Pulmonary edema
Astrid Leitner studied veterinary medicine in Vienna. After ten years in veterinary practice and the birth of her daughter, she switched - more by chance - to medical journalism. It quickly became clear that her interest in medical topics and her love of writing were the perfect combination for her. Astrid Leitner lives with daughter, dog and cat in Vienna and Upper Austria.
More about the experts All content is checked by medical journalists.In pulmonary edema, fluid collects in the lung tissue and alveoli. This impairs the exchange of oxygen and the organs are no longer adequately supplied with oxygen. The heart is usually the cause of pulmonary edema. Read here how it develops, what symptoms occur and how it is treated!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. J81

Brief overview
- What is pulmonary edema? With pulmonary edema, fluid collects in the lungs. The "water in the lungs" hinders the exchange of oxygen. Possible consequences are breathing problems up to respiratory arrest.
- Causes: heart disease, kidney failure, toxins, smoke inhalation, severe pneumonia, blood poisoning, allergic shock, altitude sickness, ARDS, SIPE
- Risk factors: previous heart and lung diseases
- Course and prognosis: If left untreated, pulmonary edema leads to respiratory failure. The prognosis with timely treatment is good, depending on the underlying disease.
- Symptoms: Fast and shallow breathing, shortness of breath that worsens when lying down, cough, blue lips, fear of choking
- Treatment: Immediate medical treatment necessary! Dehydrator, antihypertensive, oxygen, upper body elevated, treatment of the underlying disease
- Diagnostics: Typical symptoms, lung x-ray or MRI, heart ultrasound, EKG, blood gas analysis, blood test
- Prevention: No concrete precautionary measures possible, generally healthy lifestyle, treatment of existing underlying diseases, slow ascent to prevent altitude sickness
What is pulmonary edema?
In pulmonary edema (pulmonary edema, water lung), fluid collects in the lungs, which affects the exchange of oxygen. Depending on how pronounced the pulmonary edema is, those affected initially have only mild symptoms up to life-threatening conditions. If left untreated, the so-called "water in the lungs" leads to death.
The term "water in the lungs" is medically incorrect: in fact, the liquid that has accumulated is blood plasma - the liquid component of blood. The plasma emerges from the blood vessels and is pressed into the lung tissue. The reasons for this are different.
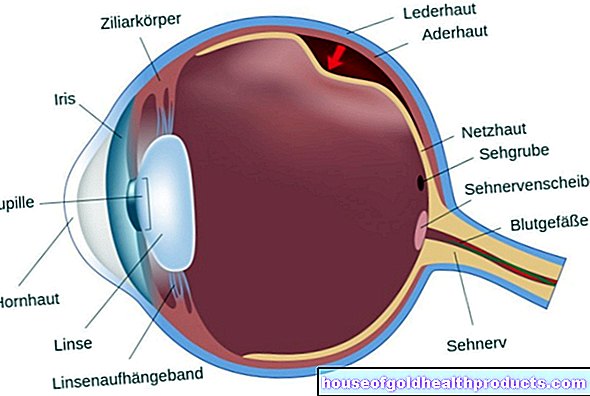
The oxygen exchange takes place in the alveoli: the oxygen reaches the underlying blood vessels through the thin wall of the vesicles. As the blood flows through the body, the oxygen supplies all body tissues and thereby maintains their function.
In pulmonary edema, the fluid collects in the alveoli. The blood plasma that has escaped from the blood vessels wets the inner side of the alveoli, which is otherwise filled with air, and thus hinders the passage of oxygen into the blood. There is shortness of breath and an insufficient supply of oxygen-rich blood to the body. If left untreated, there is a risk of respiratory failure and, as a result, multiple organ failure (several organs lose their function).
Stages of pulmonary edema
Interstitial pulmonary edema: First, the "water" collects in the lung tissue. At this point, the oxygen exchange is only slightly impaired, but the first symptoms such as coughing and shortness of breath may already appear.
Alveolar pulmonary edema: As a result, the fluid from the lung tissue reaches the alveoli, and "alveolar pulmonary edema" develops. The exchange of oxygen in the alveoli is already impaired and the symptoms intensify.
Foam formation: The protein-rich edema fluid mixes with the air in the airways. A "foam" forms which triggers a cough. Affected people sometimes cough out the foam. This is whitish or - mixed with blood - reddish.
Asphyxia: In the end stage of the pulmonary edema, there is a lack of oxygen due to insufficient gas exchange. Medical professionals refer to this condition as asphyxia. If those affected do not receive oxygen now, there is a risk of breathing arrest. The organs no longer receive oxygen and stop functioning. The patients eventually die of multiple organ failure.
How does pulmonary edema develop?
There are several reasons why fluid builds up in the lungs. In pulmonary edema, it is usually not the lungs themselves that are sick. Most often the "water in the lungs" is the result of a heart disease (cardiac pulmonary edema), somewhat less often pulmonary edema has non-cardiac causes.
