Pneumonia in Children
Updated onSophie Matzik is a freelance writer for the medical team.
More about the experts All content is checked by medical journalists.Of all respiratory diseases, pneumonia is the most common in children. It is usually triggered by bacteria or viruses. Since the symptoms of the disease can be very unspecific, it is difficult to detect pneumonia in children. Early treatment is very important - if the course is severe, pneumonia in children can lead to death. Read everything you need to know about pneumonia in children here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. J15J14J16J18J12P23J13
Pneumonia in Children: Description
Pneumonia in children (like adults) has inflamed the lung tissue and airways in the chest. An infection with pathogens such as bacteria, viruses or fungi is usually responsible for the disease. The symptoms of pneumonia in young children are similar to those in adults. Affected people suffer from a fever and cough and feel limp and tired. Often, however, there are also other symptoms in children that are rather rare in adults - for example chills and body aches.
Children are particularly at risk for pneumonia. Since small children in particular are not yet aware of hygiene, pathogens such as bacteria or viruses are quickly passed on - mostly through coughing or sneezing (droplet infection). Mutual contagion occurs so quickly, especially in community facilities such as schools, kindergartens or homes. In addition, children's immune systems are often not yet as effective as those of adults. Children therefore generally have more infections and are therefore also at greater risk for serious illnesses such as pneumonia.
frequency
Pneumonia is the most common respiratory disease in young children and older children. It is even one of the most common causes of childhood death worldwide. Every year around 1.8 million children around the world die of pneumonia. In Germany, the number of deaths is comparatively low, which is due on the one hand to the good medical care and on the other hand to the possibility of vaccination against the most common pathogens.
Pneumonia in children: causes
Pneumonia in children can be the result of another respiratory disease (such as asthma) or a complication of other conditions (such as cystic fibrosis). Pneumonia is less common in children with no previous illnesses or risk factors.
Bacteria or other pathogens (such as viruses, fungi) are often the cause of pneumonia in children. Other causes such as gases that irritate the respiratory tract or disorders of the immune system, on the other hand, are rarely the cause of pneumonia in children.
Bacterial pneumonia in children
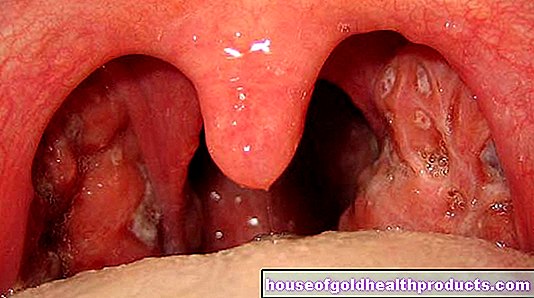
As in adults, bacteria are usually responsible for pneumonia in children. Babies and toddlers are also susceptible to less common pathogens that older children and adults would not get sick with. Typical germs of pneumonia in children are pneumococci (Streptococcus pneumoniae), Streptococcus agalactiae, Hemophilus influenzae and Escherichia coli. The pathogens of so-called atypical pneumonia such as chlamydia or mycoplasma are more likely to occur in children of school age.
As a rule, symptoms of bacterial pneumonia in children are much more pronounced than those of viral pneumonia. Often, bacterial pneumonia occurs after a virus-induced pneumonia. Doctors then speak of a so-called superinfection.
Viral pneumonia in children
Viral pneumonia in small children is caused, for example, by the respiratory syncytial virus (RS virus), the adenovirus or the influenza virus (flu virus). RS virus pneumonia can be particularly severe in infants.
Fungal pneumonia in children
Fungi are rarely responsible for pneumonia in children. Girls and boys with weakened immune defenses and premature babies are most likely to be affected.
Infection in a sick child
Children (and adults) with infectious pneumonia are potentially contagious to others. The pathogens can be transmitted to other people when you cough or sneeze (droplet infection). Especially with children, therefore, sufficient hygiene must be observed: Always carry a clean handkerchief with you and make sure that your child sneezes or coughs at you and not other people.
