Radioiodine therapy
Markus Fichtl is a freelance writer in the medical department.
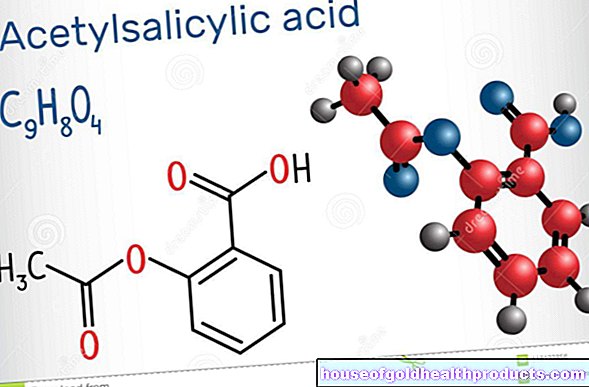
More about the experts All content is checked by medical journalists.Radioiodine therapy is the local irradiation of the thyroid with radioactive iodine molecules. It is often used for thyroid cancer and pathological overactivity of the thyroid gland. Here one takes advantage of the fact that the thyroid gland is an “iodine catcher”: it stores almost all of the iodine that the body absorbs. Read everything about the therapy procedure, when it is carried out and what the risks are.

What is radioiodine therapy?
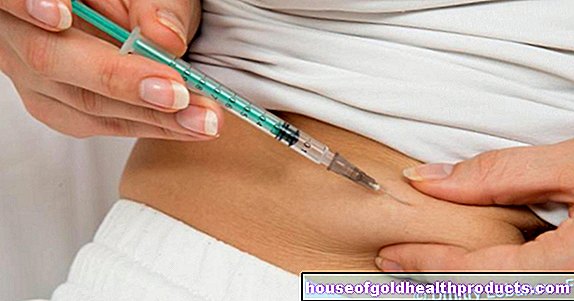
Radioiodine therapy is the most common form of nuclear medicine therapy. During the procedure, the patient swallows radioactive iodine in the form of sodium iodide - either as an aqueous solution or in capsule form. It is then transported via the bloodstream to the thyroid gland, which absorbs and stores the iodine very quickly. After the iodine has reached the pathologically altered thyroid cells, its radioactivity can damage the pathologically altered cells from the inside out and ultimately destroy them.
Why does the thyroid store iodine at all?
The butterfly-shaped thyroid under the larynx is an important organ for the human hormonal balance. It produces hormones (called T3 and T4) from iodine normally ingested through food, which have an activating effect on the body's energy metabolism. The activity of the thyroid gland is controlled by the pituitary gland, which, depending on the need for thyroid hormones, releases more or less of the stimulating messenger substance TSH to the thyroid gland.
When is radioiodine therapy carried out?
In certain diseases, the control of thyroid hormone production by the pituitary gland can be disturbed. The thyroid then produces the hormones "autonomously", i.e. independent of the body's needs and the control signals from the pituitary gland. It produces more hormones than are needed and can grow uncontrollably in the process.
Radioiodine therapy is carried out:
- as follow-up treatment for thyroid cancer and its metastases (only for differentiated thyroid carcinoma)
- for benign thyroid nodules that release hormones in an uncontrolled manner (thyroid adenomas)
- in inflammatory immune diseases (Graves disease)
- with goiter formation. The goiter usually has no effect on the metabolism, but due to the strong growth of the thyroid tissue it is an aesthetic problem and can lead to swallowing difficulties.
With radioiodine therapy, the diseased thyroid tissue can be removed very safely and with little risk. Prior surgery is not necessary, except for follow-up treatment for thyroid cancer. In this type of cancer, radioiodine therapy is used to treat the thyroid gland or remnants of the thyroid gland and any daughter tumors (metastases) that may be present.
What do you do with radioiodine therapy?
