from breast cancer. However, the chances of recovery are much better today than in the last few decades. On the one hand, according to experts, this is due to the advances in breast cancer treatment. On the other hand, regular screening examinations have become established.
Suspicious tissue changes
When the cells of a tissue multiply, experts speak of hyperplasia. If a new tissue growth forms as a result, experts call this neoplasm. Initially, this tissue change can only be determined in the laboratory, later a "lump" can form in the breast. The good news is, most of the nodular changes discovered in the breast are benign and do not affect healthy tissue. Breast cancer, on the other hand, can develop from suspicious tissue changes (risk lesions).
Cancer does not develop from every breast lump. The doctor can tell you whether a tissue change is harmless or dangerous.
The risk of developing breast cancer from a tissue change increases in older women and if there are already cases of breast cancer in the family. As a rule, the doctor therefore decides on a case-by-case basis whether to initially only observe a discovered tissue change in the chest area or to treat it immediately.
Breast Cancer - Risk Lesions
Different cell types can proliferate in the breast and cause risk lesions. These are not necessarily precancerous stages. Rather, these tissue changes encourage breast cancer to develop.
If cells in the glandular lobes are abnormal, doctors speak of lobular neoplasia (LN), also known as lobular intraepithelial neoplasia (LIN). An LN increases the risk of breast cancer by 4 to 12 times. It can be further subdivided into the less dangerous "atypical lobular hyperplasia" (ALH), in which the glandular lobule retains its shape, and "lobular carcinoma in situ" (LCIS), in which the glandular lobe expands because of the large number of new cells.
Cells in the milk ducts can also multiply in an uncontrolled manner. If these cells actually look "normal" and are only present in large numbers, doctors speak of common ductal hyperplasia (UDH). It increases the risk of breast cancer only slightly, 1.5 times. If, on the other hand, some of the cells are changed, for example in their shape and structure, doctors call this atypical ductal hyperplasia (ADH). Her breast cancer risk is around four times higher.
The risk of flat epithelial atypia (FEA) is slightly higher. It often only affects a single cell layer, namely certain cells of the "milk duct walls" (epithelial cells). The FEA is closely linked to the ADH and is considered an early form of the DCIS.
Possible precancerous stage: DCIS
The so-called ductal carcinoma in situ (DCIS) is considered to be a possible preliminary stage of breast cancer. The cells that line the milk ducts (epithelial cells) are pathologically changed. However, they remain in the milk ducts (ductal), “in place” (in situ). As soon as these cells invade the surrounding mammary gland tissue, "real" breast cancer has developed from them. This happens to about four in ten women with DCIS that is not treated.
Even if a DCIS often remains harmless, it should always be treated to be on the safe side. Your doctor can tell you which treatment will make the most sense in your case.
You can read more about the diagnosis and treatment of this possible precancerous stage in the article DCIS - Ductal Carcinoma in Situ.
Breast cancer: different forms
Not all breast cancer is created equal. Doctors distinguish between different forms. The two most common are:
- Invasive breast cancer without a special type (IC-NST = no special type): Formerly known as invasive ductal breast cancer, the World Health Organization (WHO) has removed “ductal” from the current classification. Accordingly, these tumors show parts of milk ducts, but not enough to be considered purely invasive ductal breast cancer. Invasive breast cancer without a special type accounts for around 75 percent of all breast cancer diseases.
- Invasive lobular breast cancer (ILC): About 15 percent of all breast cancer tumors fall into this group. The cancer starts here from the glandular lobes.
There are also some rarer forms of breast cancer. These include, for example, inflammatory breast cancer (“inflammatory” breast cancer). This particularly aggressive breast cancer is associated with an inflammatory reaction in which the skin is reddened and swollen. It accounts for about one percent of all breast cancer diseases.
Where breast cancer develops
Doctors divide the chest into four quadrants (15 minute steps, analogous to the face of a clock). In this way, it is possible to more precisely specify where the tumor is growing:
- About half of all breast cancers develop in the upper outer quadrant.
- About 15 percent of malignant breast tumors grow in the upper inner quadrant.
- About eleven percent of breast cancers form in the lower outer quadrant.
- In about six percent of patients, the cancer tumor is located in the lower inner quadrant.
- In about 17 percent of cases, breast cancer develops on or under the nipple (retromamillary breast cancer).
Breast cancer in men
Rare, but possible: men can also develop breast cancer. Those affected are on average 70 years old. As in women, important risk factors are a genetic predisposition and an unfavorable lifestyle (obesity, lack of exercise, smoking, high alcohol consumption).
Men who had undescended testicles or some other form of testicular dislocation (cryptorchidism) as a child are also more susceptible to breast cancer. A previous inflammation of the testicles (orchitis) or inflammation of the epididymis (epididymitis) also increases the risk of male breast cancer.
You can find out more about the development of breast cancer in men, the symptoms as well as diagnosis and treatment in the article Breast cancer in men.
Breast cancer: symptoms
Signs of breast cancer include lumps and hardening in the breast tissue and watery or bloody secretions from the nipple. Breast cancer can also be the cause if a nipple or part of the breast skin pulls inwards. There are sometimes relatively harmless causes behind such changes. However, always have the complaints clarified by a doctor.
How do you recognize breast cancer?
As a woman, you should carefully palpate your chest once a month to detect any changes early. If breast cancer is actually behind it, treating the tumor quickly can improve the chances of recovery.
The best time to do a breast self-exam for women before menopause is one week after their menstrual period has started. Then the breast tissue is particularly soft, so that changes (such as lumps or hardening) can be identified more easily.
Supplement the monthly breast self-examination with regular early diagnosis examinations at the gynecologist. The statutory health insurances in Germany pay women over 30 years of age for a medical examination of the breast once a year. Women in Austria are generally entitled to an annual gynecological check-up from the age of 18. The basic insurance of the health insurance company in Switzerland takes over the examination at least every three years.
You can find out more about screening and early detection in the article Breast cancer screening.
