Lymph gland cancer
and Martina Feichter, medical editor and biologist Updated onDr. med. Julia Schwarz is a freelance writer in the medical department.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Lymph gland cancer (malignant lymphoma) is a malignant disease of the lymphatic system. A distinction is made between two large groups - Hodgkin lymphoma and non-Hodgkin lymphoma. Typical symptoms of these cancers are painless, swollen lymph nodes, fever, weight loss, and night sweats. Lymph gland cancer can occur at any age. Men are affected slightly more often than women. Therapy and prognosis depend on the type and stage of lymphatic cancer. Read everything you need to know about lymph gland cancer here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. C84C85C82C81C83
Lymphatic cancer: description
Lymph gland cancer is the slang term for malignant lymphoma (formerly also called lymphosarcoma). This tumor disease is caused by degenerate cells of the lymphatic system (lymphatic system).
Lymphatic system (lymphatic system)
The lymphatic system is an important part of the body's defense system. It consists of the lymphatic system - a network of vessels comparable to the blood vessel system - and the lymphatic organs (e.g. thymus, bone marrow, lymph nodes, spleen, tonsils). The tissue fluid (lymph fluid, lymph) is collected and transported in the lymphatic system.
In addition, the lymphatic system is used for the formation, maturation and differentiation of a certain type of white blood cells, the lymphocytes (= lymph cells). They are extremely important for the immune defense because they can specifically identify and eliminate pathogens. The majority of the lymphocytes remain in their place of formation; only a small part passes into the blood. You can find out more about lymphocytes and their two subgroups (T and B lymphocytes) here.
The lymph nodes filter the tissue fluid (lymph) that flows through them. If you catch foreign bodies such as pathogens or cancer cells, the lymphocytes stored in the lymph nodes are activated - the immune system fights and removes the foreign bodies if possible.
The spleen also plays an important role in immune defense and blood purification. Read more about it here.
This is how lymph gland cancer develops
Lymph gland cancer occurs when a lymph cell (lymphocyte) degenerates and becomes a cancer cell. These can be, for example, lymphocytes in the lymph nodes or in the spleen or stem cells in the bone marrow (which can produce all other blood cells in addition to lymphocytes). The cancer cells differ in appearance from healthy lymph cells, no longer fulfill the actual task of a healthy cell and multiply in an uncontrolled manner.
As the disease progresses, lymph gland cancer can spread beyond the lymphatic system and affect other organs.
Lymphatic cancer: incidence and forms
Lymphatic cancer is a rare form of cancer. Every year two to ten out of 100,000 residents develop malignant lymphoma. Men are more often affected than women.
On the basis of fine tissue differences, doctors differentiate between two large groups of lymph gland cancer:
- Hodgkin's lymphoma (Hodgkin's disease): This independent form of lymph gland cancer is one of the five most frequently diagnosed cancers between the ages of 10 and 35. It most commonly occurs in young adulthood. In 2020, 8,856 women and 11,002 men were newly diagnosed with Hodgkin's lymphoma in Europe.
- Non-Hodgkin lymphoma (NHL): This includes all forms of lymphoma that are not classified as Hodgkin lymphoma - there are around 30 different types (e.g. plasmacytoma). In 2020, 55,601 women and 67,378 men were newly diagnosed with an NHL in Europe. The average age of the patients is 72 years (women) and 70 years (men).
Children can also develop lymphatic cancer, with both main groups of the disease occurring roughly equally - Hodgkin's lymphoma and non-Hodgkin's lymphoma each make up around six percent of all cancers in children.
Hodgkin's disease
You can read more about the causes, symptoms, diagnosis, treatment and prognosis of this form of lymph gland cancer in the article Hodgkin's disease.
Non-Hodgkin lymphoma
You can find out everything you need to know about this much more common group of lymph gland cancers in the article Non-Hodgkin Lymphomas.
Lymphatic cancer: symptoms
You can read everything you need to know about the typical signs of lymph gland cancer in the article Lymph gland cancer symptoms.
Lymphatic cancer: causes and risk factors
The exact causes of lymphatic cancer are not yet known. It is believed that several factors must come together before malignant lymphoma develops. Some of these factors increase the chances of developing lymph gland cancer - Hodgkin's lymphoma or non-Hodgkin's lymphoma.
