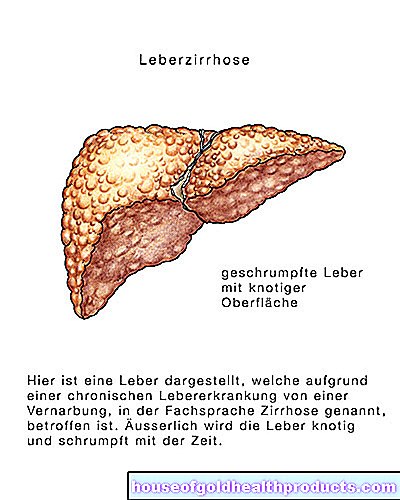
Cirrhosis of the liver
and Martina Feichter, medical editor and biologistMareike Müller is a freelance writer in the medical department and assistant doctor for neurosurgery in Düsseldorf. She studied human medicine in Magdeburg and gained a lot of practical medical experience during her stays abroad on four different continents.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
In cirrhosis of the liver (shrunken liver), the liver tissue perishes and gradually turns into connective tissue - it scars. The more intact liver tissue is lost in this way, the more difficult it is for the organ to perform its tasks. The most common causes of cirrhosis of the liver are chronic alcohol consumption and inflammation of the liver (hepatitis). Read everything you need to know about symptoms, causes, therapy and life expectancy in cirrhosis of the liver.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. K74K76K70K71K72
Brief overview
- Description: In cirrhosis of the liver (shrunken liver), healthy tissue is increasingly converted into non-functional connective tissue (scar tissue). The liver is less and less able to fulfill its important tasks.
- Symptoms: general complaints (such as tiredness, lack of appetite, weight loss), liver skin signs (reddened palms and soles of the feet, itching, yellowing of the skin and the white dermis in the eye, etc.), often also complications (ascites, etc.)
- Causes: mostly alcohol abuse or liver inflammation caused by viruses (hepatitis). Sometimes other diseases of the liver, biliary tract, heart, metabolic diseases, etc. or drugs or toxins
- Treatment: The cause must be eliminated / treated. This can stop the progression of the disease. Existing liver damage cannot be reversed.
- Prognosis: It depends on how advanced the liver cirrhosis is and whether the cause can be eliminated / treated.
What is cirrhosis of the liver?
In the case of cirrhosis of the liver (shrunken liver), liver tissue perishes and gradually transforms into connective tissue (scarring). A possible trigger is liver damage from alcohol abuse, inflammation of the liver (hepatitis) or other diseases.
Organ function decreases due to the increasing restructuring of the liver tissue. In the final stage of liver cirrhosis, the liver can no longer adequately fulfill its tasks as the central metabolic organ: the patient dies due to the collapse of all liver functions (acute liver failure).
Development of cirrhosis of the liver
In Germany, around 250 out of 100,000 people develop cirrhosis of the liver each year. However, experts suspect a high number of unreported cases: The actual number of illnesses is therefore possibly much higher. About twice as many men as women develop and die from cirrhosis of the liver. Mortality has increased in recent years.
Liver cirrhosis: symptoms
Cirrhosis of the liver causes various general symptoms such as tiredness, poor appetite, or nausea. There are also signs of the underlying disease. With more advanced liver damage, specific liver cirrhosis symptoms also occur.
General symptoms of cirrhosis of the liver
Cirrhosis of the liver initially shows no symptoms at all or manifests itself with general symptoms such as:
- Fatigue and poor performance
- Loss of appetite
- nausea
- Weight loss
- Feeling of fullness in the upper abdomen
Liver cirrhosis: symptoms of the underlying disease
In addition, there are often symptoms of the underlying disease, i.e. the actual cause of cirrhosis of the liver. Signs of copper storage disease Wilson's disease, for example, are memory disorders, shakiness and psychosis.
Specific symptoms of cirrhosis of the liver
Later-stage cirrhosis of the liver is associated with specific signs of liver damage: the liver may be enlarged or reduced, rough or bumpy due to the scar tissue that forms. The majority of patients also have an enlarged spleen. Simultaneous enlargement of the spleen and liver is called hepatosplenomegaly.
