Mastoiditis
Sophie Matzik is a freelance writer for the medical team.
More about the experts All content is checked by medical journalists.Mastoiditis is a purulent inflammation of the bone behind the ear. Mastoiditis usually develops as a result of an otitis media that has not been treated or has been treated too briefly. Inflammation is triggered by different types of bacteria. With timely and consistent treatment, mastoiditis has a good prognosis. However, if left untreated, complications can arise that can be life-threatening. Read everything you need to know about mastoiditis here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. H70
Mastoiditis: description
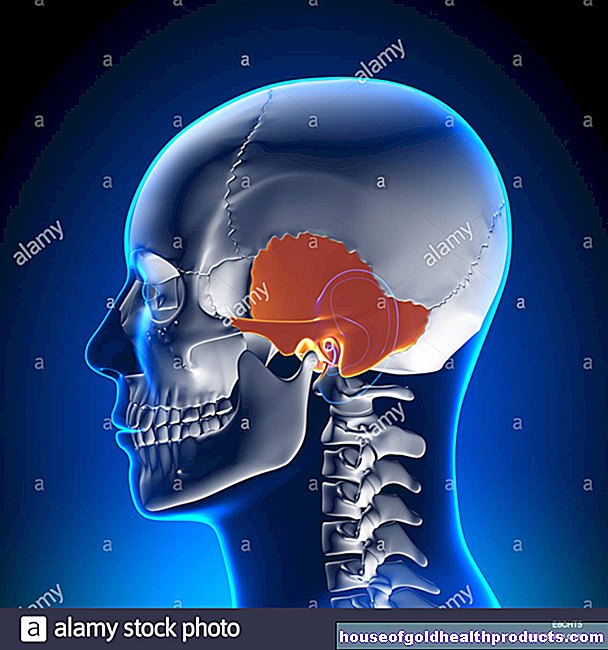
Mastoiditis (also called mastoid inflammation) is a purulent inflammation of the boil that is behind the ear. This bone (medically referred to as mastoid bone) has an elongated, pointed shape that is vaguely reminiscent of a wart, hence the name of the mastoid process (pars mastoidea). The interior of the mastoid process is not completely filled with bone mass; its interior is partially filled with cavities lined with mucous membrane cells. In mastoiditis, there is inflammation here.
The mastoid process lies behind the ear, behind there it can be felt as a bulge. It is directly connected to the tympanic cavity (Cavum tympani). The tympanic cavity is the part of the middle ear where the ossicles are located. If inflammation occurs there, it is known as "otitis media". Due to the close spatial proximity, mastoiditis is usually always a secondary disease or complication of otitis media.
Mastoiditis is the most common complication of otitis media today. Middle ear infections mainly affect children and adolescents, while adults are less likely to get the disease. This is why mastoiditis occurs more frequently in childhood. Nevertheless, due to the good treatability of otitis media, it is a rare disease. 1.2 to 1.4 children in 100,000 children are considered to be affected by this complication.
Chronic mastoiditis
Chronic mastoiditis must be differentiated from acute mastoiditis. Chronic mastoiditis is a little less common than acute mastoiditis, but it is more dangerous. In chronic mastoiditis, the mastoid process also becomes inflamed. However, this inflammation is not noticeable through the symptoms (such as fever or pain) that are classically associated with mastoiditis. Because of this, it can go undetected for weeks and even months. Doctors therefore also call this form masked mastoiditis. If chronic mastoiditis persists over a long period of time, the bacteria continue to multiply. They also have plenty of time to spread further in the body and affect other areas. It is not uncommon for chronic mastoiditis to result in considerable consequential damage.
Mastoiditis: symptoms
Symptoms of mastoiditis appear around two to four weeks after an acute otitis media starts. Most of the time, their symptoms have subsided and then suddenly flare up again. Mastoiditis may be the cause.
In general, the symptoms of mastoiditis are similar to those of otitis media. It is therefore very difficult for a layperson to differentiate between the two diseases. Either way, they should be treated as quickly as possible. In general, therefore, a doctor should be consulted as a precaution if one or more of the following symptoms occur:
- Pain in and around the ear. A constant, throbbing pain is typical.