Pneumonia in Children: Recognizing Symptoms
Detecting pneumonia in children and young children is not always easy. Especially with babies and very young children who cannot speak yet, you need to look out for the following signs that distinguish pneumonia from a common cold:
- Unwillingness to drink and refusal to eat
- Cough, often with greenish or yellowish expectoration
- bloated stomach
- fast and shallow breathing (tachypnea)
- erect nostrils when inhaling (nostrils breathing)
- high fever
- noticeably high heart rate (children generally have a higher heart rate than adults)
- apathetic behavior
In children who can already speak, it is usually easier to recognize pneumonia and better assess the severity of the disease. The children then complain - similar to adults - of a poor general state of health, a strong feeling of illness and, in addition to the symptoms mentioned above, of the following complaints:
- Headache and pain in the limbs
- chills
- Chest pain when coughing, some of which radiate into the (right) lower abdomen
Pneumonia in Children: Diagnosis and Treatment
The diagnosis of pneumonia in infants and children is essentially the same as that in adults. First the doctor collects the medical history (anamnesis), whereby the parents usually provide him with the necessary information (children are often too small for this). Specific questions that can help the doctor if there is a suspicion of pneumonia in children are, for example:
- Has your child suffered from a cough and fever for a long time?
- Does your child cough a lot? Did it cough up phlegm?
- Has your child been feeling weak and tired for a long time?
- Has your child been eating less lately?
- Does your child behave differently than usual (e.g. change of character)?
This is followed by a physical exam. The doctor uses a stethoscope to listen to the child's lungs at various points on the back and chest. The inflamed lung tissue and the mucus that can collect between the alveoli cause typical breathing noises (ringing, fine-bubble rattling noises).
roentgen
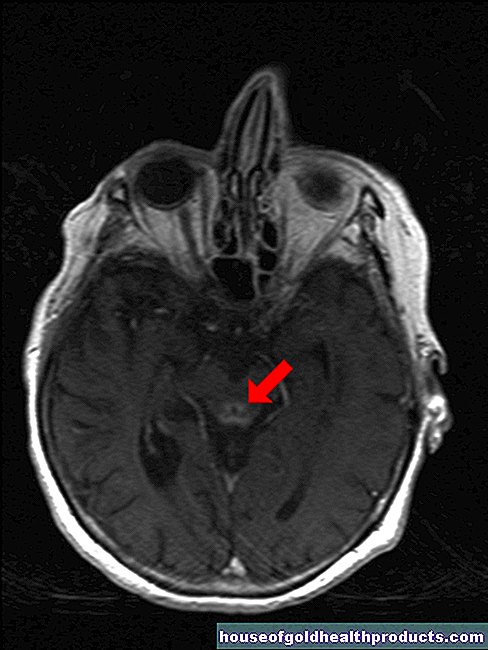
In order to be able to assess the condition of the lungs more precisely, a chest x-ray is necessary (chest x-ray). It is the most important test for suspected pneumonia.
Taking a single x-ray of children is harmless in terms of radiation exposure. Excessive radiation exposure and corresponding consequential damage would only be expected if a large number of X-ray examinations were carried out in a very short time
Laboratory tests
A laboratory analysis is necessary to prove which pathogens caused the pneumonia. For this purpose, sputum is cultivated. This means that an attempt is made in the laboratory to reproduce bacteria from the sputum and then to identify them. A laboratory analysis is important for therapy planning because different pathogens react differently to antibiotics. This can even be tested in the laboratory by adding various antibiotics to the pathogens that have been cultivated.
A sputum sample is not always necessary. It is usually only taken if the doctor cannot make a clear diagnosis based on the symptoms. In complicated cases, for example if a therapy does not work, it may be necessary to take a sample of the mucous membrane (biopsy).
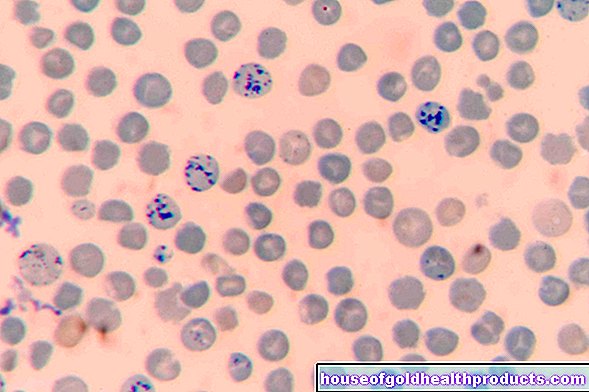
Blood tests can confirm suspicions of pneumonia in children. In general, when there is inflammation in the body, the C-reactive protein (CRP) and the number of white blood cells (leukocytes) are typically increased.
Treatment of pneumonia in children
Treatment depends on the age of the child and the severity of the pneumonia. Babies up to six months of age and children with comorbidities or very severe disease should be treated in hospital. Older children with no accompanying illnesses can be treated at home. However, you need to adhere to bed rest, and parents should strictly ensure that the therapy prescribed by the doctor is followed.