Other signs of liver cirrhosis are the so-called liver skin signs:
- Yellowing of the dermis of the eyes and the skin (jaundice = jaundice)
- "Vascular spiders" (Spider naevi): small, visible vascular branches that spread out in a star or spider shape (especially on the face and décolleté)
- Reddening of the palms of the hands (palmar erythema) and the soles of the feet (plantar erythema)
- Angle of the mouth rhagades (painful cracks in the corners of the mouth) and lacquer lips (noticeably red, shiny lips)
- itching
Hormonal disorders also occur: if damaged, the liver can no longer properly break down female sex hormones (estrogens), among other things. This can cause the following cirrhosis symptoms:
- Men: breast development, loss of abdominal hair (bald head), shrinkage of the testicles, decrease in sexual desire or potency
- Women: Missing or irregular menstrual periods
Cirrhosis of the liver: signs of complications
If the cirrhosis is very advanced, the liver can no longer compensate for the large loss of functional cells. This decompensated cirrhosis of the liver can cause various complications. These include, for example, ascites, portal hypertension, liver cell cancer and a liver-related brain disease (hepatic encephalopathy). Varicose veins also often develop in the esophagus (esophageal varices).
Such complications cause additional symptoms in cirrhosis of the liver:
Ascites: Ascites very often occurs in cirrhosis of the liver in an advanced stage. The accumulation of fluid increases the size of the abdomen and makes the abdomen bulge. When lying down, the fluid in the abdomen expands to the sides. If it presses on the diaphragm, breathing problems can arise.
Portal vein hypertension: The portal vein collects the blood from various abdominal organs (stomach, intestines, spleen, etc.) and brings it to the liver. In patients with cirrhosis of the liver, this blood can accumulate in front of the scarred liver. Then there is portal hypertension (portal hypertension). Possible consequences include varicose veins in the esophagus (esophageal varices: see below) or stomach, which can burst and cause dangerous bleeding.
Liver cell cancer: Liver cell cancer (hepatocellular carcinoma) can make itself felt as painful tenderness in the right upper abdomen. However, symptoms do not always occur in the early stages. Therefore, all patients with liver cirrhosis are screened for liver cell cancer as a precaution.
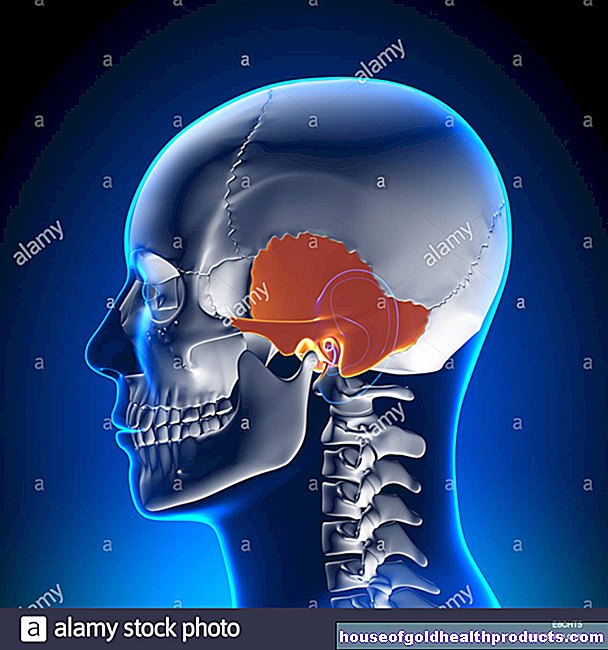
Hepatic encephalopathy: The hepatic encephalopathy is the most important complication of liver cirrhosis. Around 70 percent of those affected show signs of a brain metabolism disorder. The main cause is an increase in toxins such as ammonia in the blood, as the liver's detoxification function is too weak. Depending on the symptoms that occur, hepatic encephalopathy is divided into four stages:
- Stage 1: The sick are somewhat sleepy, slightly slowed down in their reactions and easily confused. Mood swings, poor concentration and slurred speech also occur.
- Stage 2: Drowsiness increases. In addition, the patients appear listless (apathetic), have shaky hands (tremor), and their writing changes.
- Stage 3: The patients sleep a lot but allow themselves to be woken up. Excitement (agitation), aggressiveness, and changes in brain electrical activity (EEG changes) are other signs at this stage.
- Stage 4: The failure of the liver causes the patient to fall into a coma (coma hepaticum). They no longer react to painful stimuli, they no longer show any reflexes, and the air they breathe has a typically sweet smell (foetor hepaticus).
Esophageal varices
Cirrhosis of the liver can cause varicose veins to form in the esophagus. Because the veins in the esophagus then serve as a substitute route for large amounts of venous blood on the way from the abdomen to the heart. These esophageal varices do not initially cause any symptoms.
