Plasmacytoma
Dr. med. Julia Schwarz is a freelance writer in the medical department.
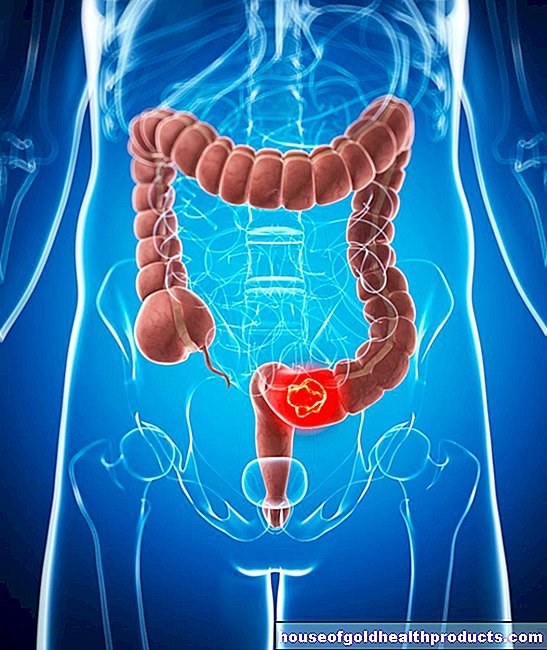
More about the experts All content is checked by medical journalists.Plasmacytoma (multiple myeloma) is a type of blood cancer that affects the bone marrow. Altered white blood cells are formed, which affects the immune system. Plasmacytoma is rather rare, but it is the most common cancer of the bone marrow. Men are affected more frequently than women. Read more about the causes and treatment options for plasmacytoma, life expectancy and the course of the disease here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. C90
Plasmacytoma: description
A plasmacytoma is a special form of blood cancer in which so-called plasma cells in the bone marrow multiply in an uncontrolled manner. Other names for plasmacytoma are "Kahler's disease" and "multiple myeloma". Strictly speaking, multiple myeloma describes a diffuse distribution of proliferating plasma cells in the bone marrow. The plasmacytoma, on the other hand, shows a locally limited (solitary) proliferation of plasma cells.
The blood cancer classification system is complicated. The plasmacytoma is classified in the group of lymphomas (so-called B-cell non-Hodgkin lymphomas).
Degenerate plasma cells
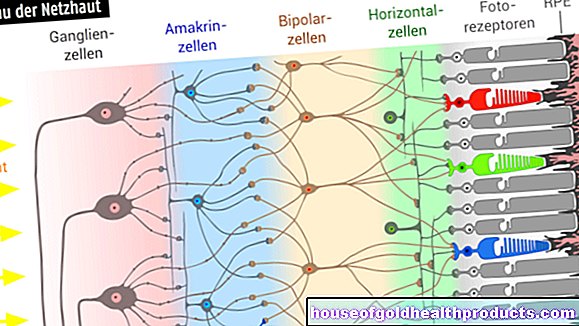
Red and white blood cells are produced in the bone marrow. While the red blood cells (erythrocytes) are responsible for transporting oxygen in the body, the white blood cells (leukocytes) are formed in the bone marrow for immune defense. There are different subgroups of leukocytes, such as granulocytes, T- or B-cells. Plasma cells represent the most mature stage of the B cells and are responsible for the production of antibodies.
In a plasmacytoma, the plasma cells in the bone marrow grow uncontrollably. They also produce large amounts of abnormal proteins: complete or incomplete modified antibodies of a single type (monoclonal antibodies) called paraproteins. As a result, the immune system is weakened in a plasmacytoma, which makes the patient much more susceptible to infections. Over time, the degenerate plasma cells displace more and more healthy cells in the bone marrow, which can lead to various symptoms.
Plasmacytoma: frequency
Around one in four to five out of 100,000 people in Germany will develop a plasmacytoma. Men are affected more frequently than women. The average age of onset of plasmacytoma is over 45 years.