- Prolonged fever
- Hearing deteriorates
- Restlessness, trouble sleeping, violent screaming
- Exhaustion
In addition, with mastoiditis there is an externally palpable swelling and sensitivity to pressure over the mastoid process, which does not occur with otitis media. If the swelling is severe, it will push the ear down sideways. As a result, the auricle stands out clearly. In addition, large amounts of a milky liquid often drain from the ear. The patient may refuse to eat and appear apathetic.
In young children, it is difficult to determine exactly which symptoms are present. A sign of both otitis media and mastoiditis is when children hold their ears frequently or shake their heads back and forth. Many young children also experience nausea and vomiting. Mastoiditis is often less severe in babies than in older children. Parents should therefore pay close attention to the smallest changes in their child's behavior.
Mastoiditis: causes and risk factors
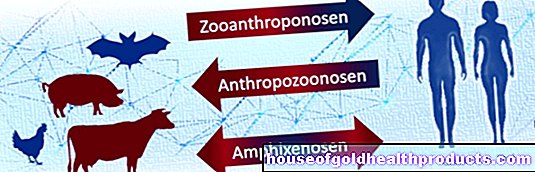
Mastoiditis in babies and children is usually caused by bacteria such as pneumococci, streptococci and Haemophilus influenzae type b, and often staphylococci in babies. Since there is no outside path that leads directly into the mastoid process, mastoiditis is usually a result of other diseases.
In most cases mastoiditis is preceded by a real chain of infection. Children quickly and frequently become infected with various types of virus, which then cause inflammation of the throat and pharynx. The viral infection reduces the body's defenses. This easily creates an additional infection with bacteria (superinfection). Bacteria can get from the pharynx through the Eustachian tube (which connects the pharynx and middle ear) directly into the middle ear and also trigger inflammation here. Mastoiditis often develops as a result of an otitis media that is not treated or treated too late. Even if an otitis media is treated too briefly, bacteria can spread from the middle ear into the mastoid process.
Difficult drainage of secretions in the case of infections promotes mastoiditis. This happens, for example, with a severely swollen nose or blocked ears. A weakened immune system also promotes infections. A weakening of the immune defense occurs, for example, in the context of therapy with antibiotics or corticosteroids (e.g. cortisone) and in certain chronic diseases (e.g. HIV or diabetes mellitus).
Mastoiditis: examinations and diagnosis
If mastoiditis is suspected, an ear, nose and throat doctor is the right person to talk to. In a first conversation, he will record the medical history (anamnesis). You have the opportunity to describe your complaints in detail. In the case of children, the parents usually provide information. The doctor can ask questions such as:
- Have you (or your child) had an infection recently?
- How long have the complaints existed?
- Have you noticed any discharge from your ear?
A physical examination follows the anamnesis. The doctor first looks for external changes. For example, he can detect redness as well as pain and tenderness above or behind the ear. With the help of an ear mirror (otoscope), the eardrum and the internal auditory canal are examined. This examination is also called an otoscopy. If there is a swelling of the eardrum, this is determined, among other things, by a light reflex that is located in a different place on the eardrum than in a healthy ear. In addition, the inside of the ear is red.
Further diagnosis is made in a hospital if there is a reasonable suspicion of mastoiditis. This makes sense because the therapy should start as quickly as possible and an operative intervention may be necessary under certain circumstances. If the doctor has not done this yet, a blood count will be done first. If there is inflammation in the body, certain blood test values are increased. These include the number of white blood cells (leukocytes), the value of the C-reactive protein and the rate of sedimentation of the blood cells. To determine the causative agents of the inflammation, a smear is taken from the ear. A culture is created from this in the laboratory. The result is available within one to two weeks. As a rule, mastoiditis therapy is started before the final result is available.
The diagnosis is further confirmed with the help of an X-ray image or computer tomography. The doctor can identify possible complications on the resulting images - for example, if pus has accumulated in surrounding areas. Getting an x-ray and computed tomography scan can be difficult for young children. If there are clear findings that substantiate the suspicion of mastoiditis, doctors in some cases dispense with these additional examinations.