But it becomes dangerous when the esophageal varicose veins burst. The so-called esophageal variceal bleeding can lead to life-threatening blood loss and manifest itself, among other things, in coughing up blood (hemoptysis). If the patient aspires this blood into the airways, there is a risk of suffocation or severe pneumonia. In addition, the blood can enter the intestines via the stomach and turn the stool black. Doctors speak of a tarry stool.
Variceal bleeding in the esophagus is life-threatening and must be treated immediately by a doctor!
You can read more about this in the article Esophageal Varices.
Liver cirrhosis: therapy
The progression of cirrhosis of the liver can be stopped if the cause is eliminated in good time. With the right treatment, the symptoms can also be alleviated. Any damage that has already occurred remains - it can no longer be undone.
Liver cirrhosis therapy consists of several components:
The patient must avoid substances that are harmful to the liver. This primarily includes alcohol. Refraining from alcohol does not only apply to patients with alcohol-related cirrhosis of the liver, but also to everyone else! The doctor can give tips and options for alcohol withdrawal (advice centers, therapy centers, etc.). Patients should also seek support from family members, friends, and / or support groups (such as Alcoholics Anonymous).
Medicines also damage the liver: They should therefore only be taken in cirrhosis if it is medically absolutely necessary. In addition, patients should always ask their doctor first before using any preparations on their own, including over-the-counter drugs and dietary supplements.
Any liver cirrhosis therapy also includes treating the underlying disease that causes it (as best it is possible). For example, the doctor prescribes certain medications for inflammation of the liver (hepatitis).
The targeted treatment of complications is also very important. For example, in ascites, water tablets (diuretics) help to flush out the accumulated fluid. In addition, those affected should eat a low-sodium diet. In severe cases of ascites, a so-called puncture may be necessary: the doctor pierces the abdomen with a thin needle to drain the fluid through a tube.
In severe, advanced liver cirrhosis, a liver transplant is often the patient's last chance.
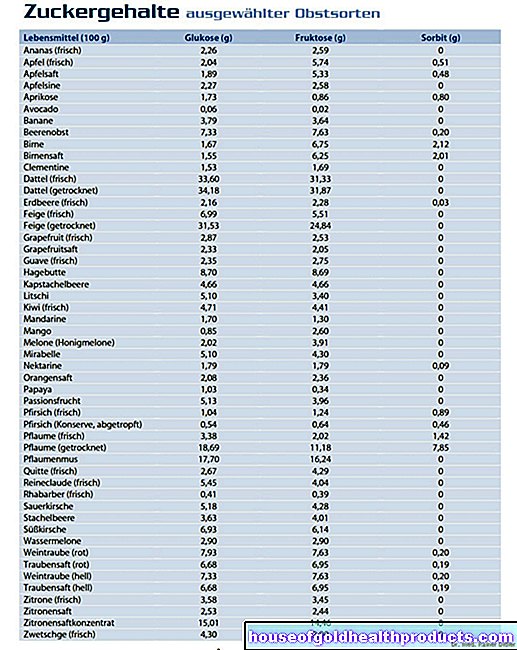
Liver cirrhosis & nutrition
In general, doctors recommend a balanced diet rich in vitamins for people with cirrhosis of the liver. If there are no complications and the patient's nutritional status is normal (neither overweight nor underweight), a special "liver diet" does not make sense. If a special diet is necessary, the attending physician will discuss this with the patient.
For example, overweight patients with fatty liver should eat a low-fat, low-calorie diet. This will help you lose weight (along with regular exercise).
If liver damage is already disrupting brain functions (hepatic encephalopathy), it is particularly important to reduce toxins in the blood. For this purpose, those affected should eat less protein - then less toxic ammonia is produced in the body. In addition, the elimination of this toxin can be promoted with lactulose, a light laxative.
The same applies to all other patients with cirrhosis of the liver: You should ensure regular bowel movements to support the elimination of toxins via the intestines. A fiber-rich diet and an adequate intake of fluids help. The patient should discuss with the doctor in charge what amount to drink per day is sensible and advisable. In certain cases you shouldn't ingest too much fluid, such as ascites.
Liver cirrhosis: causes and risk factors
Various diseases can lead to liver cirrhosis as a long-term consequence. In the industrialized countries, alcohol abuse occurs in more than half of all cases of cirrhosis of the liver. In the remaining patients, the cirrhosis of the liver can be traced back to an inflammation of the liver (hepatitis B or hepatitis C) or (less often) another disease. Sometimes it is also caused by medication.
Cirrhosis of the liver from alcohol
Long-term alcohol abuse is one of the main causes of liver cirrhosis in Germany. Doctors also refer to this as ethyl-toxic liver cirrhosis.
