EHEC
Florian Tiefenböck studied human medicine at the LMU Munich. In March 2014, he joined as a student and has supported the editorial team with medical articles ever since. After receiving his medical license and practical work in internal medicine at the University Hospital Augsburg, he has been a permanent member of the team since December 2019 and, among other things, ensures the medical quality of the tools.
More posts by Florian Tiefenböck All content is checked by medical journalists.EHEC (enterohaemorrhagic Escherichia coli) are certain strains of the intestinal bacterium Escherichia coli. As a rule, an EHEC infection has few symptoms with watery diarrhea, nausea and abdominal pain. In rare cases, however, the disease can take a life-threatening course if bloody bowel inflammation (hemorrhagic colitis) or hemolytic uremic syndrome (HUS) develops. Find out everything you need to know about EHEC here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. D59A04

EHEC: description
The abbreviation EHEC stands for Enterohaemorrhagic Escherichia coli. These are certain bacterial strains of the bacterial species Escherichia coli (E.coli). The EHEC bacteria are sometimes mistakenly called the EHEC virus.
Occurrence and frequency
EHEC diseases occur all over the world. Infants under five years of age are most commonly affected, but EHEC infection can occur in all age groups. According to the Robert Koch Institute (RKI), 30 percent of all EHEC cases in Germany in 2013 concerned children in the age group under five. A total of 1621 cases were reported to the RKI in the same year. The consequences of the EHEC infection resulted in death in two patients. According to the Robert Koch Institute, the fact that the number of new EHEC cases reported was the second highest in 2013 (highest: EHEC 2011) is most likely due to the increased attention of patients and doctors after the EHEC epidemic in Germany in 2011 and others Countries.
EHEC epidemic 2011
The year 2011 is a special case. There were increased reports of EHEC outbreaks. A previously unknown EHEC strain caused extremely serious illnesses from the beginning of May 2011, especially in adult women in northern Germany. In some of those affected, the severe complication of an EHEC infection, the HUS (hemolytic uremic syndrome), occurred. A total of 4908 EHEC infections were reported, over five times as many cases as in 2010 (according to RKI: 918). While in the years before, almost 50 percent of cases were mainly affected by small children, in 2011 this age group made up only 14 percent of all EHEC infections. 21 cases were fatal.
EHEC: symptoms
In adults in particular, EHEC often proceeds without any signs. There are usually no other EHEC symptoms. The bacteria are excreted in the stool after one to three weeks and can be passed on to other people if hygiene is poor. If symptoms arise as part of the EHEC infection, the patient is usually nauseous. They complain of watery diarrhea, have abdominal cramps and vomit. In rare cases, a mild fever is also one of the EHEC symptoms. In rare cases, the EHEC infection is very serious. The following symptoms can occur:
Severe inflammation of the bowel (hemorrhagic colitis)
A severe clinical picture develops in 10 to 20 percent of EHEC infections. Older people, infants and people with weakened immune systems are particularly often affected. EHEC bacteria cause severe intestinal inflammation. The patients have very painful abdominal cramps and bloody diarrhea. Fever may also occur. Doctors refer to this clinical picture as hemorrhagic colitis, which translates as bleeding colon inflammation.