Important signs of breast cancer
But what are the possible signs of breast cancer for which it is best to see your gynecologist as soon as possible? The main symptoms are
- New lumps or indurations in the chest (usually in the upper outer quadrant) or armpit
- changed size or shape of a breast
- Differences in the movement of the two breasts when raising the arms
- Retracted breast skin or nipple
- Changes in the color or tenderness of the skin of the breast, areola, or nipple
- watery or bloody secretions from a nipple
- enlarged lymph nodes in the armpit
- New, permanent reddening or flaking of the skin on the chest
Don't be alarmed if you discover one or more of these symptoms! Often there are relatively harmless causes behind it.
For example, if the lymph glands in your armpit are enlarged, the cause may be an infection. If a pressure-sensitive lump in the breast tissue can be felt, it is often just a benign tumor, a harmless cyst or compacted connective tissue.
Nevertheless, you should go to the gynecologist immediately in order to find out quickly. If the cause of your symptoms is harmless, you can rest assured. However, if the symptoms are actually breast cancer, early detection and treatment of the tumor can significantly improve your chances of recovery!
Does breast cancer cause pain?
Pain is an important alarm signal for many diseases - but not for breast cancer, at least not in the early stages. In the case of advanced breast cancer, however, daughter settlements (metastases) can trigger pain, for example bone metastases.
-
"Take your time!"
Three questions for
Prof. Dr. med. Michael Braun,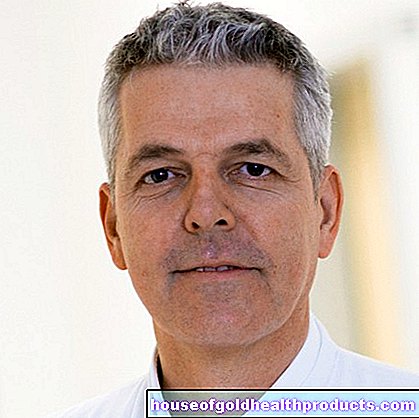
Gynecological and Obstetric Specialist -
1
How safe are mammography findings?
Prof. Dr. med. Michael Braun
In breast cancer screening in Germany, just under four percent of the findings are false positive - so raise the false alarm. However, screening usually reveals tumors that are still small and have not spread. In the majority of women affected by this, chemotherapy is then not necessary and no extensive lymph node removal has to be performed. Overall, screening can lower breast cancer mortality.
-
2
I was discovered breast cancer. Do you have to operate immediately?
Prof. Dr. med. Michael Braun
Breast cancer is usually very treatable! Take your time, visit a certified breast cancer center and seek advice. An operation is always part of the treatment. If chemotherapy is necessary, it is usually done before the operation. This allows you to see how the tumor is responding to it. If he has gotten smaller, you know that the therapy is working. If it has not disappeared, you can follow up with further therapy.
-
3
Can I still have children later and also breastfeed them?
Prof. Dr. med. Michael Braun
In principle, it is possible to have children after developing breast cancer. However, anti-hormonal therapy is often necessary for 5 to 10 years after treatment. If you want to have children, this must be interrupted - your doctor will advise you. Breastfeeding is possible with a healthy breast. In the case of the diseased breast, depending on the extent of the operation and the effects of radiation therapy, less milk is produced or breastfeeding is painful.
-
Prof. Dr. med. Michael Braun,
Gynecological and Obstetric SpecialistAs chief physician, Prof. Braun heads the senology department at the Rotkreuzklinkum Munich and heads the interdisciplinary breast center there. His focus is on gynecological oncology and special surgical gynecology.
Breast cancer: causes and risk factors
As with many other cancers, the root cause of breast cancer is not known. However, it is known that a number of risk factors promote breast cancer:
Female gender risk factor
About 99 percent of all breast cancer patients are female. Men very rarely develop breast cancer.
Age as a risk factor
According to statistics, the risk of breast cancer in women increases with age and decreases again slightly from the age of 75:
- 35 - 45 years: approx. 0.9 percent of women get sick
- 45 - 55 years: approx. 2.1 percent of women fall ill
- 55 - 65 years: approx. 3.2 percent of women fall ill
- 65 - 75 years: approx. 3.7 percent of women fall ill
- over 75 years: approx. 3.2 percent of women fall ill
Risk factor hormones
Breast cancer mostly grows dependent on female sex hormones. Various hormonal factors therefore influence the risk of breast cancer:
The longer a woman is exposed to cyclical fluctuations in estrogen and progesterone levels each month, the higher the risk of breast cancer. Women who had their first menstrual period very early (<11 years) and who entered menopause very late (> 54 years) are particularly at risk.
Pregnancy and breastfeeding also affect the risk of breast cancer. It decreases the more often a woman is pregnant and the longer she breastfeeds. A late first pregnancy, on the other hand, is a risk factor: If women do not have their first child until after the age of 30, the risk of breast cancer is slightly higher than for women who become mothers for the first time at a young age.
The importance of hormones for tumor development is also evident when taking artificial hormones: The “pill” can slightly increase the risk of breast cancer. Women who have been taking the pill for at least four years before they have a child and women who have been using the pill for several years before the age of 20 are particularly affected.
The risk of breast cancer increases more when taking hormone replacement preparations for menopausal symptoms. This is especially true if these preparations are taken for more than five years and contain both estrogens and progestin.
Experts advise against taking plant hormones (such as phytoestrogens) in isolation and in high doses as dietary supplements (for example for menopausal symptoms). They may also increase the risk of breast cancer.
Risk factors overweight and sedentary lifestyle
Obesity is another important risk factor for breast cancer. This also has to do with hormones: In adipose tissue, hormones are produced that raise the level of estrogen. Especially after menopause, being overweight seems to increase the risk of breast cancer - especially the risk of so-called estrogen-dependent tumors.
Sedentary lifestyle also has a negative impact on breast cancer risk.
Diet as a risk factor
A high-fat diet is bad for your health in several ways: for example, it makes you more susceptible to cardiovascular diseases (e.g. heart attack, stroke) and diabetes (diabetes mellitus). In addition, the estrogen level increases if you eat plenty of animal fats (sausage, fatty meat, butter, etc.). This increase in the female sex hormone increases the risk of breast cancer.
Risk factors smoking and alcohol
Smoking and secondhand smoke are harmful to health in several ways. Among other things, they promote the development of malignant tumors such as lung cancer and breast cancer. Girls who start smoking as teenagers, in particular, are at increased risk of developing a malignant tumor in the breast.