As the central metabolic organ, the liver is responsible for breaking down the large amount of alcohol. This creates more toxins. First of all, they cause the liver to store a lot of abnormal fat - a so-called fatty liver is created. At this stage the changes in the liver tissue are still partially reversible.
If the excessive consumption of alcohol continues, the cells overloaded with fat perish. They are replaced by connective tissue (scar tissue). Doctors then speak of liver fibrosis. The development of the scar and connective tissue can no longer be reversed. If the fibrosis progresses, it will ultimately lead to cirrhosis of the liver.
The amount of alcohol that leads to cirrhosis of the liver varies greatly from person to person. In general, the daily consumption of about 40 grams of alcohol in men can irreparably damage the liver. Women are more sensitive to the pleasure poison. Therefore, even 20 grams of alcohol per day can cause permanent liver damage in them.
Cirrhosis of the liver due to viral hepatitis
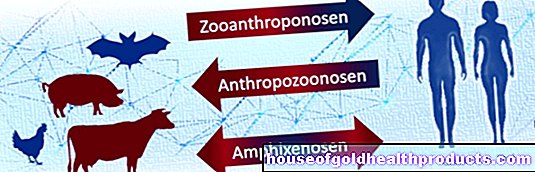
More than 30 percent of all liver cirrhosis cases in Germany are caused by chronic liver inflammation (hepatitis) of type B or C. Both forms of the disease - hepatitis B and hepatitis C - are each triggered by a certain type of virus. These viruses are found in practically all body fluids such as blood, semen, urine or saliva in infected people.
The chronic inflammation can damage the liver cells over time to such an extent that they die and scar - cirrhosis of the liver develops.
Other causes of liver cirrhosis
Other causes of cirrhosis of the liver can be:
- Liver and biliary diseases: e.g. immune-related inflammation of the liver (autoimmune hepatitis), chronic inflammation of the small bile ducts in the liver (primary biliary cirrhosis / cholangitis, PBC), chronic inflammation and scarring of the middle and larger bile ducts (primary sclerosing cholangitis, PSC)
- Metabolic diseases: iron storage disease (hemochromatosis), copper storage disease (Wilson's disease), cystic fibrosis, etc.
- Tropical diseases such as schistosomiasis or liver fluke infestation
- Heart disease such as chronic right heart failure (right heart failure)
- Toxins like carbon tetrachloride or arsenic
- Medications such as methotrexate (for cancer and autoimmune diseases)
In some cases, the cause of the disease cannot be found. Then there is what is known as cryptogenic liver cirrhosis.
Liver cirrhosis: examinations and diagnosis
The doctor will first collect the patient's medical history in conversation with him (anamnesis). He has the symptoms described in detail and asks about any previous or underlying illnesses. A possible hepatitis infection is particularly important. In addition, the doctor asks if the patient is using any medication and how much alcohol he is consuming.
Physical examination
The next step is a physical examination if cirrhosis of the liver is suspected. The doctor feels the size of the liver and spleen as well as the edge of the liver. He also taps the abdomen to see if there is any fluid in the abdominal cavity (ascites).
The so-called liver skin signs are also an important indicator of liver cirrhosis. The doctor checks, for example, whether the palms of the hands are reddened (palmar erythema), "vascular spiders" (Spider naevi) or whether the patient has jaundice (jaundice).
Blood test
A blood test can determine the extent of the liver damage. If the following values are reduced, this indicates that the liver is no longer working as well:
- albumin
- Cholinesterase (CHE)
- Coagulation factors II, VII, IX, X (this lowers the Quick value, i.e. it takes longer for the blood to clot)
The following values can be increased in cirrhosis of the liver:
- Bilirubin
- Ammonia (for hepatic encephalopathy)
- the liver enzymes GOT (ASAT), GPT (ALAT), GLDH and Gamma-GT
Imaging methods
Using ultrasound (sonography), the doctor can assess the size and condition of the liver. It can also be used to determine hypertension of the portal vein. Sometimes the doctor also uses a special ultrasound technique for this - Doppler sonography. Another special form of ultrasound (Fibroscan) shows how severely the liver is already scarred.
Computed tomography (CT) is only necessary if the ultrasound findings are unclear.
In order to demonstrate the structural remodeling in scarred connective tissue, the doctor takes a tissue sample (biopsy) from the liver and sends it to the laboratory for analysis.
Further investigations
Sometimes further tests are indicated. A gastroscopy is often recommended for newly discovered cirrhosis of the liver. The doctor can track down varicose veins in the esophagus or in the stomach.