Plasmacytoma: symptoms
In the beginning, the cancer in the bone marrow usually does not cause any symptoms. Only in the further course can multiple myeloma cause symptoms of various kinds:
Back pain
The first symptoms of a plasmacytoma are usually bone pain. Those affected particularly often complain of back pain. The plasmacytoma breaks down bone tissue (often around the spine). The risk of broken bones (fractures) is therefore increased.
Displacement of red blood cells
In a plasmacytoma, altered plasma cells proliferate in the bone marrow. This displaces other important blood cells in their growth. As a result, too few red blood cells are produced and anemia develops. The symptoms of anemia are based on the resulting lack of oxygen in the tissue: pale skin color, feeling weak, dizzy and tired.
Lack of antibodies
If the healthy white blood cells are also displaced, sufficient intact antibodies can no longer be produced. The immune system is weakened by the plasmacytoma, and infections with bacteria or viruses are more likely to occur.
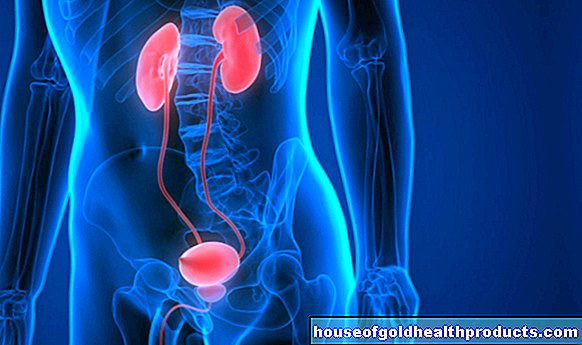
Kidney damage
Some of the paraproteins produced by the plasmacytoma are excreted through the kidneys. However, these so-called Bence Jones proteins can also establish themselves in kidney tissue and damage it. Some patients subsequently report foamy urine.
Small skin bleeding
The formation of blood platelets (thrombocytes) is also impaired by a plasmacytoma. The platelets are usually responsible for blood clotting. As a result, small, pinhead-sized bleeding in the skin (petechiae) is more common.
Plasmacytoma: causes and risk factors
The starting point for a plasmacytoma is a degenerate plasma cell that multiplies exponentially. Plasma cells are part of the B lymphocytes, a subgroup of white blood cells. Their most important task is the production of antibodies. However, degenerate plasma cells produce modified antibodies (paraproteins).
How plasma cells degenerate in plasmacytoma has not yet been fully clarified. Scientists were able to determine a genetic change in 15 percent of those affected. Chromosomes 13 and 14 showed an increased number of defects. The influence of ionizing radiation and pesticides on the development of plasmacytomas is currently also being investigated.
The plasmacytoma ensures the formation of a large number of new blood vessels in the bone marrow so that it is optimally supplied with nutrients and can grow.
Plasmacytoma: examinations and diagnosis
Patients should seek medical advice for any symptoms that may suggest a plasmacytoma. He can use various examinations to determine whether multiple myeloma is actually present.
Blood and urine test
A blood test is a quick and inexpensive way to get the first signs of a plasmacytoma. The degenerated antibodies can be detected in the blood by means of an increased protein level. The protein level correlates with the plasmacytoma activity: the more degenerate proteins are present, the more advanced the plasmacytoma.
A blood count shows the percentage of different blood cells. This shows how much the plasmacytoma has already displaced healthy cells and whether there is already anemia. A blood count can also help identify changes in kidney values when Bence Jones proteins damage kidney tissue and kidney function deteriorates as a result.
If the bones are affected by the plasmacytoma, increased calcium values can be found in the blood count: the bone consists to a large extent of calcium. If the plasmacytoma accelerates bone breakdown, the released calcium is distributed in the blood and can be measured.
The Bence Jones proteins, also degenerate proteins from the plasma cells, can be detected in the urine of the patient.
Bone marrow aspiration
If a plasmacytoma is suspected, a bone marrow aspiration can be performed. Usually the iliac crest is pierced with a needle to pull out some bone marrow. The bone marrow sample is then examined under the microscope. In healthy people, the proportion of plasma cells is usually a maximum of five percent. In contrast, plasmacytoma patients often have values of over ten percent. The degenerated cells can be examined in more detail by determining the rate of division or looking for possible chromosome changes.