Risk factors for Hodgkin lymphoma
It has long been known that the Epstein-Barr virus (EBV) - the causative agent of Pfeiffer's glandular fever (infectious mononucleosis) - can be causally involved in the development of this form of lymph gland cancer - but only in some of the Hodgkin's lymphomas. On the one hand, evidence of a previous EBV infection can be found in only about half of all Hodgkin lymphoma patients. On the other hand, such infections are widespread, while lymph gland cancer is rare.
Congenital diseases of the immune system and acquired immune deficiencies (e.g. as a result of an HIV infection) are further risk factors for Hodgkin's disease.
Smoking for many years may also increase the risk of the disease.
A possible genetic predisposition is also being discussed: children and siblings of Hodgkin lymphoma patients have a slightly increased risk of developing this form of lymphatic cancer themselves. However, this relationship still needs to be explored further.
Risk factors for non-Hodgkin lymphoma
No generally applicable risk factors for the heterogeneous group of non-Hodgkin lymphomas (NHL) can be identified.
Certain pathogens are considered risk factors for individual forms of non-Hodgkin lymphoma. For example, the Epstein-Barr virus mentioned above can contribute to the development of Burkitt's lymphoma - a form of lymphatic cancer that occurs mainly in Africa. The so-called MALT lymphoma of the stomach (MALT = Mucosa Associated Lymphoid Tissue), on the other hand, is favored by the "stomach germ" Helicobacter pylori.
Various chemical substances can also increase the risk of some non-Hodgkin lymphoma, such as benzene and other organic solvents that are widely used in industry.
As with Hodgkin's disease, a congenital or acquired immune deficiency can also contribute to the development of tumors in some non-Hodgkin's lymphomas. An HIV infection, chemotherapy or immunosuppressive therapy (e.g. after organ transplantation) can be responsible for an acquired immune deficiency.
Radioactive radiation and old age are also considered risk factors.
Other possible risk factors such as genetic factors (if there are several cases of illness in a family) and lifestyle factors are being researched.
Lymphatic cancer: examinations and diagnosis
Painless swollen lymph nodes - typical symptoms of lymph gland cancer - can also have many other causes. However, if the painless swelling of the lymph nodes persists for weeks, possibly accompanied by symptoms such as fever, night sweats and unwanted weight loss, you should urgently consult a doctor. If you suspect lymph gland cancer, the right person to contact is your general practitioner or a specialist in internal medicine and oncology.
anamnese
The doctor will first take a detailed discussion with you about your medical history (anamnesis). Possible questions from your doctor include:
- Have you accidentally lost weight in the past few months?
- Have you recently woken up at night from being "bathed in sweat"?
- In the past, did you have frequent fever (with no signs of infection) and felt weak?
- Have you noticed painlessly enlarged lymph nodes (for example on the neck, under the armpits or on the groin)?
- Are you aware of any illnesses?
- Are / have there been cases of cancer in your family? If so, what type of cancer?
Physical examination
As part of the physical exam, the doctor will scan your lymph nodes and abdomen and look at your tonsils. In lymph gland cancer, lymphatic organs such as lymph nodes and / or spleen etc. are typically enlarged painlessly.
Blood tests and immunohistochemistry
Blood tests are an important diagnostic tool for suspected lymphatic cancer. The blood count of those affected shows changed values for the various blood cells: the other cells in the blood are displaced by the strong increase in the number of degenerated lymphoma cells. This can lead to a lack of erythrocytes (anemia = anemia), blood platelets (thrombopenia or thrombocytopenia) and also leukocytes (leukopenia or leukocytopenia).
The latter can, however, also be increased (leukocytosis), as is often the case with Hodgkin's disease: The differential blood count (breakdown of the various subgroups of leukocytes) shows that this increase in total leukocytes is due to the increase in the subgroup of "eosinophilic granulocytes" ( Eosinophilia).
The functional values for various organs such as the liver and kidneys can also be seen in the blood count. If these values deviate from the norm, this can indicate that the lymph gland cancer has already affected the organ concerned.
Elevated inflammation levels may also be seen in the blood of lymphatic cancer patients (especially increased blood sedimentation). Such an increase is, however, unspecific, that is: The inflammation values in the blood can also be increased for many other reasons.