Anemia and kidney weakness (haemolytic uremic syndrome)
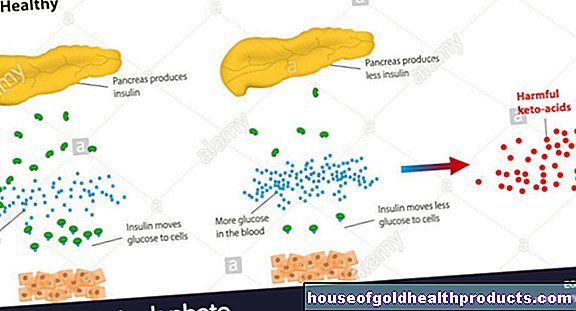
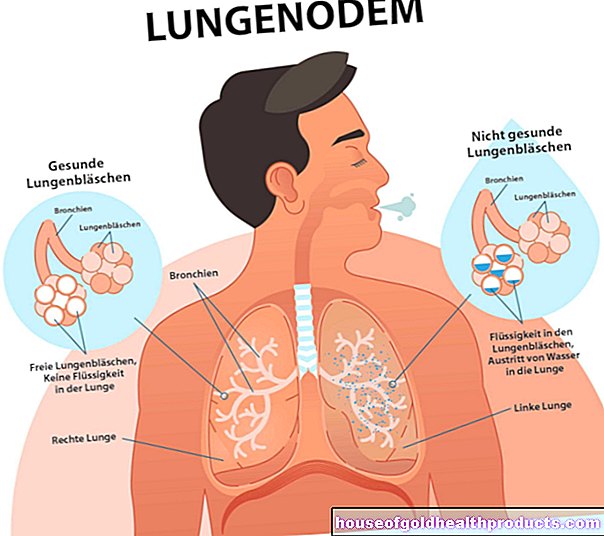
The dangerous haemolytic uremic syndrome (HUS) can also occur as part of an EHEC infection: EHEC toxins destroy red blood cells (haemolysis) and lead to anemia. The patients therefore feel weak and are noticeably pale. In addition, the blood vessel walls and the blood platelets (thrombocytes) are damaged by the bacterial toxins. This leads to a strong tendency to bleed.
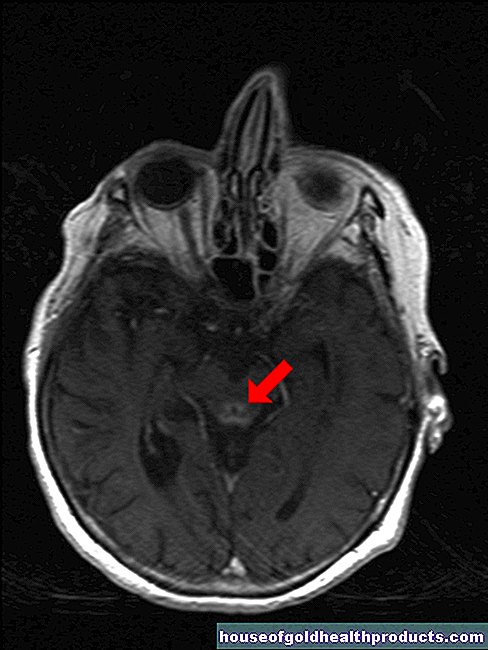
As a result, bleeding occurs, which can be seen in the skin as pin-head-sized, punctiform hemorrhages ("petechiae"). In addition, the kidneys and thus the excretion of fluids no longer function properly. As a result, those affected store water mainly on the legs (edema). The kidneys may fail completely (acute kidney failure). As a result, the detoxification of the blood is restricted. Confusion or seizures may occur.
EHEC: causes and risk factors
EHEC infections are caused by special strains of the bacterium Escherichia coli (E.coli). Millions of E. coli bacteria are part of the normal intestinal flora of humans and animals. There they perform important tasks: they break down indigestible nutrients and ward off pathogens. However, EHEC are strains of these bacteria that can make people sick. Sometimes they are mistakenly called the EHEC virus, even though they are bacteria.
Contagion with EHEC
EHEC bacteria are normally found in the intestines of ruminants such as cattle, sheep or goats. They are excreted in the faeces. Infection mostly occurs through food that is contaminated with manure (liquid animal droppings that are used to fertilize fields). In small children, direct contact with animals also carries the risk of disease.
The risk of EHEC infection is also increased if you consume certain foods, for example unpasteurized milk or raw meat. In the summer of 2011 there were increased EHEC cases. The exact source of the infection could not be found out. However, researchers speculate that green leafy vegetables eaten raw, such as sprouts or spinach, were responsible for the outbreaks.