Imaging procedures
If the plasmacytoma has led to bone loss, this can be demonstrated in the X-ray image.You can see small holes (osteolytic foci) in the skull, in the ribs, in the vertebral bodies or in the pelvic bones.
Computed tomography (CT) is another imaging method for plasmacytoma diagnostics. It shows even more precisely to what extent the skeletal system has already been affected by the plasmacytoma.
If it is suspected that the spinal cord has already been damaged by the breakdown of the vertebral bodies, magnetic resonance imaging (MRI) can also be performed.
Plasmacytoma: treatment
Plasmacytoma therapy depends on the stage of the disease. A distinction is made between three stages of the disease: the higher the stage, the more malignant the plasmacytoma. A precise classification is of great importance in order to be able to create an adequate therapy plan.
If there are no complaints and if the plasmacytoma is stage I, the patient is closely examined and observed (“watch and wait”).
Multiple myeloma: chemotherapy and stem cell transplant
Chemotherapy is started as soon as the plasmacytoma continues to spread. The aim of the therapy is to prevent the degenerated plasma cells from spreading further.
In the case of advanced plasmacytoma in stage II and III, high-dose chemotherapy is carried out. This severely weakens the patient's immune system. Therefore, if possible, what is known as an autologous stem cell transplant is then carried out: the patient's own stem cells - taken before chemotherapy - are re-administered so that the formation of immune and blood cells is quickly restored. For patients under the age of 75, this is the current standard procedure. Patients older than 75 years or patients in a very poor general condition are not suitable for high-dose chemotherapy.
Multiple myeloma: therapy with other drugs
Not every patient can be treated with high-dose chemotherapy and subsequent stem cell transplantation. In addition, this combination treatment does not work in some patients, causing relapses. In both cases, the administration of additional medication can be useful.
High-dose glucocorticoids (dexamethasone, prednisolone) can cause a rapid reduction in tumor mass.
The active ingredient bortezomib is a so-called proteasome inhibitor. It causes cancer cells to die and prevents new blood vessels from forming. Without an adequate blood supply, the plasmacytoma cannot grow any further.
The two active ingredients thalidomide and lenalidomide belong to the group of IMiD (immunomodulatory drugs). They also prevent new blood vessels from growing in the bone marrow and trigger cell death in cancer cells. They also inhibit the release of inflammatory substances.
The substances are used and dosed individually. Other drugs can also be given in combination therapy. A combination of lenalidomide, thalidomide, and bortezomib is often used to prevent relapse.
Supportive therapy
The plasmacytoma can be extremely painful, especially if the bone is affected. The pain can be treated with radiation therapy in addition to chemotherapy. Individual tumor foci are irradiated in order to inhibit cell growth.
So-called bisphosphonates are also given. Bisphosphonates inhibit bone breakdown and have a stabilizing effect on the bones.
Since the immune defense is weakened by the plasmacytoma, particular attention should be paid to protection against infections. A flu vaccination or a vaccination against pneumococci is very useful for many people affected. In addition, the patient should wash their hands more often, especially during the flu season (autumn, winter). There is an increased risk of infection in public transport, kindergartens and schools.
Plasmacytoma: disease course and prognosis
The plasmacytoma can vary greatly in its course and prognosis. The stage of the disease, the age of the patient and any concomitant diseases play a role in this. The aim of treatment is always to extend the life span with the maximum possible quality of life.
Multiple myeloma: prognosis
Complete healing is only possible in very few cases. The plasmacytoma prognosis is much better than it used to be thanks to today's therapeutic options. Before chemotherapy became the standard practice, the mean survival time was around one year. With chemotherapy it is now around five years. The following are considered unfavorable prognosis factors:
- a change in chromosome 13
- a high stage of plasmacytoma
- an old age
In general, however, the following applies to multiple myeloma: Life expectancy in individual cases cannot be precisely predicted. Some patients die after just a few months, other patients still live after ten years.
Multiple myeloma: terminal stage
In the final stage, the plasmacytoma is already very large. Patients often die because the plasmacytoma does not produce enough blood cells in the bone marrow.
Tags: medicinal herbal home remedies parasites alcohol drugs