-
"Accept the disease!"
Three questions for
Prof. Dr. med. Marcus Hentrich,
Internal oncology -
1
When is antibody therapy used?
Prof. Dr. med. Marcus Hentrich
It is chosen for almost all so-called B-cell lymphomas. There it can significantly increase the healing rate. It's a clever principle: the antibodies bind precisely to the surfaces of the cancer cells and thus help the immune system to eliminate them. Treatment is usually combined with chemotherapy. The cancer cells are attacked on different levels.
-
2
How well do patients tolerate antibody therapy?
Prof. Dr. med. Marcus Hentrich
Patients may develop a fever or chills, especially when they are used for the first time. This is due to the fact that the antibodies are an exogenous protein and therefore initially alert the patient's immune system. But these side effects are easy to accept - the advantages far outweigh them.
-
3
What can I do myself to support the treatment?
Prof. Dr. med. Marcus Hentrich
Cancer is a serious disease. But it becomes even more threatening when you let fear overwhelm you. Accept the diagnosis and find your way with it. The thankful thing is that lymphoma can be cured in many cases. And if they don't, you can at least control them well over a long period of time. It is therefore important that you cooperate well with your treatment.
-
Prof. Dr. med. Marcus Hentrich,
Internal oncologyProd. Dr. med. Marcus Hentrich is medical director and chief physician, as well as a specialist in internal medicine, hematology and oncology at the Rotkreuzklinikum Munich.
Tissue sample (biopsy)
For a reliable lymph gland cancer diagnosis, the removal and analysis of tissue samples is necessary. In this way it can also be determined what type of lymph gland cancer it is.
As a rule, the surgeon removes a complete lymph node (lymph node extirpation) - for example from the neck or groin region - which he examines under the microscope (histologically) for the presence of lymphoma cells.
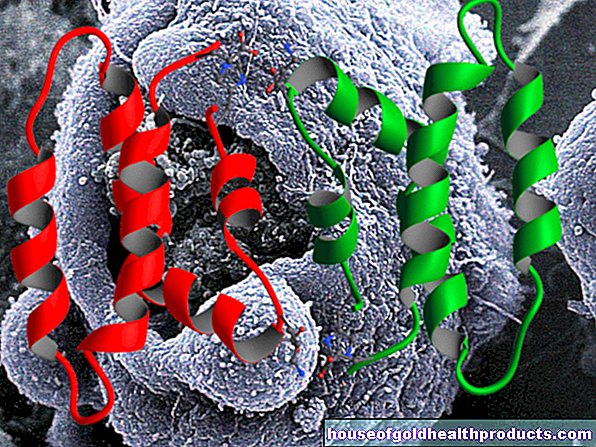
In the case of non-Hodgkin lymphoma (NHL), the cancer cells can then be further specified by means of immunohistochemical tests: Using certain features on the surface of the lymphoma cells, it is possible to determine whether the non-Hodgkin lymphoma is in degenerated B or T lymphocytes has its origin - B-lymphocytes have the surface feature "CD20", T-lymphocytes "CD3" on their surface. Antibodies and certain chemical substances are used to identify these surface features (hence "immunohistochemistry").
Samples (biopsies) can be taken not only from lymph nodes, but also from other tissues if necessary. For example, if a skin lymphoma is suspected (cutaneous lymphoma), a sample is taken from the skin, if a MALT lymphoma is suspected, a sample is taken from the gastric mucosa. Both lymphomas are non-Hodgkin lymphomas.
Further investigations
Once the diagnosis of lymph gland cancer has been made, it is important to determine how far the Tyumor has already spread in the body. Imaging methods such as an X-ray examination of the chest (chest X-ray), an ultrasound examination of the abdomen and / or computed tomography (CT) help. The latter is often combined with positron emission tomography (PET). This so-called PET / CT is also important for planning therapy for Hodgkin's lymphoma.
In some patients, an additional examination of the bone marrow is necessary to determine whether it has been infected. The iliac crest is usually punctured with a needle under slight sedation and some bone marrow is suctioned off. The bone marrow is then examined under a microscope.
In rare cases, a sample of the nerve water (cerebrospinal fluid = liquor) must be taken and examined.