EHEC can also be transmitted via contaminated water, for example if you drink it or bathe in it. In order to become infected with EHEC, only a very small number (around 100) of bacteria is necessary. This is precisely why transmission from person to person is more common than with other diseases. Here, too, the pathogens are found in the stool and spread to the next person through smear infection and poor hygiene. The time between infection and the first symptoms of the disease (EHEC incubation period) is two to ten, but mostly three to four days.
Why are EHEC dangerous for humans?
EHEC form toxins, so-called Shiga toxins (Stx), which ultimately trigger the EHEC symptoms. To date, researchers have discovered numerous subgroups (serotypes) of EHEC. These can cause various symptoms in humans, from mild gastrointestinal complaints to severe intestinal inflammation. The EHEC serotype O157: H7 is found most frequently worldwide (O and H stand for special surface structures of the respective E. coli strain). The serotypes O103 and O26 follow.
Mode of action of the EHEC poisons
The formed shiga toxins, also called verotoxins, bind to human cells, especially to the blood vessel walls of humans. There they block the build-up of important proteins and the affected cells die. In addition, some EHEC strains can “inject” harmful proteins into body cells. This mechanism enables the pathogens to adhere closely to cells in the intestine.
There are two skin groups of poisonous Shigatoxins, Shigatoxin 1 (Stx1) and Shigatoxin 2 (Stx2). The Stx1 group mainly triggers diarrhea. EHEC, which form Stx2, mainly cause serious diseases such as haemolytic uremic syndrome (HUS). This also explains why EHEC triggered such a severe epidemic in Germany in 2011. Because the newly discovered EHEC serotype O104: H4 forms both Shiga toxins 1 and 2. This makes this strain particularly aggressive.
EHEC: diagnosis and investigation
If the person has diarrhea, they have bowel movements more than three times a day. The stool is not shaped and has a high water content (> 75 percent) - it is therefore liquid. Usually the amount of stool is increased due to the high fluid content (> 250 grams per day). If a patient with this condition presents to a practice, the doctor will carry out some examinations regardless of age. The right person to contact if you suspect an EHEC infection is initially your family doctor. In the case of pronounced complaints (severe diarrhea, poor general condition), a hospital with an infection department should be visited directly.
Medical history and physical examination
First, the doctor asks a few questions (anamnesis) in order to be able to uncover possible additional EHEC signs: How often do you have a bowel movement? How is the chair shaped? Is there blood in the stool? Questions about fever, abdominal pain and urine frequency or appearance are just as crucial. Blood in the urine is a potential indicator of damaged kidneys.
The doctor will also inquire about possible risk factors. This tries to track down a source of infection with EHEC. Was there contact with animals on a farm? Was unwashed vegetables or raw meat eaten? Have you had contact with people with diarrhea, for example at work?
Another important piece of information is the job of the person concerned. If he works with food, this may explain and contain the spread of EHEC infections. It also takes into account which medications are being taken. In particular, excessive use of laxatives can lead to severe diarrhea and simulate an infection.
During the physical exam, the doctor looks for signs of kidney weakness or kidney damage, such as edema or blood in the urine. If the patient feels weak and is unusually pale, these may be signs of anemia. The skin is also thoroughly examined by the doctor. Smaller hemorrhages (petechiae) indicate impaired blood clotting.
If bloody diarrhea shows signs of impaired kidney function, poor blood clotting or anemia, the patient is immediately admitted to a hospital and isolated from other patients. Further examinations are then carried out there.
Investigations of stool samples
There are a number of different causes of diarrhea. The doctor can try to find the cause with a stool sample. With EHEC, patients usually suffer from diarrhea without blood, but otherwise show no health restrictions. However, in a stool sample, EHEC can sometimes detect hidden (occult) blood in the stool.