Alcohol is also a risk factor: the more often and the more alcohol you drink, the more likely you are to develop breast cancer!
Genetic predisposition as a risk factor
About 30 percent of patients have other breast cancer cases in the family. This can indicate a genetic cause. However, a disease-causing gene can only be found in 5 to 10 out of 100 patients. Hereditary breast cancer is therefore rather rare.
Two genes in particular have been well researched. They are referred to as BRCA 1 and BRCA 2. We also know a few other breast cancer genes that are likely to have less of an impact. But we don't know for sure yet.
Read more about genetic risk factors for breast cancer in the article Breast cancer genes BRCA 1 and BRCA 2.
If you have breast cancer in your family, you may want to have a genetic test. Ask your doctor whether this makes sense in your case.
Dense breast tissue risk factor
Some women have very dense breast tissue - that is, less fatty tissue and more glandular and connective tissue. This increases your risk of breast cancer five times. The reason: the more mammary gland tissue there is, the more cells there are that can degenerate.
Mammography can be used to determine how dense the breast tissue is. Doctors differentiate between four degrees of density:
- Density grade I: fat-transparent, well-transparent breast tissue
- Density grade II: moderately transparent breast tissue
- Degree of density III: dense breast tissue
- Density grade IV: extremely dense breast tissue
The density of breast tissue depends on various factors. It increases during hormone replacement therapy and decreases during pregnancy.
Risk factor ionizing radiation
Anyone who received radiation in the chest area as a child or adolescent has a slightly increased risk of breast cancer. Such radiation therapy is necessary for Hodgkin's lymphoma, for example. It's a form of lymphatic cancer.
Other forms of ionizing radiation, such as radioactive rays and X-rays, can also cause breast cancer and other forms of cancer. Breast tissue is considered to be particularly sensitive to radiation, especially before and during puberty and before the first full pregnancy. With age, breast tissue is less sensitive to ionizing radiation.
Breast cancer: examinations and diagnosis
If you notice a breast lump or other symptoms of breast cancer (such as skin retraction or leakage of fluid from the nipple), see a gynecologist immediately. He will first ask you a few questions about your medical history (anamnesis). This will help him to get to the bottom of the cause of your complaints. For example, the doctor will ask when you discovered the symptoms, whether you are taking hormones, and whether there are any cases of breast cancer or other cancers in your family.
Palpation examination of the chest
Then the doctor will palpate your chest and surrounding areas (such as armpits, collarbone). You can either sit or stand. As instructed by your doctor, either extend your arms up or put them on your hips. When palpating, the doctor pays attention to swelling, redness, retractions and changes in the shape of the breast and nipple. He also presses gently on the nipples. In this way he can determine whether secretion is leaking.
Ultrasonic
As part of an ultrasound examination (sonography) of the breast, the doctor examines the breast tissue itself and the area up to and in the armpit. With the help of the ultrasound, he recognizes the tissue under the skin and can thus assess any changes more precisely. You can read more about this in our article Breast ultrasound.
Mammography
With mammography, the preliminary stages and early stages of breast cancer can be identified even better than with ultrasound. However, the X-rays damage the tissue, especially in young women, as their cells divide more quickly and therefore more cells are irradiated. In young patients, the doctor therefore only carries out the X-ray examination if the benefits outweigh the risks.
For women between 50 and 69 years of age (Germany and Switzerland) or between 45 and 69 years of age (Austria), however, doctors even perform mammography routinely. The risk of breast cancer is particularly high in this age group. Every two years women of this age can have a mammography (mammography screening) at the expense of the statutory health insurance. Experts recommend this regular examination even if there is no specific suspicion of cancer. In younger women, mammography is only ordered if there is a specific suspicion of breast cancer.
You can read more about the procedure, significance and risks of chest x-rays in the article Mammography.
biopsy
Not every tissue change in the breast is malignant. By taking a tissue sample (biopsy), the doctor can determine whether it is actually cancer. Doctors can also determine the exact form of breast cancer in this way. Among other things, it is important to know how much the cells have already changed and whether they have many binding sites for hormones (i.e. need hormones to multiply). Only with this information can the doctor treat breast cancer in the best possible way.
The doctor usually removes the tissue on an outpatient basis, i.e. without a long hospital stay. You can read more about the process in our article "Biopsy: Breast".
Magnetic resonance imaging (MRI)
In some cases, the doctor will also perform magnetic resonance imaging (MRI). In order to be able to better delimit tissue changes, he usually also administers contrast media (contrast medium MRI). This gives him very detailed images of your breast tissue, on which even the smallest changes can be seen. However, this examination is only necessary if
- Ultrasound and / or mammography were not informative
- the doctor cannot remove any tissue, e.g. because the tumor is unfavorably located or several tissue sites are suspect
- the patient has breast implants
- the patient has close relatives with breast cancer or has BCRA gene changes
Investigations in confirmed breast cancer
If it is established that the patient has breast cancer, further examinations will follow. They should show whether and how far the cancer has spread in the body. For example, an X-ray examination of the chest (chest X-ray) can detect daughter tumors in the lungs (lung metastases). Settlements in the liver can often be detected using ultrasound.
A nuclear medicine examination of the bones (bone scintigraphy) can show whether cancer cells have settled in the skeleton. Computed tomography (CT) with contrast agent can also be helpful in looking for metastases. For patients with a high risk of relapse or metastasis, the currently valid guidelines recommend a computed tomographic examination of the thorax and abdomen.
The pathological finding
On the basis of the various examination results, the doctor creates a so-called pathological finding. It records the characteristics of breast cancer, mostly in the form of abbreviations.
For example, the TNM designation indicates
- how big the tumor is (T1 to T4),
- whether neighboring (regional) lymph nodes are affected (N0 to N3) and
- whether the breast cancer has already formed (distant) metastases in other parts of the body (yes = M1, no = M0).
An example: T4 N3 M0 describes a large tumor that has invaded the surrounding tissue (T4), cancer cells spread in many lymph nodes in the armpit and / or clavicle (N3), but has not yet formed any distant metastases (M0).