The stage of cancer can be determined on the basis of further examinations. Both the therapy plan and the assessment of the prognosis are based on this tumor stage.
Lymph gland cancer: staging (according to Ann-Arbor)
Lymph gland cancer (malignant lymphoma) is divided into disease stages (staging) on the basis of the test results, according to the so-called Ann Arbor classification with its four stages. It was originally developed for Hodgkin's lymphoma, but is now also used for non-Hodgkin's lymphomas.
|
stage |
Involvement of the lymph nodes |
|
I. |
Involvement of only one lymph node region |
|
II |
Involvement of two or more lymph node regions on the same side of the diaphragm (either in the chest or in the abdomen) |
|
III |
Involvement of lymph node regions on both sides of the diaphragm (i.e. both in the chest and in the abdomen) |
|
IV |
Diffuse involvement of the extralymphatic organ / area (e.g. bone marrow) with or without involvement of the lymph node regions |
The various stages can be specified further by adding additions. If a lymph gland cancer patient is in stage III (S), this means that in addition to lymph node regions on both sides of the diaphragm, the spleen is also affected by the cancer.
With parameters A and B as an addition to the tumor stage, it can be shown whether the patient shows B symptoms (weight loss, fever, night sweats) - parameter A stands for the absence of B symptoms, parameter B for the presence of B symptoms. Symptoms.
Lymphatic cancer: treatment
Malignant lymphoma should always be treated in a specialized clinic. These are mostly hematological-oncological or internal wards at a university clinic. The patient receives an individual therapy plan adapted to the stage of the disease. The age and general health of the patient are also taken into account when it is drawn up.
The therapy options for lymphatic cancer primarily include chemotherapy and / or radiation therapy (radiation). In certain cases, other therapies can be considered in the treatment of malignant lymphomas, such as antibody therapy. If the lymph gland cancer grows only very slowly, treatment can sometimes (for the time being) be dispensed with. Affected patients are closely monitored ("watch and wait").
Chemotherapy and radiation therapy for lymphatic cancer
In the early stages of lymph gland cancer, radiation therapy can be helpful because it still does not spread through the body. In non-Hodgkin's lymphoma, local radiation alone may be sufficient in some cases. Usually, however, it is combined with another therapy method - very often with chemotherapy.
In the early stages of Hodgkin's disease, on the other hand, combined chemotherapy and radiation therapy is always recommended. Irradiation on its own is not recommended here. Radiation therapy is carried out after chemotherapy is completed.
Chemotherapy and radiation therapy also play an important role in the more advanced stages of lymphoma.
Stem cell transplantation for lymphatic cancer
Another therapeutic option in certain cases of lymph gland cancer is the transfer of blood-forming stem cells (haematopoietic stem cell transplantation). The doctor first obtains healthy blood-forming stem cells, mostly from the patient's own body (autologous stem cell transplant). In principle, such stem cells can be obtained directly from the bone marrow (bone marrow transplantation) or from peripheral blood (= blood outside the bone marrow). Usually you choose the second variant. The stem cells obtained are frozen until they are transferred back.
In the next step, the patient receives high-dose chemotherapy to destroy all of his bone marrow and the cancer cells it contains. Immediately afterwards, the previously removed healthy blood stem cells are transferred to him, which then start a new blood formation without cancer cells.
In certain cases, donated blood stem cells from another person can also be considered for transplantation (allogeneic stem cell transplantation).
Immunotherapy for lymphatic cancer
Some patients with lymphatic cancer receive immunotherapy - often in combination with another therapy, such as chemotherapy (the combination is called chemoimmunotherapy). Immunotherapy for cancer aims to strengthen the immune system and target it against the cancer cells.
There are several types of immunotherapy that are available in treating malignant lymphoma.
Antibody therapy
In this form of immunotherapy, the patient is administered artificially produced antibodies that bind specifically to the cancer cells and destroy them in different ways. Two examples:
The antibody rituximab can be used to treat certain cases of non-Hodgkin lymphoma (NHL). It specifically binds to the CD20 protein on the surface of the cancer cells and thus signals the immune system's defense forces to destroy this cell. Antibody therapy with rituximab can be considered for NHL forms that have developed from degenerate B lymphocytes (B cell lymphomas). This type of lymphocyte carries the CD20 protein on its surface (on the other hand, T lymphocytes lack it).