In certain situations, the doctor will arrange a special stool test for EHEC. According to the valid EHEC 2011 guidelines of the German Society for General Medicine, this applies if
- the patient has diarrhea and blood is visible in the stool
- the patient works directly with food
- the person concerned had contact with HUS sufferers
- Children suffer from kidney failure
Blood and urine tests
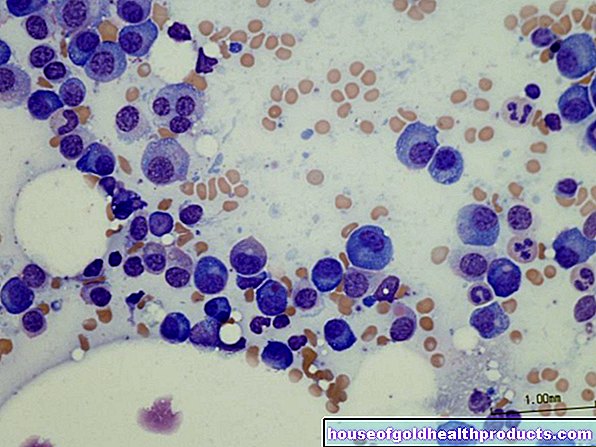
When examining the blood, particular attention is paid to those values that speak for an EHEC-related haemolytic uremic syndrome (HUS). This is mainly the number of red blood cells and platelets. Both the red blood cells and the blood platelets can be significantly reduced because they are destroyed by the toxins of the EHEC.
Changes in kidney values in the blood (for example creatinine) indicate a possible impairment of the kidney due to the EHEC infection. In addition, the inflammation parameters (white blood cells, C-reactive protein) in the blood are determined. However, increased inflammation values only indicate an infection; they are not proof of EHEC. When examining the urine (with a so-called urine stix), doctors first and foremost look for hidden blood and proteins. These can be detected in the case of a functional disorder of the kidneys.
Evidence of EHEC poisons
If an EHEC infection is suspected, the most important thing is to examine whether the bacteria have the genes necessary for poison production (toxin production) (toxin gene detection) and whether they actually produce the toxins (toxin detection). The toxin genes are detected with a PCR test (polymerase chain reaction) from stool material. For the toxin detection, the E. coli obtained from the patient material are first propagated in a culture. In this culture, the Shiga toxins can be detected with a so-called ELISA (Enzyme Linked Immunosorbent Assay).
EHEC: treatment
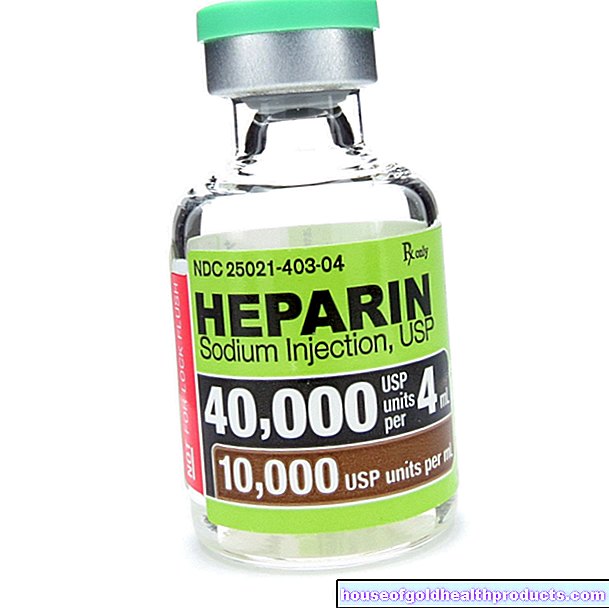
Although EHEC are bacteria (there is no EHEC virus!) Treatment with antibiotics is currently not recommended, as such treatment could prolong the excretion of bacteria and lead to an increased release of toxins by the bacteria. However, recent research suggests that high-dose antibiotic therapy may still be of benefit. However, this has to be verified by further studies. The diarrhea must also not be treated with diarrhea medication such as loperamide, as these also prevent the pathogens from being excreted in the stool.
The EHEC therapy is therefore usually purely symptomatic. Which measures are necessary for this depends on the severity of the disease. As a rule, a fluid and salt substitute is necessary: Patients lose salts (electrolytes) such as potassium and sodium through the diarrhea. These play an important role in the functioning of the heart, nerves and muscles, for example.