Antibiotics
Bacterial pneumonia in children (like adults) is usually treated with antibiotics. The treatment takes place over several days. Which antibiotic is used in each individual case depends on the type of bacteria. Babies and infants up to six months old are given the antibiotic by infusion. Oral ingestion is still very difficult at this age. Older children, on the other hand, can usually be given the antibiotics as juice or in tablet form without any problems.
Antibiotics are also often prescribed for viral pneumonia, although viruses do not respond to them at all. Often, however, there is already an additional bacterial infection or this should be prevented by administering antibiotics.
Bronchitis in children is also often treated with antibiotics, although it is mostly viral. Here, too, the antibiotics should prevent an additional bacterial infection - because in this way, bronchitis can develop into bacterial pneumonia.
Antipyretic agents
If the fever is high, the doctor will also prescribe antipyretic medication. As a rule, they are safe to take, even for young children, provided that the dosage prescribed by the doctor is adhered to. Fever juices especially suitable for children with the active ingredients ibuprofen or paracetamol are available in stores. Under no circumstances should children receive the fever-lowering pain reliever acetylsalicylic acid (ASA), as this can develop the life-threatening Reye's syndrome!
Expectorant and cough suppressant
With pneumonia, a lot of mucus collects in the tissue between the alveoli (interstitium). This mucus is carried out by coughing. Expectorant drugs can make it easier to cough up.
At night, on the other hand, it can make sense to give a cough suppressant so that the child can sleep better.
Expectorant and cough suppressant must not be taken at the same time - the increased dissolved mucus is then not coughed up, which can cause or worsen breathlessness!
Further measures
Coughing up mucus can also be facilitated by inhalation therapy and a vibration massage:
In inhalation therapy, a solution of table salt and expectorant additives is inhaled. As a rule, the children are dependent on the help of their parents.
So-called vibration therapy is carried out by a physiotherapist. For this purpose, a vibrating device is placed on the patient's back, which loosens the mucus through the vibrations and thus also supports coughing.
In addition to therapy, it is important that children drink plenty of fluids to compensate for the loss of fluids caused by coughing and fever, and that they take care of themselves.
Pneumonia in Children: Prognosis
There is no uniform prognosis for pneumonia in children. The individual healing process and the duration of the illness depend on the type of pathogen and the general health of the child. If the child has no other illnesses, the prognosis is usually good and the pneumonia usually heals within seven to ten days. After a pneumonia, however, children are sometimes prone to infections of the respiratory tract for weeks. Therefore, you should take it easy for at least a month even after you have overcome pneumonia.
Pneumonia in children: complications
Complications of pneumonia in children are rare. They often arise when the antibiotic therapy prescribed by the doctor is not followed. This can prolong the duration of pneumonia or the pathogens can spread to the rest of the body. If the pathogen gets from the lungs to other organ systems, the following complications are possible:
- Pleurisy (pleurisy)
- Fluid build-up in the pleural space (pleural effusion)
- Blood poisoning when the bacteria enter the bloodstream (sepsis)
- Meningitis
- Collection of pus (abscess) in the lungs
Take your child to the doctor immediately if their symptoms worsen or if their condition has not improved significantly after three days - despite antibiotic therapy!
Pneumonia in children: prevention
You cannot prevent pneumonia in children in general because there are too many different causes. However, with certain vaccinations you can protect your child from infection with certain common pathogens that cause pneumonia. The Standing Vaccination Commission (StiKo) at the Robert Koch Institute (RKI) recommends the following vaccinations for all children, which can prevent pneumonia, among other things:
- Measles vaccination (only available as a combined MMR vaccine - effective against measles, mumps and rubella)
- Haemophilus influenzae type b vaccination (Hib vaccination)
- Pneumococcal vaccination
- Chickenpox vaccination (also available as a quadruple vaccine MMRV vaccination - effective against measles, mumps, rubella and chickenpox = varicella)
The best preventive measure against pneumonia in children is also a healthy lifestyle. Make sure that your offspring have a balanced diet and exercise regularly. If your child has an underlying disease or a weakened immune system, you have to be more careful that they do not play with friends who are sick - pneumonia could possibly be life-threatening for your child!
To prevent complications, existing pneumonia in children should also be completely cured before the offspring go back to kindergarten or school.
Tags: eyes organ systems palliative medicine