Atrial fibrillation
and Dr. med. Andrea ReiterClemens Gödel is a freelancer for the medical team.
More about the expertsDr. med. Andrea Reiter is a freelance writer for the medical editorial team.
More about the experts All content is checked by medical journalists.Atrial fibrillation is a very common heart rhythm disorder in which the heart beats irregularly. It is the most common form of abnormal heart rhythm - over six million people in Europe suffer from it. Sometimes people do not even notice the atrial fibrillation. Others experience a "palpitations" or a racing heart. The risk of stroke is increased. Find out everything about the symptoms, diagnosis and therapy for atrial fibrillation.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. R00I48I46I47I49I45I44
Atrial fibrillation: description
Atrial fibrillation is the most common type of arrhythmia. Mostly the elderly are affected. Ten percent of people over the age of 70 suffer from atrial fibrillation.
Normally, an electrical signal is generated in the sinus node in the right atrium, which is conducted into the ventricles via a conduction system. There it triggers a muscle contraction and thus the heartbeat. With atrial fibrillation, many circulating electrical excitations arise in the atria, some of which are also conducted to the ventricles via the conduction system. This results in an irregular heart rhythm (arrhythmia). It is usually too fast (tachyarrhythmia). If a so-called conduction block is added, it is sometimes too slow (bradyarrhythmia).
Because of the circulating electrical signals, the atria are unable to fill themselves completely with blood. Therefore, the amount of blood ejected from the heart is also reduced. If the heart is already weakened, even less blood is pumped. The blood pressure drops.
Atrial fibrillation: forms
Doctors differentiate between three different forms of atrial fibrillation:
- Paroxysmal: occurs spontaneously and in a seizure manner and often lasts for several minutes to hours. Typically, paroxymal atrial fibrillation lasts less than 24 hours. It can reach a maximum duration of seven days.
- Persistent: The heartbeat does not find its way back to its usual rhythm on its own; atrial fibrillation only ends with cardioversion.
- Permanent: chronic atrial fibrillation, should or can no longer be converted into a stable sinus rhythm.
Most often, atrial fibrillation develops over the course of life. In many cases, it initially occurs as a paroxysmal attack and then lasts for minutes, hours or even days. At some point it develops into chronic (permanent) atrial fibrillation, which can persist even with drug treatment.
What is atrial flutter?
Another form of arrhythmia also starts in the atria and is treated similarly, but has a different cause. Read more about this in the article Atrial Flutter.
Atrial fibrillation: symptoms
Atrial fibrillation is often symptom-free. Around two-thirds of those affected feel nothing or only a small decrease in performance from a seizure-like atrial fibrillation.
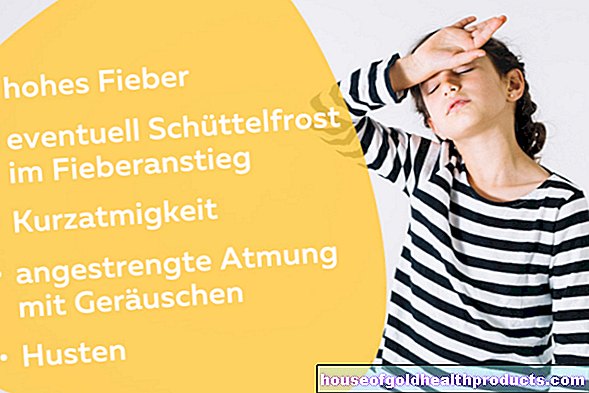
A third of those affected have these symptoms:
- Racing heart
- dizziness
- Shortness of breath
- Chest pain or anxiety
The symptoms depend on the speed of the heartbeat. If the heart beats normally despite the atrial fibrillation, those affected may only feel tiredness and dizziness. If the heart beats too fast (often over 100 beats per minute), the affected person usually feels an uncomfortable racing heart, often chest pain and shortness of breath. If the heart beats too slowly, they may feel dizzy or faint.
If the atrial fibrillation becomes chronic, the organism can "get used to" the arrhythmia and those affected no longer have any pronounced symptoms.
Atrial fibrillation: cause and risk factors
Atrial fibrillation mostly develops with age. The causes of atrial fibrillation cannot always be clearly clarified. Since the structure of the heart changes with age and the heart tissue increasingly scars, electrical signals in the atrium are incorrectly transmitted. This causes the signals to circulate through the atrial tissue and disrupt normal heart activity.