Mastoiditis: treatment
Mastoiditis, like other bacterial infections, is treated with antibiotics. Depending on which pathogen is responsible for mastoiditis, different antibiotics are particularly effective. If the exact pathogen has not (yet) been determined, in most cases a broad spectrum antibiotic, an active ingredient from the group of penicillins, is used. They work against a large number of different bacteria, but are particularly effective against staphylococci and streptococci, the most common pathogens causing mastoiditis.
The easiest way to give antibiotics to babies and young children is through the vein (infusion). This ensures that the medication actually ends up in the bloodstream and is not spit out again. In adolescents and adults, antibiotics are given in the form of tablets. In addition, pain relievers may be prescribed to relieve earache.
Mastoiditis - when is surgery necessary?
If the mastoiditis is very pronounced or if there is no improvement even after a few days of treatment, the swelling must be surgically removed. To do this, the inflamed areas of the mastoid process are removed (mastoidectomy). There are two methods of surgery to choose from, simple and radical mastoidectomy. With a simple mastoidectomy, only the inflammation-affected cells of the mastoid process are removed. With radical mastoidectomy, on the other hand, additional structures are removed. These include the back wall of the external auditory canal and the upper part of the tympanic cavity of the middle ear. This massive intervention creates a large cavity between the mastoid process and the external auditory canal. This cavity makes it easier to monitor and maintain the ear and mastoid spaces. Radical mastoidectomy is indicated for mastoiditis that is associated with excessive pus formation and accumulation.
During the operation, a thin tube (drainage) through which the pus is drained is placed so that the fluid (mostly pus) can escape from the ear. The operation is always carried out as an inpatient. A small incision is made behind the ear through which the operation is performed. The cut heals quickly. After an operation, those affected have to stay in the hospital for about a week. After that, however, they are usually symptom-free. During the operation, antibiotics are given to kill any bacteria that may still be in the body.
Mastoiditis: disease course and prognosis
The prognosis for mastoiditis depends on when the infection is detected. In order to avoid secondary diseases, mastoiditis should be treated as soon as possible. The later the therapy begins, the more time the bacteria have to spread in the body and the more likely complications are to arise.
If therapy starts in good time, complications of mastoiditis can usually be avoided. With consistent treatment, mastoiditis heals within a few days to weeks. Meanwhile, the symptoms decrease. Permanent damage such as hearing loss then rarely occurs.
Mastoiditis complications
If mastoiditis is left untreated, however, serious complications can result. If the accumulation of pus cannot flow outwards, it looks for alternatives around the mastoid process. This can lead to an encapsulated accumulation of pus below the mastoid in the periosteum. In addition, pus can penetrate between the bones and the outermost meninges (epidural abscess). However, the pus can also penetrate the side muscles of the neck and neck (Bezold abscess). An encapsulated accumulation of pus in the brain (brain abscess) is particularly dangerous, as it can move and thus pinch or squeeze different structures in the brain.
The bacteria can also spread further in the body from the mastoid process. It is particularly dangerous if they spread to the meninges (meningitis) or the inner ear (labyrinthitis). If the bacteria get into the bloodstream, blood poisoning (sepsis) occurs. The facial nerve, which is responsible, among other things, for the facial muscles, runs near the mastoid. If this is damaged, permanent numbness and facial paralysis can occur. In extreme cases, mastoiditis can take on such a life-threatening course!
It is not possible to specifically prevent mastoiditis. However, you can reduce the risk of illness by trying to prevent infections and inflammation in general. To do this, strengthen your or your child's defenses by eating a balanced diet and exercising a lot in the fresh air.
It is important that you have an otitis media treated immediately. In doing so, you should absolutely follow the doctor's instructions. If you do not take the antibiotic regularly or for too little time, some bacteria may survive in the ear and multiply again after you stop taking the antibiotic. If the symptoms of otitis media have not subsided after two weeks, if they increase despite treatment or if they recur after a while, you should consult a doctor again and thus reduce the risk of mastoiditis.
Tags: magazine parasites prevention



.jpg)