Cardiac pulmonary edema
Cardiac pulmonary edema is the most common form. Various heart diseases result in the fluid being pressed out of the blood vessels into the lung tissue or into the alveoli.
The most common heart disease that causes pulmonary edema is heart failure (heart failure). In so-called left heart failure, the left ventricle is too weak to pump enough blood into the body. However, since more blood flows from the pulmonary vessels into the heart chamber than it can transport further, the blood backs up in the lungs. This increases the blood pressure in the pulmonary vessels and the blood fluid (plasma) is pressed into the lung tissue. If the water gets into the alveoli, pulmonary edema forms.
Other heart conditions that can lead to pulmonary edema include:
- Heart attack
- Myocarditis
- Cardiac arrhythmias
- Heart valve diseases such as aortic stenosis or mitral valve regurgitation
Non-cardiac pulmonary edema
In non-cardiac pulmonary edema, the cause of the fluid build-up lies outside the heart. The edema arises because the blood vessel walls are no longer sufficiently tight, they become permeable. This causes fluid to leak out and collect in the lungs.
Possible triggers for this are:
Kidney failure: The kidneys regulate the fluid balance in the body. If the kidneys are weakened (kidney failure) or fail completely (kidney failure), they excrete less or no more fluid. This increases the pressure in the blood vessels, making it easier for the fluid to pass into the tissue - creating edema. Doctors speak of renal pulmonary edema.
Acute kidney failure is a life threatening condition that requires immediate treatment!
ARDS: ARDS is the abbreviation for "acute respiratory distress syndrome", a life-threatening respiratory disease in which the blood vessels in the lungs suddenly become permeable and fluid quickly escapes. ARDS is not an independent disease, but develops as a result of another underlying disease. Patients with severe pneumonia or those who require intensive medical care because of severe injuries, (allergic) shock or blood poisoning (sepsis) are particularly at risk.
Inhalation or absorption of toxins: Certain toxins that are inhaled or reach the lungs via the bloodstream can cause pulmonary edema. Doctors refer to this clinical picture as "toxic pulmonary edema". Regardless of how they get into the body, they damage the blood vessel walls in the lungs so badly that fluid enters the airways.
Examples of toxins that reach the lungs through breathing:
- formaldehyde
- Nitrous gases
- Phosphine
- Hydrogen sulfide
- Sulfur dioxide
- ozone
- Oxygen (in large quantities over a long period of time, such as with continuous ventilation)
- Hydrogen fluoride
- Fluoride
- Smoke poisoning
- Inhaled gastric fluid
Examples of toxins that enter the lungs by blood include:
- heroin
- Methadone
- Venlafaxine (antidepressant)
- Certain chemotherapy drugs
Diseases of the nervous system: Examples of diseases that trigger what is known as "neurogenic pulmonary edema" are epilepsy (in the event of a grand mal seizure) or traumatic brain injury.
Altitude sickness: Even healthy people without previous illnesses develop life-threatening pulmonary edema under certain circumstances. The so-called "high-altitude pulmonary edema", which up to seven percent of all mountaineers develop at high altitudes, is particularly feared. From around 3,000 to 4,000 meters there is only a low oxygen content in the air. This causes the small vessels in the lungs to constrict, blood pressure rises and fluid is pressed into the alveoli.
SIPE: SIPE means “swimming induced pulmonary edema”, English for “diver's edema”. This is a special form of pulmonary edema, the origin of which is not fully understood. The SIPE primarily affects endurance athletes who swim in cold water. Mostly women are affected. The water does not get into the lungs through accidental inhalation. Without water aspiration, fluid accumulates in the lungs, which hinders gas exchange.
Other diseases: Pulmonary edema also occurs in connection with diseases such as lung cancer. In rare cases, life-threatening edema develops after a lung transplant.
How dangerous is pulmonary edema?
Depending on the cause, pulmonary edema occurs suddenly or develops over a long period of time. Acute pulmonary edema is potentially life threatening and requires immediate hospital treatment.
The pulmonary edema itself can be treated well: With timely medical help, the life-threatening acute symptoms can in most cases be controlled by administering oxygen and medication. Long-term chances of survival depend on the cause of the pulmonary edema. If the triggering circumstances are eliminated, the prognosis is good.
Life expectancy after successfully treated pulmonary edema depends on the underlying disease and the patient's state of health. There are large individual differences in how well the patient responds to the individual therapy, for example in the case of heart or kidney disease.
If left untreated, pulmonary edema is life-threatening. If the fluid in the lungs is not removed, the body will no longer receive sufficient oxygen. It comes to respiratory arrest with subsequent multi-organ failure.
How do you know that you have water in your lungs?
The symptoms of pulmonary edema depend on how far the edema has progressed.
The first sign of pulmonary edema is shallow, rapid breathing (shortness of breath). It occurs when the accumulation of fluid is still limited to the lung tissue. If the water has expanded to the alveoli, the symptoms worsen.