A disturbed kidney function also affects the electrolyte level in the body. Therefore, electrolyte losses are compensated for by infusions, tablets or electrolyte powder. The same applies to the fluid balance of the patient, since the patients lose excessive amounts of water through diarrhea.
Treatment of the HU syndrome
Since the complication of hemolytic uremic syndrome (HUS) can be life-threatening, purely symptomatic treatment is not sufficient. The weakened kidney function is stimulated with special drugs (diuretics). If the kidneys fail completely, a kidney replacement procedure such as dialysis ("blood washing") is necessary. The blood is cleaned of waste materials via dialysis. If necessary, the patient's blood plasma is also cleaned with what is known as plasma apheresis, similar to dialysis.
In addition, there are other treatment measures, but no long-term studies have yet been carried out on their effectiveness and tolerability. In 2011, the medical journal “The New England Journal of Medicine” presented a study in which, among others, German experts were also involved. According to the results of the study, the treatment of HUS by EHEC with a special active ingredient called eculizumab is promising. With annual therapy costs of around 400,000 euros, it is one of the most expensive drugs of all and can only be used in specialized treatment centers.
EHEC: disease course and prognosis
As a rule, a simple EHEC infection heals without any consequences. However, complications such as bleeding bowel inflammation or haemolytic uremic syndrome (HUS) can have long-term consequences: Around 50 percent of children who develop HUS subsequently need permanent kidney replacement (dialysis) due to permanent kidney damage. Up to 40 percent develop high blood pressure and chronic kidney failure in the ten to fifteen years after a HUS. In the 2011 epidemic, the death rate was around one percent. Taking previous studies into account, this rate is around two percent. It is increased in a complicated haemolytic uremic syndrome, from which around four percent of people die.
EHEC: prevention
The Robert Koch Institute has issued some recommendations to protect yourself and those around you from an EHEC infection.These recommendations are aimed primarily at young children, the elderly, the immune system and pregnant women:
Be careful with direct animal contact
This applies, for example, to a petting zoo. Be careful not to put your hands in your mouth after contact with the animals. Avoid eating and drinking at the same time. Wash hands thoroughly with soap and warm water.
Store your food well chilled
This is especially true of perishable foods. Because EHEC bacteria multiply best at a temperature of 37 ° Celsius.
Wash your fruit thoroughly and peel it if necessary
EHEC can be found on vegetables and fruit if animal manure (manure) has been used as fertilizer.
Do not eat vegetables raw or peel them
As with the preparation of meat, care should be taken to heat the food to at least 70 ° Celsius for ten minutes.
Do not consume raw animal products
Refrain from consuming raw or insufficiently heated meat. The same applies to raw milk and products made from it. EHEC and its toxins are only rendered harmless in well-heated animal products.
Make sure the cooking environment is clean
After preparing raw food, thoroughly clean dishes, cutlery, work surfaces, towels, and cutting boards. In this way, the EHEC bacteria cannot be transferred to the next prepared food.
Wash your hands thoroughly with soap and warm water
This is especially true after using the toilet, after working with raw foods, and before you eat or drink.
Go to the doctor in time
This is especially true if diarrhea persists for several days or if you find blood in your stool. A doctor should be consulted quickly, especially in the case of infants and small children, if diarrhea occurs frequently throughout the day.
Preventing the spread
In order to prevent the spread of EHEC, thorough hygiene measures are of enormous importance. This can also successfully contain the transmission from person to person. If patients are treated as inpatients in a hospital, they are cared for in isolation there. Only when the EHEC bacteria are no longer detectable after three stool samples is the isolation canceled. Infected people who work in community facilities such as schools are not allowed to work there as long as they excrete EHEC. The same applies to people who work with food. By making infections notifiable even if they are suspected, attempts are made to identify and contain the spread of EHEC at an early stage.
Tags: drugs teenager book tip


.jpg)










.jpg)