TBE vaccination
and Martina Feichter, medical editor and biologistFabian Dupont is a freelance writer in the medical department. The human medicine specialist is already doing scientific work in Belgium, Spain, Rwanda, the USA, Great Britain, South Africa, New Zealand and Switzerland, among others. The focus of his doctoral thesis was tropical neurology, but his special interest is international public health and the comprehensible communication of medical facts.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
The TBE vaccination is the only safe protection against early summer meningoencephalitis (TBE). This is a tick-borne viral infection that can be very dangerous. That is why the TBE vaccination is recommended to all people in TBE risk areas. It can be administered by your family doctor or a travel doctor. Read everything you need to know about the TBE vaccination here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. Z24A84
What is the TBE vaccination?
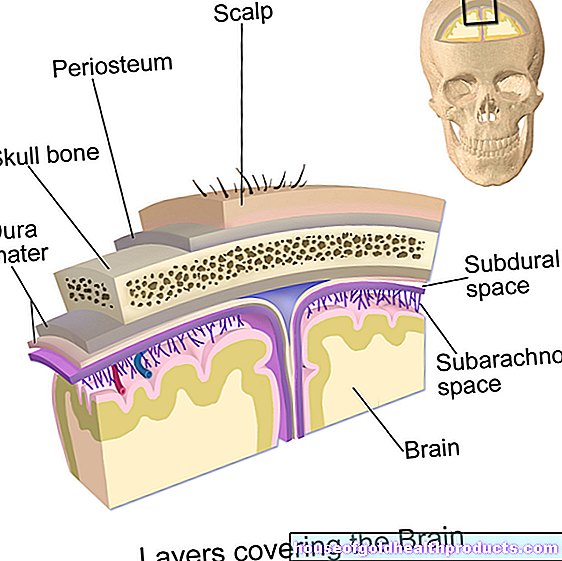
The TBE vaccination (colloquially: tick vaccination) is a vaccination against early summer meningoencephalitis. This tick-borne viral infection is rare, but it can have serious consequences: The viruses can cause inflammation of the meninges, brain and spinal cord. This can have long-lasting or even permanent neurological consequences such as paralysis. In rare cases, TBE can even lead to death.
A vaccination against TBE was developed for prevention. The vaccine is a so-called dead vaccine. It consists of inactivated TBE viruses. These can no longer trigger illness, but still activate the immune system: The white blood cells (defense cells of the body) remember the characteristic features of the TBE virus and develop specific antibodies against them. If a real infection with the TBE virus occurs later, the immune system is prepared: It immediately begins to produce large numbers of the specific TBE antibodies in order to eliminate the intruder before the disease can break out.
The TBE vaccination only prevents infection with TBE viruses - it does not offer any protection against other pathogens transmitted by ticks (such as borreliosis bacteria)!
Who should receive the TBE vaccination?
The TBE vaccination is recommended in Germany by the responsible authorities (Robert Koch Institute) for the following people:
- People who live in or travel to TBE risk areas: This also includes people who spend a lot of their free time in forest and meadow regions within TBE risk areas. If you plan to travel abroad, you should clarify in advance with a travel doctor whether there is a risk of infection in the target region.
- Professional groups who could come into contact with the TBE virus during their work: These include, for example, foresters, hunters, forest workers, agricultural workers and employees in medical laboratories.
TBE risk areas
In Germany, ticks in Bavaria, Baden-Württemberg, Hessen, Lower Saxony, Thuringia, Rhineland-Palatinate, Saarland and Saxony are mainly infected with the TBE virus - many regions in these federal states are designated as TBE risk areas. Infection can also occur in other federal states such as Brandenburg and North Rhine-Westphalia, albeit less often.
Other European countries in which TBE viruses are widespread are, for example, Austria, Switzerland, Hungary, the Czech Republic, Croatia, Poland, Sweden and Finland. In contrast, in Italy, France, Norway and Denmark, the risk of TBE transmission is very low.
You can find out more about the areas at home and abroad in which there is a risk of TBE infection in the article TBE areas.
How is the TBE vaccination administered?