Further abbreviations in front of the TNM designation provide additional information. For example, a preceding “c” means that the doctor has classified the cancer on the basis of clinical examinations (for example imaging procedures, biopsy). With a preceding “p”, the TNM designation is based on tissue (histopathological) laboratory results that were carried out after an operation.
Grading - the degree of degeneration of the tumor - is also important for the classification of breast cancer stages. It indicates how much the tissue has changed. It comprises four stages: from G1 (cells little changed, tumor usually grows slowly and not very aggressively) to G4 (cells strongly changed, tumor usually grows quickly and tends to grow aggressively into the surrounding tissue).
The pathological findings also indicate the hormone receptor status of the tumor. It indicates whether the patient's breast cancer has many docking points for estrogen (ER + or ER-positive) and / or progesterone (PgR + or PgR-positive). Often both are stated together as hormone receptor positive (HR + or Hr-pos.). This is important for therapy planning: A tumor with many hormone receptors grows through hormones. If you withdraw these hormones from him, it slows down his growth.
The HER2 receptor status indicates whether the tumor cells have many docking sites for growth factors (HER2 / neu receptors, also ERBB2 or erbB2) on their surface. If so (HER2-positive), the disease usually takes a more aggressive course. Blocking the docking sites can prevent the breast cancer from growing.
Unsuitable for diagnosis: tumor markers
As previously hoped, breast cancer cannot be diagnosed using tumor markers in the blood. Tumor markers are proteins whose concentration in the blood or tissue can be increased in cancer - either because they are produced by the tumor itself or by healthy cells in response to the tumor.
However, other diseases can also increase the concentration of such tumor markers. Therefore, they are usually not suitable for diagnosing cancer. With their help, however, one can assess the progression of cancer and the success of the therapy.This also applies to breast cancer: the most important tumor marker in breast cancer is CA 15-3; CEA also plays a role. The doctor regularly measures both tumor markers in breast cancer patients to check how the tumor is developing and how well the treatment is working.
Breast cancer: treatment
If you have breast cancer, the doctor treating you will give you an individual treatment plan. It depends on which breast cancer is present and how far advanced it is. The properties of the cancer cells are also decisive - for example, whether they have receptors for hormones and / or growth factors on their surface. In addition, the doctors take into account your age, your general health and your hormonal status (i.e. whether you are going through menopause or not) when planning therapy.
The therapy plan usually consists of several components: The doctors combine the treatment methods that promise the best chance of success in your case. In principle, the following treatment options are available for breast cancer: surgery, chemotherapy, radiation, (anti) hormone therapy and targeted therapies such as antibody therapy.
Depending on the type and stage of cancer, doctors recommend a certain therapeutic approach that, according to numerous studies, promises the best possible success. The attending physician will explain this to you in detail. Speak openly about your concerns and wishes.
Adjuvant, neoadjuvant, palliative
Breast cancer surgery is performed on almost all patients. Usually another therapy method follows the procedure in order to improve the success of the treatment. Doctors refer to this as "adjuvant". For example, many patients receive adjuvant chemotherapy or radiation therapy.
Sometimes the doctor will perform chemotherapy or radiation before the tumor is surgically removed. The aim is to reduce the size of the tumor before the procedure. In this case, doctors speak of neoadjuvant treatment.
Chemotherapy and the like can also be used palliatively: In some cases, breast cancer has progressed so far that a cure is no longer possible. Then palliative treatment can at least slow down tumor growth and alleviate the symptoms.
Breast cancer: surgery
Doctors almost always remove breast cancer surgically. Whenever possible, he chooses breast-conserving therapy (BET). In some cases, however, the entire breast must be amputated (mastectomy). The breast can then be reconstructed.
Breast-conserving therapy (BET)
With breast-conserving therapy, the doctor removes the tumor while the breast itself is (largely) preserved. This is possible with many patients. However, certain requirements must be met. For example, doctors can only operate breast-conserving surgery if the tumor is localized. In addition, it must not be too large in relation to the breast and not grow multicentrically (i.e. not consist of several foci in different quadrants of the breast).
Together with the cancerous tumor, the doctor removes a margin from healthy tissue. He wants to make sure that no marginal cancer cells remain in the body. He also cuts out the immediately neighboring lymph nodes (sentinel nodes). During the procedure, he examines them under the microscope to check whether they are already infected with cancer cells. If so, he will also have to cut out lymph nodes from the armpit.
A breast-conserving operation is usually followed by radiation therapy (adjuvant radiation).
Mastectomy
In some breast cancer patients, the tumor is too large for breast-conserving surgery. Then the whole breast has to be removed. Doctors call this procedure a mastectomy. It may also be necessary for other reasons, for example if the tumor consists of several cancer foci in different quadrants of the breast (multicenter breast cancer). Doctors also remove the entire breast for inflammatory breast cancer.
There are different types of mastectomy. In the past, the breast muscles were removed along with all of the breast tissue, the overlying skin and the nipple. Today doctors usually use gentler techniques that preserve the pectoral muscle. Sometimes they even leave the breast skin and nipple in place.
You can read more about the procedure and risks of a mastectomy in the article Mastectomy.
The doctor discusses the most suitable OP variant with the patient in advance. By the way: In the early stages of breast cancer, breast-conserving therapy with subsequent radiation has just as good a prognosis as a complete mastectomy.
Breast augmentation
Breast amputation is often followed by breast reconstruction. The removed breast is rebuilt with an implant made of plastic or with your own tissue. Breast augmentation can also be useful after breast-conserving surgery if the surgeon had to cut a lot of tissue out of the breast to remove the tumor.
In both cases, the following applies: Breast augmentation after breast cancer surgery is not cosmetic surgery out of vanity. Especially after a mastectomy, many women feel "incomplete" and less feminine than before. Breast-conserving surgery can also be psychologically stressful, for example if the breasts look different afterwards. Breast reconstruction can help those affected to feel good again in their bodies. This is important for the healing process!
There are also medical reasons for breast augmentation. Some patients have back pain and poor posture after breast removal, which can permanently damage the bones (postural damage). So don't be afraid to seek detailed advice from your doctor on the options for breast reconstruction!
You can read more about the topic of breast reconstruction in the article Breast augmentation.