For certain patients with Hodgkin's lymphoma, the active ingredient brentuximab vedotin can be considered. It is an artificially produced antibody that is loaded with a cytostatic - a substance that inhibits cell division. The antibody attaches to a certain surface protein (CD30), which is increasingly found on degenerated B and T lymphocytes. It is then absorbed into the interior of the cancer cell along with its "charge". There the cytostatic agent is split off, whereupon it unfolds its effect - the cancer cell can no longer multiply and as a result dies.
Immunotherapy with checkpoint inhibitors
For some patients with Hodgkin lymphoma, treatment with checkpoint inhibitors is an option. These are also special antibodies. However, these do not act directly on cancer cells, but rather influence certain control points of the immune system that slow down immune reactions (so-called immune checkpoints):
Some tumors such as Hodgkin's lymphoma can activate these "brakes" on the immune system and thus protect themselves from an immune attack. Checkpoint inhibitors such as nivolumab release these "brakes" so that immune cells can now act against the cancer.
CAR T cell therapy
A very new form of immunotherapy is CAR-T cell therapy. It is useful for treating certain types of non-Hodgkin lymphoma (and leukemia).
Here, immune cells (T cells) are taken from the patient and genetically modified in the laboratory: The T cells thereby form a receptor on their surface (CAR = chimeric antigen receptor) that can specifically recognize cancer cells and dock onto them. It then sends a signal to the T cell to destroy the bound cancer cell.
In preparation for this treatment, the patient is treated with mild chemotherapy. It kills some of the cancer cells as well as the body's own T cells. This "gap" in the T-cell inventory is filled by the CAR-T-cells produced in the laboratory, which are infused into the patient.
Therapy with signaling pathway inhibitors
So-called signaling pathway inhibitors are a very new therapeutic option for certain non-Hodgkin lymphomas. These are drugs that switch off important growth signals in the cancer cells - the cell can no longer multiply.
One example is the active ingredient idelalisib. It can be given to patients with follicular lymphoma when chemotherapy and antibody therapy have not been effective.
For complete information on treating the different types of lymphatic cancer, see the articles Hodgkin's Disease and Non-Hodgkin's Lymphoma.
Lymphatic cancer: disease course and prognosis
Whether lymph gland cancer is curable depends largely on the stage and the histological form of the disease. But other factors also influence the prognosis, such as the age of the patient, possible complications and previous illnesses. Thus, no generally valid information can be made about the chances of a cure for lymph gland cancer. In general, however, the following applies:
The prognosis for Hodgkin lymphoma is generally quite favorable. A cure is possible in many patients: In 84 percent of the affected women and 86 percent of the affected men, this lymph gland cancer has not (yet) led to death five years after the diagnosis (relative 5-year survival rate).
It usually looks a little worse with non-Hodgkin lymphoma (NHL). On average, the relative 5-year survival rate here is 70 percent for women and 68 percent for men. In individual cases, however, life expectancy and the chances of recovery for this group of lymph gland cancer can vary considerably. An initial assessment is possible based on the growth behavior of the tumor:
- Some NHL types grow very aggressively (e.g. Burkitt's lymphoma). These so-called highly malignant lymphomas do not necessarily have a bad prognosis - it is precisely the high rate of cell division that ensures that these forms of lymph gland cancer usually respond well to treatment (such as chemotherapy). Many patients can therefore be cured with an initial intensive treatment (if the tumor is discovered early).
- Other NHL types - so-called low-malignant lymphomas - develop slowly over years to decades (e.g. MALT lymphoma, hairy cell leukemia). They are considered to be chronic diseases: treatment can usually only suppress them, but not permanently cure them. Affected patients must therefore be given lifelong medical care and, if necessary, be treated repeatedly.
Risk of secondary tumors
For both main groups of lymph gland cancer (Hodgkin lymphoma and non-Hodgkin lymphoma), the following also applies: Both chemotherapy and radiation therapy, with which a tumor is treated, can cause a second tumor as a long-term consequence - i.e. trigger a new cancer years or decades later .
Tags: palliative medicine eyes vaccinations