There are some risk factors that can promote atrial fibrillation. Many chronic diseases are included, for example:
- long-standing high blood pressure
- Heart diseases (e.g. heart valve defects, heart muscle weakness)
- Diabetes mellitus
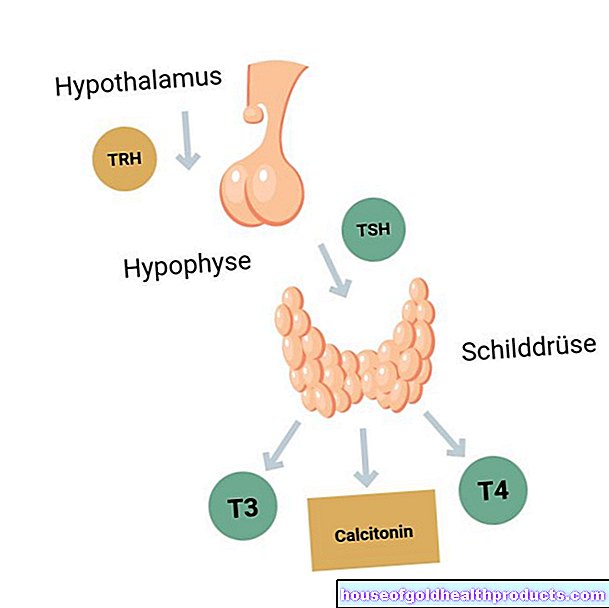
- Thyroid disease
- Lung disease
- Sleep apnea
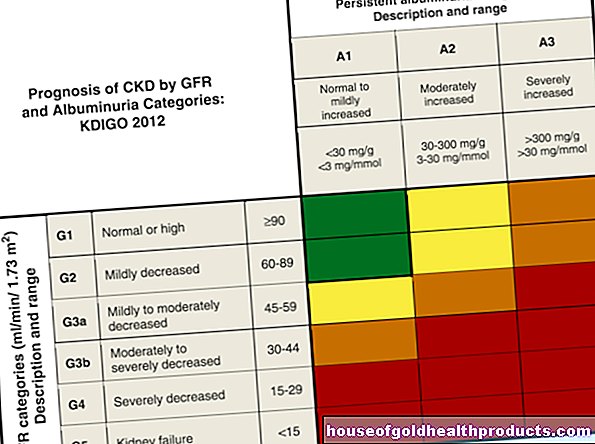
- Kidney disease
But lifestyle also has an influence on the development of atrial fibrillation. The following factors can trigger atrial fibrillation:
- significant alcohol consumption
- Obesity
- stress
Researchers found that atrial fibrillation risk also has a genetic component. Sometimes the arrhythmia develops without an apparent cause.
Atrial fibrillation: diagnosis and examination
The specialist in atrial fibrillation is a cardiologist. First, the doctor will ask about the medical history. The following questions are important:
- How often and for how long do you feel your heart racing?
- Do certain factors such as alcohol consumption, sleep deficit or surgery trigger the racing heart?
- Do you have any heart or thyroid disease?
- Do you have any other complaints while racing your heart?
- Does atrial fibrillation run in your family?
This is followed by a physical examination and a pulse and blood pressure check.
Electrocardiogram (EKG)
The most important test to diagnose atrial fibrillation is an electrocardiogram (EKG). The electrical currents of the heart are measured using electrodes that are attached to the chest.
Sometimes an EKG has to be written over several days. Doctors then speak of a long-term EKG. For this purpose, small EKG machines are available that are hung around the neck. The EKG can also be recorded during physical activity. The patients have to exert themselves physically on a kind of home trainer.
Echocardiography
An ultrasound examination of the heart (echocardiography) can examine its structure and pumping behavior. Checking for blood clots in the heart is especially important if atrial fibrillation has already been diagnosed.
In order to examine the atria more closely and to be able to detect any blood clots that may develop, the ultrasound head is inserted into the esophagus with a tube like a gastroscopy. In the middle of the esophagus, the right atrium is very close to the ultrasound head. It can be judged particularly well from this position. This examination is called transesophageal echocardiography. It is usually performed under a light anesthetic.