Breast prostheses
Alternatively, the lack of a breast can be concealed with a breast prosthesis (breast epithesis). Different models are available:
The simplest variant is an insert made of foam or silicone, for example. It is pushed into the bra to visually replace the missing breast. In medical supply stores you can get special prosthetic bras with integrated pockets for the insoles. Special swimsuits and bikinis with such pockets are also available.
Another variant are self-adhesive prostheses. They are worn directly on the skin. Women should only wear such adhesive prostheses once the surgical scar has healed completely and radiation therapy has been completed.
Breast cancer: radiation
After breast-conserving surgery and sometimes also after a mastectomy, patients usually receive (adjuvant) radiation therapy: Breast cancer residues that may have remained in the body are so badly damaged by the high-energy radiation that they die.
The doctor usually irradiates the entire breast. He often also irradiates the lymph nodes under the collarbone and in the armpit. Only in older patients or when the risk of relapse is very low, does he limit the radiation to the part of the breast where the tumor was (partial breast radiation).
Breast cancer patients should start radiation therapy as soon as possible - as soon as the surgical wound has completely healed. The radiation usually takes place several days a week. How long it lasts and what radiation dose the doctor uses varies from patient to patient.
In certain cases, neoadjuvant radiation therapy is also useful - i.e. irradiating the tumor before the operation. This is supposed to shrink the breast cancer focus so that surgeons can eventually remove it more easily. If breast cancer cannot be operated on or if the patient refuses the operation, the doctor may give radiation therapy on its own.
Side effects of breast cancer radiation
Nowadays it is possible to direct the rays very specifically only to the desired tissue area and thus largely to spare healthy cells or organs. Nevertheless, side effects cannot be completely ruled out. The skin in the irradiated area is very stressed. As with severe sunburn, it can react with painful redness and even blistering. Hair loss can also occur. When lymph nodes are irradiated, lymph fluid can accumulate in the chest or arm (lymphedema).
Lymphedema in breast cancer can be a direct consequence of the tumor and can also occur after an operation and / or radiation.
Breast cancer: chemotherapy
The doctor very often uses chemotherapy for breast cancer. The patients receive so-called cytostatics (usually as an infusion, sometimes also as a tablet): The active ingredients are distributed in the body and reach even the smallest, previously undiscovered tumor nests and individual cancer cells in the blood and lymphatic system. These are so damaged by the cytostatics that they die.
Chemotherapy can be performed before (neoadjuvant) or after surgery (adjuvant). Doctors also use them as palliative therapy: If breast cancer is incurable, the cytostatics can at least slow down tumor growth.
Chemotherapy: multiple cycles
Usually the patient receives various cytostatics in several cycles. The doctor individually determines which drugs these are and how many. There is a short break between the individual cycles in order to keep the side effects of chemotherapy as low as possible.
Chemotherapy port
The doctor usually gives the cytostatics as an infusion. So that he does not have to prick the patient's vein before each treatment cycle, he can insert a port under the skin (usually below the collarbone). This is a small metal or plastic chamber with a tube (catheter) that leads into a large vein near the heart. The doctor uses a special needle to administer the cytostatics through the port into the vein.
The port can remain in the body for a long time (even a few years). The patient is not restricted in her movement by the implanted small chamber and may - in consultation with the doctor - also bathe, shower or do sports.
Chemotherapy side effects
Cytostatics cannot differentiate between healthy and cancerous cells. Therefore, the treatment can have undesirable effects. Cells that divide quickly are particularly damaged. In addition to cancer cells, these include, for example, the blood-forming cells in the bone marrow. As a result, patients sometimes have too few red and white blood cells and platelets. They suffer from anemia, their blood clotting is impaired and they are more prone to infections.
Chemotherapy also often damages the hair root cells, causing hair loss. Other common side effects are nausea and vomiting, diarrhea, loss of appetite, and persistent exhaustion and tiredness.
You can read more about the undesirable effects of cytostatics in the article Chemotherapy: Side Effects.
Breast cancer: anti-hormone therapy
About two thirds of all breast cancers have many estrogen and / or progesterone receptors. They therefore grow through the female sex hormones. For such tumors, (anti) hormone therapy (endocrine therapy) comes into question: The patients receive drugs that stop or at least slow down the hormone-dependent tumor growth. Depending on the exact mechanism of action, these are anti-estrogens, aromatase inhibitors or GnRH analogues.
(Anti-) hormone therapy for breast cancer extends over several years. Possible side effects of treatment include menopausal symptoms such as hot flashes and mood swings. They can also occur in patients who have already passed their menopause.
Antiestrogens
Anti-estrogens inhibit the effect of the female sex hormone estrogen by occupying its binding sites on cancer cells and inhibiting estrogen-dependent processes in the cell.
The main anti-estrogen drug in breast tissue is tamoxifen. It is suitable for patients before and after the menopause and is taken as a tablet once a day. Since it only works against estrogen in breast cells, but works exactly like estrogen in the uterine lining, doctors call tamoxifen a selective estrogen receptor modulator (SERM). The effects of the drug therefore depend on the type of cell in question.
A preparation that always counteracts estrogens is fulvestrant. It is therefore considered an actual anti-estrogen. It also reduces the number of estrogen receptors. Doctors primarily prescribe fulvestrant for advanced or metastatic breast cancer.
Aromatase inhibitors
Aromatase inhibitors block the body's own production of estrogen in muscle and fat tissue, but not those in the ovaries. They are therefore only suitable for postmenopausal patients (when the ovaries have already stopped producing hormones). Aromatase inhibitors are taken as a tablet once a day. Well-known aromatase inhibitors are anastrozole, letrozole and exemestane.
GnRH analogues
GnRH analogues (such as buserelin or goserelin) are artificial hormones that inhibit the production of estrogen in the ovaries. They are therefore suitable for the treatment of breast cancer before menopause. The patients are "artificially put into menopause" by the GnRH analogues. The medication is injected under the skin every few weeks or months.
The different groups of active substances in (anti) hormone therapy can also be combined with one another. Doctors usually administer GnRH analogues together with tamoxifen or aromatase inhibitors.
Doctors also often use GnRH analogues on patients of childbearing potential before starting chemotherapy. This can help ensure that the person concerned is still able to reproduce after therapy. Cytostatics can also make you sterile. Consult your doctor in detail about this.