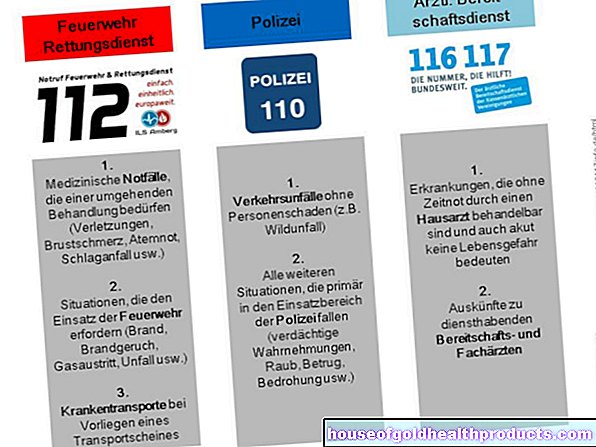
The course and goal of the therapy are always the same regardless of the underlying disease: The patient is admitted to the hospital, because although the radiation from the iodine used only reaches a few millimeters, there is theoretically the possibility of harming other people. This is because the radioactive decay of the iodine used not only releases the therapeutic so-called beta radiation, but also a small proportion of gamma radiation, which has a far greater range. Therefore, the patient is not allowed to receive a visit for the duration of radioiodine therapy and the waste water from the toilet, shower and other service water is collected in special systems until the radiation has subsided.
On the first day of your stay in the clinic, there will be an informative discussion, an ultrasound examination of the thyroid gland and a final determination of the relevant laboratory values. A scintigraphy was often carried out beforehand in order to determine the metabolic activity of various tissues in the body.
A so-called radioiodine test is then carried out with a test capsule to determine how active the thyroid is. The patient then swallows the therapy capsule or liquid with the radioactive iodine.
From this point onwards, an inpatient stay of at least 48 hours is required by law, and the daily residual radiation from the thyroid must not exceed a certain maximum value. Therefore, it can sometimes be necessary to spend several weeks in the clinic. This period of time varies from person to person. On the other hand, there is the prospect of the very high chances of recovery of 90 percent and the low side effects of radioiodine therapy. After discharge, the patient can immediately resume their normal everyday life and also go to work.
What are the risks of radioiodine therapy?
Like almost any therapy, radioiodine therapy has side effects. Early side effects up to 14 days after the end of treatment are temporary changes in the blood count or painful swelling and inflammation of the thyroid gland in up to 70 percent of treatments (10 to 40 percent).
With a higher dose of radio iodine after tumor treatment, the radiation exposure of the salivary glands can lead to dry mouth for a short time. Salivary glands or stomach can also become inflamed in about a third of cases. Many tumor patients also have problems with permanently dry eyes during the course of treatment. In the long term, the effects of radiation can cause serious side effects such as leukemia (less than one percent of treatments) or damage to the bone marrow (very rarely!).
To protect the child, radioiodine therapy must not be carried out during pregnancy and breastfeeding. In addition, contraception should be used for six to twelve months afterwards.
Some of the patients develop an underactive thyroid after radioiodine therapy. However, this is not dangerous, as the missing hormones can be replaced easily and without side effects with thyroid hormones in tablet form.
What do I have to consider before and after radioiodine therapy?
Thyroid hormones, drugs containing iodine, or contrast media must not be taken four weeks before radioiodine therapy. The reason for this is that the messenger substance from the pituitary gland, which stimulates the thyroid gland to absorb iodine (the TSH), only circulates in the blood in the highest possible concentration and the thyroid gland thus absorbs the maximum amount of radioactive iodine.
Pregnancy must be ruled out at the time of treatment.
Aftercare
The success of the radioiodine therapy is checked after three to six months by means of a full-body scintigraphy. Sometimes it may be necessary to do a second radioiodine therapy. If the laboratory check shows signs of hypothyroidism after the therapy, it may be necessary to take thyroid hormones in tablet form.
Tags: menshealth gpp parasites