Atrial fibrillation: treatment
If the atrial fibrillation has developed due to another condition such as an overactive thyroid, this must first be treated. In many cases, the arrhythmia will then improve on its own.
If atrial fibrillation has occurred in attacks, it will often go away on its own in a few hours or days.
Medical therapy
Patients who have already been diagnosed with atrial fibrillation are usually prescribed a medication by their doctor, which they must take as soon as the atrial fibrillation recurs. With this drug, the heart rhythm usually "jumps" back into normal rhythm.
The so-called antiarrhythmic drugs are very effective, but often have not inconsiderable side effects. In the event of an overdose, the heart sometimes beats so slowly that the patient becomes very dizzy or tired. The following active ingredients are used in atrial fibrillation:
- Vernakalant (antiarrhythmic)
- Flecainide (antiarrhythmic)
- Propafenone (antiarrhythmic)
- Amiodarone (potassium channel blocker)
If the seizures of palpitations occur very frequently or are very uncomfortable, other medication can be taken to prevent it from the outset. Beta blockers such as metoprolol, bisoprolol and carvedilol are suitable. Here, too, dizziness, but also depression, can occur as side effects.
Since the risk of stroke is increased by frequent or persistent atrial fibrillation, many patients have to take medication that thins the blood.
Cardioversion
Sometimes atrial fibrillation is very persistent and does not go away on its own or under medical therapy. The heart rhythm can then also be normalized by external electrical currents. This therapeutic measure is called cardioversion.
The electrocardioversion works in a similar way to defibrillation during resuscitation. First, the patient is connected to various monitoring devices in order to be able to observe the blood pressure and the oxygen supply. Then the patient is anesthetized for a short time and electricity is passed through two electrodes into his heart for a fraction of a second. The heart often falls back into its normal rhythm as a result of the electrical surge. People who have paroxysmal atrial fibrillation can be treated with electrical cardioversion instead of medication.
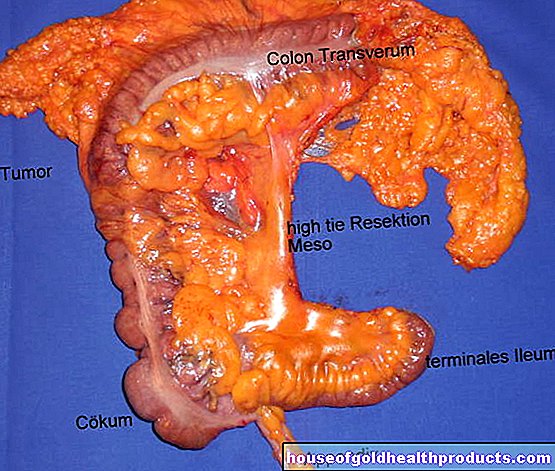
Pulmonary vein isolation
Many patients can be cured of atrial fibrillation through a so-called pulmonary vein isolation. The regions in the heart that trigger the atrial fibrillation are desolated. First, a wire (catheter) is passed through the inguinal veins into the heart. Since atrial fibrillation often occurs in the area where the pulmonary veins (pulmonary veins) open into the heart, the tissue there is obliterated. The chance of recovery with this procedure is 60 to 80 percent.
Pacemaker implantation
Affected people whose heartbeat is too slow sometimes have to be treated with a pacemaker implantation. The pacemaker ensures a faster and more stable heartbeat.
Stroke protection
If people suffer from paroxysmal or chronic atrial fibrillation, there is a risk that blood clots will form in the atrium, which can trigger a stroke. Since the blood in the atrium no longer circulates properly due to the arrhythmia, it can "clump". The blood clots can travel through the heart into the bloodstream and from there into the brain vessels.
When a cerebral vessel becomes blocked, it is called a stroke. Taking blood-thinning medication can reduce the risk of stroke. However, bleeding complications can occur.
A newer method of protection against a stroke is the closure of the so-called atrial appendage. The atrial appendage is a bulging of the atrium, in which the clots form particularly often.
Exercise for atrial fibrillation
Exercise can reduce the risk of recurrence of atrial fibrillation attacks. However, it shouldn't be too much. High-performance athletes in endurance sports (marathon, cross-country skiing) are up to eight times more likely to experience an episode of atrial fibrillation.