Breast Cancer: Targeted Therapies
Targeted therapies specifically block processes in cancer cells that are important for tumor growth. The drugs attack certain target structures in the cancer cells. Targeted therapy is only possible if the cells have such a target structure (which is not always the case). Usually the doctor only uses these therapies in advanced breast cancer, in addition to other methods (such as chemotherapy). The following are some examples of targeted drugs approved for breast cancer treatment:
HER2 antibodies
One of the targeted therapies against breast cancer is antibody therapy (immunotherapy) with HER2 antibodies (trastuzumab, pertuzumab): some breast carcinomas have a large number of docking points for growth factors, so-called HER2 receptors (HER2 / neu receptors) on their surface. These tumors grow particularly aggressively. In the past, it was therefore often not so easy to help affected women. That changed with the introduction of HER2 antibody therapy: HER2 antibodies block the receptors so that growth factors can no longer dock - cancer growth is slowed down or blocked.
The HER2 antibody trastuzumab is already approved for the early stages of breast cancer, but can also be used for advanced and metastatic breast cancer. The doctor gives trastuzumab as an infusion before or after the surgical removal of the tumor (neoadjuvant or adjuvant).
Sometimes the doctor will give another HER2 antibody called pertuzumab along with trastuzumab. It works in a similar way, but binds in a different place than trastuzumab. The combination of both antibodies together with chemotherapy can therefore be particularly effective.
Tyrosine kinase inhibitors
A tumor needs certain enzymes to grow. These include the so-called tyrosine kinases. They can be blocked with tyrosine kinase inhibitors. Lapatinib belongs to this group of drugs. It blocks the corresponding tyrosine kinase site on the growth receptors EGFR and HER2. Therefore, doctors only give it to HER2-positive breast cancer. The active ingredient is taken as a tablet. Doctors use it for advanced breast cancer, often in addition to chemotherapy, hormone or antibody therapy, and usually only after other therapies have already taken place.
Angiogenesis inhibitors
If the tumor exceeds a certain size, it needs more oxygen and nutrients - the existing blood vessels are no longer sufficient for it. The tumor itself then stimulates the formation of new blood vessels (angiogenesis). With so-called angiogenesis inhibitors, the formation of new vessels can be prevented - the tumor "starves". An example of an angiogenesis inhibitor is the active ingredient bevacizumab. It is sometimes given as an infusion to patients with advanced breast cancer, in addition to chemotherapy.
Bone-Targeting Therapy
Many of the drugs used in chemotherapy and anti-hormone therapy damage the bones. They break down bone substance and make it unstable and fragile (osteoporosis). To avoid this, the doctor sometimes uses bone-directed therapy.Bisphosphonates such as alendronate prevent bone loss and strengthen the remaining bone mass. Patients usually receive it as a tablet. An alternative is the denosumab antibody.
Doctors also use these drugs for bone metastases from breast cancer.
Breast cancer: further therapeutic measures
In addition to breast cancer therapy with surgery, chemotherapy, etc., other measures can help. Some of them are used to prevent or alleviate side effects of the therapy. For example, chemotherapy often triggers nausea and vomiting. Special medications, so-called anti-emetics (anti-emetics), help against this. They are usually given immediately before and during chemotherapy. This means that in many cases there is no longer any vomiting, which was more common in the past and which many sufferers still fear.
Acupuncture can also relieve nausea and vomiting. The targeted placement of the needles is also often recommended against the persistent exhaustion and tiredness (fatigue) in cancer patients.
In addition, yoga can help against stress, anxiety, depression and exhaustion (fatigue) and improve the quality of life for cancer patients.
It is also important to do sports and exercise. If you are unsure how much your body can handle, ask your doctor for advice.
Medicinal plants for breast cancer
Some patients support breast cancer therapy with medicinal plants. This only makes sense in some cases. Some examples:
When patients feel bloated, fennel tea can help. Black cohosh extracts can relieve hot flashes that occur, for example, as a result of anti-hormone therapy. However, so far nothing is known about possible side effects or interactions with cancer therapy.
Mistletoe extracts are said to help with breast cancer (and other forms of cancer) in several ways: They are supposed to work against the tumor, prevent relapse and improve the tolerance of chemotherapy. So far, however, it has not been possible to prove these effects with certainty. Some patients also have an allergic reaction to the herbal preparation, which is usually injected under the skin. In addition, it is not clear whether mistletoe extracts influence ongoing tumor therapy.
If you plan to use medicinal herbs during your breast cancer treatment, discuss this with your doctor first. He can inform you about possible side effects or interactions.
Alternative healing methods alone are not enough for cancer to successfully combat the malignant disease. However, you can support conventional medical treatment.
Diet in breast cancer
As long as the breast cancer has not progressed, it does not directly affect the patient's metabolism. As a rule, no special diet is then necessary. Just like healthy people, breast cancer patients should eat a balanced diet. Then vitamin preparations and food supplements are also unnecessary.
In addition, women with breast cancer should make sure that their bodies are supplying exactly as much energy as it needs - no more and no less: Being very overweight in breast cancer is associated with a higher risk of relapse and death. Underweight, which occurs particularly in advanced breast cancer, is also problematic. Underweight patients usually do not tolerate cancer therapy as well.
Therapies not recommended
Various therapy tips for breast cancer are circulating in books, the Internet and word of mouth, which experts advise against - because they are of no use and can sometimes even have negative effects. Some examples:
- Oxygen and ozone therapy are not recommended because they can have an adverse effect.
- The effects of zinc, magnesium or iodine supplements are not yet fully understood and could also be detrimental. Zinc in particular does poorly in laboratory experiments. In the case of iodine, there is also evidence of a positive effect.
- High-dose preparations with vitamins A, C and E (beta-carotene) are also not recommended. They may weaken the effects of radiation therapy or chemotherapy.
- If you have hormone-sensitive breast cancer, you should not take high-dose substances with (potentially) hormonal effects. These include, for example, drugs for hormone replacement therapy for menopausal symptoms, phytoestrogens (such as in soy, red clover, Chinese angelica, sage) as well as milk thistle, ginseng and hop preparations. You can weaken anti-hormone therapy.