It is typical of pulmonary edema that the symptoms improve somewhat when the upper body is straightened. The shortness of breath worsens when lying down. Pulmonary edema patients report excruciating anxiety because they are worried about suffocating. In addition, there is usually a feeling of pressure in the chest area. In the case of pronounced pulmonary edema, clear rattling noises are noticeable when breathing.
In the further course, the body is no longer adequately supplied with oxygen. Visible signs of this are bluish lips and fingers. Those affected often cough up a whitish foam to which blood is mixed in in some cases. In addition, the heartbeat is accelerated.
What to do with pulmonary edema
The immediate start of therapy is crucial for successful treatment. The pulmonary edema itself can usually be treated well. In addition to the acute measures, however, the treatment of the underlying disease is also of crucial importance.
Acute pulmonary edema is a medical emergency! Call an emergency doctor at the first sign! Remain in an upright position and let your legs hang down until the ambulance arrives.This helps to relieve the shortness of breath!
Acute measures
Diuretics: The most important drugs used to treat pulmonary edema are so-called diuretics such as furosemide. They cause more fluid to be excreted through the kidneys and thus flush out existing edema. They also reduce the volume of blood and thus relieve the heart.
Nitrates: The dehydrating agents are usually combined with nitrates such as nitroglycerin. They widen the blood vessels, relieve the heart and improve the oxygen supply.
Antihypertensive drugs: If the blood pressure is also increased in the case of pulmonary edema, the doctors administer antihypertensive drugs (e.g. beta blockers).
Oxygen administration: If the pulmonary edema is so advanced that there is not enough oxygen in the body, patients are given oxygen through a face mask or nasal cannula. In severe cases, artificial ventilation is necessary in the intensive care unit.
Upright position: Pulmonary edema patients are also positioned in the hospital in an upright position (upper body high) in bed. That makes breathing easier.
Other medication: Depending on the symptoms of pulmonary edema, patients are given other medication, such as strong pain relievers, anti-nausea and anti-anxiety drugs.
Treatment of the underlying disease
It is crucial for the long-term success of treatment for pulmonary edema that the triggering disease is optimally treated. Depending on the cause, this may require a wide range of therapeutic measures.
If, for example, a heart attack is the cause of the pulmonary edema, the doctor will conduct a cardiac catheter examination to reopen the blocked heart artery. In the case of pneumonia, the administration of an antibiotic is often necessary. Chronic heart failure usually requires long-term drug treatment. High blood pressure is treated with antihypertensive drugs and general measures (e.g. weight normalization, exercise, healthy eating, smoking cessation).
H2: What does the doctor do?
Your family doctor or pulmonologist is your first point of contact if you have difficulty breathing that gradually develops. Acute breathing problems require emergency medical treatment by the ambulance service or in the hospital.
The doctor first inquires about the current complaints and previous illnesses (lungs, heart). The typical symptoms and the medical history give him the first indications of pulmonary edema.
For further clarification, the doctor will carry out the following examinations:
Clinical examination: the doctor listens to the lungs with a stethoscope and pays attention to the typical rattle noises. Then he measures the blood pressure and heart rate. He also pays attention to signs of an insufficient supply of oxygen, such as blue lips.
Lung X-ray: The most important examination to be able to determine pulmonary edema is an X-ray (alternatively, magnetic resonance imaging is also suitable). With this, an incipient (interstitial) pulmonary edema can be diagnosed, since fluid is clearly visible in the X-ray image.
Heart ultrasound: If it is suspected that the pulmonary edema is the result of a heart disease, the doctor will perform an ultrasound scan of the heart. This allows structural changes such as heart valve defects or a weak heart to be made clearly visible.
EKG: With the help of electrocardiography it is possible to detect heart diseases such as cardiac arrhythmias or a heart attack.
Blood gas analysis and pulse oximetry: To determine whether and to what extent the oxygen saturation of the blood is already restricted, the doctor carries out a blood gas analysis (BGA) or pulse oximetry. With pulse oximetry, a sensor on the finger or earlobe measures the oxygen saturation. A blood sample is required for the BGA.
Blood test: Changes in blood values, for example in the kidneys, indicate possible diseases of the organs.
prevention
Since pulmonary edema is triggered by various causes, there are no specific preventive measures. In any case, it is helpful to prevent underlying diseases such as cardiovascular diseases. General precautionary measures such as a balanced diet, regular exercise and avoiding alcohol and nicotine are suitable for this.
If you have pre-existing conditions, it is important to conscientiously take your prescribed medication and to have regular check-ups. Breathing difficulties with unclear causes should be investigated as early as possible.
The following applies to mountaineers: To prevent pulmonary edema, it is important to ascend slowly and to get your body used to the altitude. From an altitude of around 2,500 to 3,000 meters, no more than 300 to 500 meters of altitude should be covered. We recommend taking a day off every three to four days.
Tags: hospital hair interview