Can you do sports with this arrhythmia? The health-promoting effect of moderate endurance sport for cardiac arrhythmias is scientifically undisputed. People with atrial fibrillation can significantly reduce the frequency of atrial fibrillation episodes with proper exercise and weight loss.
Start training with atrial fibrillation
Before starting training, patients with atrial fibrillation should always discuss the appropriate training dose (intensity and duration) with their doctor. He can make an individual recommendation and determine the patient's performance with various tests.
In this stress test, the doctor determines the optimal heart rate for endurance training.
Which sport for cardiac arrhythmias?
Low to moderate endurance training is recommended for patients with atrial fibrillation. Three to five training units per week of 20 to 30 minutes if possible are good for the heart. In total, patients should get 60 to 120 minutes of exercise per week.
If a patient can increase their exercise capacity by more than 50 watts, which corresponds to faster walking, the risk of recurrence of atrial fibrillation is reduced by more than a third over a five-year period. If the patient also sheds a few extra pounds, he can reduce the risk of renewed atrial fibrillation attacks by as much as three quarters. Exercise and weight loss have a similar effect to medication.
The following endurance sports are good for atrial fibrillation:
- (fast) walking
- jog
- Walking / Nordic Walking
- rowing
- Cycling or ergometer training
- To dance
Weight training prevents falls
In addition to endurance training, cardiac patients also benefit from low-dose strength training. Because especially older people are affected by cardiac arrhythmias such as atrial fibrillation. Strength training gives you more security in everyday life and can help prevent falls.
Exercise your legs particularly gently with these exercises:
- Strengthening the abductors (extensor muscles): Sit upright on a chair and press your hands against your knees from the outside. The legs work against the hands. Hold the pressure for a few seconds and then relax.
- Strengthening the adductors (flexor muscles): Sit upright on a chair with your hands between your knees. Now push outwards with your hands. The legs work against the hands. Hold the tension for a few seconds and then relax completely.
Atrial fibrillation patients can walk or jog on an uneven surface to improve their sense of balance. For example, sand or a soft floor mat for indoor sports is suitable. The ground also trains the muscles in the legs and torso.
Since muscle mass consumes more energy than fat, muscles increase the basal metabolic rate and help you lose weight. Therefore, cardiac patients benefit twice from light strength exercises: the muscles become stronger, the gait safer and the love handles disappear faster.
These sports are not suitable for atrial fibrillation
Atrial fibrillation often occurs suddenly and has side effects such as weakness, dizziness, or shortness of breath. Therefore, sport in the water is only suitable to a limited extent. Supervised aqua aerobics are less risky than swimming in open water.
Climbing or mountain hiking or other sports with an acute risk of falling are not suitable for patients with atrial fibrillation.
Patients who take anticoagulants for stroke prophylaxis should choose sports with a low risk of injury. Injuries cause internal or external bleeding that is difficult to stop with the medication you are taking.
Unsuitable sports for cardiac arrhythmias such as atrial fibrillation are therefore:
- Mountain biking
- Snowboarding
- Alpine skiing
- Boxing
- karate
- Full contact sports (handball, soccer, ice hockey, etc.)
Atrial fibrillation: disease course and prognosis
Even after successful therapy, it is always possible that atrial fibrillation will recur. Relapses are particularly common in people with heart disease.
Paroxysmal atrial fibrillation can develop into permanent atrial fibrillation over time if left untreated. The longer the arrhythmia persists, the more difficult it is to treat it. If it has occurred as a result of other diseases, for example an overactive thyroid, the arrhythmia often disappears on its own after treatment.
The prognosis of atrial fibrillation is particularly determined by accompanying heart disease. If the heart is already weakened, atrial fibrillation can significantly increase mortality. The increased risk of stroke can be contained well with anticoagulant drugs. The risk of overdosing is particularly high in the elderly, as their liver is no longer working as well, they sometimes have to take many other medications, drink too little or fall more frequently. In these cases it is sometimes necessary to advise against anticoagulant medication.
Atrial fibrillation itself cannot be prevented, but the diseases that cause it can be prevented. A healthy diet, regular exercise and the avoidance of stimulants reduce the risk of coronary artery disease - the main cause of atrial fibrillation.
Tags: womenshealth drugs Menstruation