- Avoid St. John's wort during anti-hormone therapy, chemotherapy, or antibody therapy for breast cancer as it could weaken the therapeutic effect.
- Do not take folic acid supplements if you are receiving chemotherapy containing the active substance 5-fluorouracil. Otherwise, chemotherapy can have a much more damaging effect on cells.
Get a second opinion!
Are you unsure about the proposed therapy plan? Then don't be afraid to tell your doctor that. If he cannot resolve your concerns, you have the right to a second medical opinion from an independent expert. Health insurance companies and cancer counseling centers will help you find a suitable specialist.
You will then need a referral for this second expert and must provide him with all the documents that led to the initial diagnosis (laboratory results, x-rays, etc.) as well as a summary of the diagnosis and the planned measures. The first treating doctor is obliged to provide these documents or copies of them.
The second specialist examines these documents and usually asks you for a personal interview in order to be able to assess your situation even better. The result may be that he confirms the proposed therapy. But he can also suggest some (minor) changes. If the first and second opinion differ significantly from each other, the two doctors should consult with each other and formulate a joint therapy recommendation so as not to further unsettle you as a patient.
The costs of a second opinion by another specialist are usually borne by the statutory health insurance companies. If you have private insurance, you can check your insurance contract to see whether such costs are covered. In any case, you should clarify the cost question with your health insurance company before obtaining a second opinion.
Breast cancer: metastases
In every fourth patient, the tumor forms daughter tumors (metastases) in other parts of the body in the course of the disease. Sometimes the metastases are already present at the time of diagnosis, but often they do not develop until later. In principle, metastases are more likely to develop
- when the cancer is discovered late
- with certain biological properties of cancer cells
- in the first few years of the disease, but metastases can still occur after a few years
How and where do breast cancer metastases develop?
Cancer cells can detach from the main tumor in the breast and are carried with the blood or lymph flow to other regions of the body, where they attach and form new growths (haematogenic and lymphogenic metastasis). The most common breast cancer metastases develop in the bones, liver and lungs. But sometimes they are also found in other organs such as the brain.
Bone metastases
Breast cancer can metastasize in the bones, especially in the spine, but sometimes in other bones such as the thighs and humerus, pelvis, ribs, sternum, or the roof of the skull. Affected people suffer from bone pain. In addition, affected bones can break more easily - medical professionals call such a cancer-related bone fracture a pathological fracture. Bone metastases can be detected by means of X-ray examinations, computed tomography (CT) and magnetic resonance imaging (MRI). The bone scintigraphy shows how extensive the bone involvement is.
Liver metastases
Breast cancer metastases in the liver often do not cause any symptoms for a long time. Sometimes they trigger nonspecific symptoms such as bloating and other digestive problems, poor appetite, and weight loss. If liver metastases are suspected, the doctor examines the abdomen using ultrasound. If the findings are unclear, computed tomography or magnetic resonance tomography can help.
Lung metastases
If, in advanced breast cancer, coughing and shortness of breath occur without an explanation (such as a respiratory infection), it can be caused by breast cancer metastases in the lungs. This suspicion can be clarified by the doctor X-raying the patient's chest (chest X-ray).
Brain metastases
Sometimes breast cancer metastasizes to the brain. Depending on the affected brain region, the result is a wide variety of symptoms. These can be headaches, perception disorders, impaired consciousness or speech, or even seizures. Brain metastases can be detected using computed tomography or magnetic resonance imaging.
Further examination for metastases
If possible, the doctor takes tissue samples from the metastases and has them analyzed in the laboratory. Sometimes metastases have different biological properties than the original tumor in the breast. It may be that the primary tumor (breast tumor) grows hormone-dependent, but the metastases do not. An (anti) hormone therapy then only works against the tumor in the breast, but does nothing against the metastases.
Sometimes metastases only appear some time after an initially successful breast cancer therapy. They then represent a relapse, medically called a relapse. New tissue samples are particularly important in such cases. In addition, the tumor markers can also be helpful: They fall off after successful treatment. If you increase again, this may indicate a renewed increase in breast cancer or metastases.
Treatment of breast cancer metastases
The doctor plans the therapy for breast cancer metastases individually for each patient. He also checks them again and again and adjusts them if necessary. The doctor usually treats metastases systemically - i.e. with drugs that work throughout the body and act against scattered cancer cells. As with breast cancer, these can be anti-hormonal drugs (anti-hormone therapy) or cytostatic drugs (chemotherapy). Sometimes he also uses targeted drugs (such as HER2 antibodies) against metastases.
In addition, women with bone metastases are often also given bisphosphonates. These active ingredients can ensure that the metastases do less damage to bone tissue. This makes the bone more stable and less prone to fractures.
The doctor surgically removes some metastases or irradiates them. Then he describes the treatment as local or regional.
Breast cancer metastases can cause great pain for those affected. You will then need adequate pain management. This mainly includes painkillers - the doctor will adjust the type and dosage individually. In addition, the pain can often be relieved with non-drug methods. This can be, for example, cold or heat applications (baths, packs, etc.) as well as relaxation methods such as autogenic training.
Breast cancer metastases: life expectancy and prognosis
When women are diagnosed with "metastatic breast cancer" it is often a big shock. Because the cancer can then usually no longer be completely cured. The individual prognosis depends on various factors, such as the exact type of breast cancer or the location of the metastases. In some cases, the condition worsens quite quickly. In other cases, women with the right treatment can survive for decades, even if the breast cancer has metastasized: The right therapy can stop further tumor growth and possibly suppress the cancer at least temporarily.
In principle, the exact course of breast cancer cannot be predicted. Information on the prognosis is based on statistics and empirical values, but does not have to apply to the individual concerned.
Breast cancer: aftercare and rehab
What happens after the initial therapy (surgery, chemotherapy, radiation therapy) has been completed? Many breast cancer patients are concerned with this question. Don't worry - you will not be left alone! As part of the aftercare, you will be looked after for a longer period of time. The doctor carries out regular follow-up examinations in order to detect any relapses at an early stage.
Rehabilitation is also important in breast cancer. It should make it easier for patients to return to everyday life.