Two TBE vaccines are currently approved in Germany: TBE-Immun® and Encepur®. In both cases, three vaccine doses are necessary for the primary vaccination. Thereafter, there is a high level of immune protection against TBE viruses. However, it should be refreshed at certain intervals (booster vaccinations).
The two available TBE vaccines are considered equivalent and interchangeable. Nevertheless, the same TBE vaccine should always be used for the primary vaccination and the booster vaccinations.
TBE basic immunization
The basic immunization for the TBE vaccination consists of three injections. The second dose should be given one to three months after the first. When the third dose is recommended depends on the TBE vaccine used: With TBE-Immun®, the third dose should be administered five to twelve months after the second. With Encepur®, the third dose is recommended nine to twelve months after the second dose.
In addition to this standard vaccination schedule, there is also a quick vaccination schedule (e.g. for trips to a TBE risk area planned at short notice). It looks like this:
- FSME-Immun®: The second vaccination dose is given 14 days after the first. The third dose (as with the standard schedule) should be given five to twelve months after the second injection.
- Encepur®: The second dose is given 7 days after the first, the third dose 14 days after the second.
TBE vaccination: refresher
The immune protection that is acquired with full basic immunization lasts for at least three years. For longer protection, it should be refreshed at certain intervals depending on the TBE vaccine:
With TBE-Immun®, the first booster vaccination is due three years after the basic vaccination - regardless of whether it was administered according to the standard or the rapid vaccination schedule. The further TBE refresher tests should then take place every five years for people between 16 and under 60 years of age. People who are 60 years or older should have the TBE booster done every three years.
With Encepur®, the first booster vaccination should be given three years after the primary vaccination, if this was administered according to the standard schedule. Anyone who was vaccinated against TBE in the rapid vaccination scheme should have their immune protection refreshed for the first time 12 to 18 months later. In both cases, the same recommendations apply to further booster vaccinations: People between the ages of 12 and 49 should have the TBE vaccination boosted every five years. For people aged 50 and over, TBE refreshment is advisable every three years.
TBE vaccination: children
In children, meningoencephalitis in early summer usually heals without any consequences. Nevertheless, vaccination protection is important for them: Children play a lot outdoors - in forests and meadows - and are therefore more likely to be bitten by ticks. The likelihood of a TBE infection is therefore higher in them than in adults.
As a preventive measure, children can be vaccinated against TBE from their first birthday. There are special TBE vaccines available for children:
Encepur® children: for children from 1 to 11 years. Standard vaccination schedule: The second dose is given 14 days to 3 months after the first, the third dose 9 to 12 months after the second. The first booster vaccination should be given three years later, further booster vaccinations every 5 years.
The accelerated vaccination schedule is the same as for the corresponding adult vaccine (see above).
FSME-Immun® Junior: for children from 1 to 15 years. The standard and accelerated schedules are the same as for the corresponding adult vaccine.
TBE vaccination: side effects
As with any vaccination, side effects are also possible with the TBE vaccination, although the vaccines are generally well tolerated. If there are unwanted vaccine reactions, they are usually harmless:
Most often, the TBE vaccination causes side effects at the injection site (redness, swelling, pain). In addition, there may be general symptoms in the first few days after the vaccination, such as increased temperature, fatigue, fever, headache, muscle or joint pain, malaise or gastrointestinal complaints. Such side effects usually only occur after the first dose of vaccine, less often after further injections. In addition, they will soon subside on their own.
Very rarely does the TBE vaccination cause serious side effects such as allergic reactions. In isolated cases, disorders of the nervous system (including paralysis) have been observed after vaccination, mostly in adults.
If the TBE vaccination causes side effects, you should inform the doctor about this before the next vaccination appointment.
TBE vaccination: costs
The statutory health insurance companies usually pay for the TBE vaccination for people who live in risk areas. In the case of certain professional groups (such as foresters), the employer usually pays the costs of the vaccination.
In all other cases you usually have to pay for the TBE vaccination out of your own pocket, for example before traveling to a TBE risk area. But it doesn't hurt to ask your own health insurance company in advance to cover the costs.
Tags: alcohol drugs skin care news