Rehabilitation after breast cancer
Rehabilitation after breast cancer should help those affected to return to their everyday, social and, if necessary, professional life as easily as possible. It is also intended to prevent or alleviate the long-term effects and impairments (such as lymphedema) caused by the cancer and its treatment.
When selecting suitable rehabilitation measures, the needs and wishes of the patient play a major role. It is best to discuss the measures that make sense together with the patient and doctor. Possible offers are for example:
- Information and training on breast cancer and other health topics
- Sports and exercise therapies
- Nutritional advice and training
- Treatment of lymphedema
- Psychological counseling and therapies, relaxation procedures and artistic therapies to support coping with illness (such as music therapy), occupational therapy
- Advice on social and social law issues, assistance with applying for benefits or a severely disabled person's pass
- Measures to support professional and social integration, planning of medical aftercare and general further care
Specialized clinics, in which patients are accommodated as inpatients, offer several weeks of all-day rehabilitation programs. In some places there are also outpatient rehab offers in a day clinic.
The rehabilitation usually takes place immediately after the cancer treatment has been completed (follow-up rehabilitation, follow-up treatment). In some cases, if patients start this later, insurance companies will not pay for it. Sometimes follow-up rehabilitation is not possible immediately after the first treatment. You can start such a “cure” after breast cancer later, but you have to consult the responsible insurance company beforehand.
Breast cancer patients can still apply for some rehabilitation measures after they return home if problems arise in everyday life. This includes, for example, psycho-oncological advice, participation in a rehab sports group or nutritional advice. Patients should discuss this with their doctor in charge of follow-up care.
Advice and application
The patient must apply for rehab after breast cancer himself. The follow-up rehabilitation even has to be applied for before the end of the first treatment phase. Patients in the hospital can get help with the application from the clinic's social services. Breast cancer patients with statutory health insurance who would like to undergo outpatient rehab can seek advice from the rehab service centers (www.reha-servicestellen.de).
costs
The costs of rehabilitation for patients with statutory health insurance are covered by health insurance or pension insurance. However, patients usually have to make an additional payment. In some cases you can be exempted from paying the co-payment. Your insurance company will answer any questions you may have. Private insurance companies only cover the rehab costs if this has been agreed in the insurance contract.
Follow-up care after breast cancer
After the first breast cancer treatment is complete, follow-up care follows. Even after 20 years, breast cancer can relapse at the original location of the tumor (local recurrence) or lead to metastases. Consistent follow-up care is therefore very important. So can the doctor
- detect a relapse or tumor in the other breast early on
- Caring for patients on anti-hormone therapy, which usually lasts for several years
- Recognize and treat side effects of breast cancer therapy
- support and advise the patient psychologically
Women with advanced breast cancer (with metastases) are usually treated permanently. Psychosocial support and all measures that improve the quality of life are particularly important here.
What does a follow-up examination look like?
For follow-up examinations, patients can either go to a resident doctor (such as a gynecologist or oncologist = specialist in cancer) or to a specialized outpatient clinic.
The examination begins with a detailed discussion (anamnesis). The doctor asks the patient what her current state of health is and whether she is suffering from symptoms or therapy side effects. He then palpates the chest, armpits and the lymph nodes located there (physical examination).
He also does chest x-rays (mammograms) and ultrasound examinations at regular intervals. In high-risk patients (for example with genetic changes), the doctor usually also arranges an MRI of the breast.
If the physical or imaging examinations reveal any abnormalities, further examinations are necessary (such as blood tests, MRI, CT). If necessary, the doctor will refer the patient to other specialists (such as radiologists) or to a breast cancer center.
Follow-up visits: the schedule
Follow-up care begins as soon as the primary treatment (such as surgery, chemotherapy and / or radiation therapy) is completed. Your doctor will tell you how long and how often the follow-up examinations make sense in your case. Experts recommend the following schedule for asymptomatic patients:
- 1st to 3rd year: discussion and palpation examination every three months; Mammography and breast ultrasound once a year
- from the 4th year: every six months discussion and palpation examination; Mammography and breast ultrasound once a year.
- from the 6th year: early breast cancer detection (palpation, mammography and ultrasound of the breast once a year)
Breast cancer: disease course and prognosis
How breast cancer will progress in individual cases depends on various factors. One thing is certain: If a breast cancer is not treated (in time), it forms daughter settlements (metastases) in other parts of the body. Treatment is then more difficult and aggressive than in the early stages of breast cancer. In addition, as the tumor progresses, the chances of recovery decrease.
Breast Cancer: Chances of a Cure
Breast cancer can be cured in most women if it is recognized in time and treated correctly. Thanks to advances in treatment, the patient's chances of survival have improved. The prognosis in each individual case depends on several factors. In addition to the stage of breast cancer at diagnosis, this also includes the type of tumor. For example, inflammatory breast cancer grows more aggressively than other forms of breast cancer.
Other factors that influence the chances of recovery from breast cancer are, for example, the general health of the patient and her age. The prognosis for younger breast cancer patients is often less favorable than for older ones.
You can find out more about the prognosis for breast cancer in the article Breast Cancer: Chances of a Cure.
Prevent breast cancer
Some risk factors for breast cancer can be avoided or at least reduced. With this in mind, experts recommend the following preventive measures:
- Get regular exercise and exercise: Women who are physically active for 30 to 60 minutes at least five days a week have a 20 to 30 percent lower risk of breast cancer. This is especially true after menopause! The currently valid guidelines recommend at least two and a half hours of moderate exercise or 75 minutes of strenuous exercise per week. Patients should do strength training two days a week.
- Maintain a healthy weight.
- Eat less saturated fatty acids, such as those that contain fat sausage, meat, butter and other dairy products. On the other hand, watch out for polyunsaturated fatty acids (for example in fish or vegetable oils). Eat a balanced diet with lots of fruits, vegetables and fiber.
- In addition, you should not smoke and drink little or no alcohol.
- Only use hormone replacement therapy (HRT) for menopause if the menopausal symptoms (such as hot flashes) cannot be alleviated in other ways or are very stressful. Caution is also advised when using other hormone preparations (such as the pill or herbal hormones).
Especially if you have had breast cancer before, these tips can help you and reduce the risk of breast cancer relapse.
Tags: sports fitness hospital Diagnosis