So-called psychometric tests can be carried out to clarify slight brain damage caused by liver cirrhosis (hepatic encephalopathy).
Stages of cirrhosis of the liver: Child-Pugh score
Liver cirrhosis can be divided into different stages. Doctors use the so-called Child-Pugh Score: It takes into account five criteria that give an indication of how far advanced the shrink liver is. The Child-Pugh criteria are:
- Ascites, assessed on ultrasound
- Damage to the brain caused by liver disease (hepatic encephalopathy)
- Albumin concentration in the blood: Albumin is a protein that is produced in the liver. Less albumin is produced in cirrhosis of the liver.
- Bilirubin concentration in the blood: Bilirubin is a breakdown product of the blood pigment hemoglobin. It is usually broken down further in the liver. In cirrhosis of the liver, it accumulates in the blood.
- Quick value: this marker for blood coagulation depends on coagulation factors that are produced in the liver. Less coagulation factors are formed in cirrhosis of the liver. This reduces the Quick value. Alternatively, blood coagulation is now often described using the INR value: it is the opposite of the Quick value (e.g. high Quick value, low INR).
The doctor checks each criterion in the patient and awards points in each case:
|
criteria |
1 point |
2 points |
3 points |
|
Albumin (g / dl) |
> 3,5 |
2,8 - 3,5 |
< 2,8 |
|
Ascites |
no |
little |
pronounced |
|
Bilirubin (mg / dl) |
< 2,0 |
2,0 - 3,0 |
> 3,0 |
|
hepatic encephalopathy |
no |
moderate |
pronounced |
|
Quick value (%) or INR |
> 70% or <1.7 |
40 - 70% or 1.7 - 2.3 |
2,3 |
If the liver cirrhosis is caused by primary biliary cirrhosis, the bilirubin value is assessed differently: 1 point is awarded for measured values below 4 mg / dl. If the bilirubin value is between 4 and 10 mg / dl, there are 2 points. The doctor awards 3 points for bilirubin values above 10 mg / dl.
Stages of cirrhosis of the liver
All the points scored add up to the Child-Pugh Score. It is between 5 and 15 points: Cirrhosis of the liver of the mildest severity gives a value of 5. In contrast, if the liver is severely damaged, a total of 15 points is achieved.
The individual point ranges are assigned to different stages of liver cirrhosis: If the total number of points is 5 to 6, there is liver cirrhosis Child A - the mildest stage of liver cirrhosis. Child B corresponds to a Child-Pugh score of 7 to 9. In contrast, scores 10 to 15 indicate the highest stage of liver cirrhosis: Child C.
Based on the stage, the doctor can estimate how high the risk of death is for the patient for the following twelve months:
|
Child-Pugh Score |
stage |
1 year mortality |
|
5 - 6 |
Child A |
3 to 10% |
|
7 - 9 |
Child B |
10 to 30% |
|
10 - 15 |
Child C |
50 to 80% |
As the table shows, the mortality in the first year of stage Child A is still quite low. However, it increases significantly as the liver cirrhosis progresses.
Liver cirrhosis: disease course and prognosis
The earlier cirrhosis of the liver is recognized and treated, the better the prognosis. Effective treatment includes eliminating or treating the cause of the disease (alcoholism, hepatitis, etc.). For example, alcoholics who permanently stop drinking have a comparatively good prognosis for cirrhosis of the liver. However, the damage that has already occurred is not curable. Only the progression of cirrhosis can be stopped.
The outlook is much worse if people with alcohol-related cirrhosis of the liver continue to drink alcohol. Every second one of them dies within five years. However, complications of liver cirrhosis can also worsen the life expectancy of the patient.
The most common causes of death in cirrhotic patients are liver failure, bleeding from varicose veins in the esophagus or stomach, and liver cancer (liver cell cancer).
Liver cirrhosis: prevention
If you want to prevent cirrhosis of the liver, you should primarily avoid alcohol or at least consume it in moderation: Healthy men can drink up to 0.75 liters of beer or three eighth liters of wine a day. Healthy women are recommended a maximum of 0.5 liters of beer or a quarter of a liter of wine. The following applies to both genders: You shouldn't treat yourself to this "permitted" amount of alcohol every day!
With a hepatitis vaccination you can prevent the second most common cause of cirrhosis of the liver. Such a vaccination is especially advisable before you plan to travel abroad.
Watch out for toxic chemicals in the workplace (carbon tetrachloride, benzene, etc.): Company doctors or occupational physicians explain possible dangers and occupational safety measures.
Only take medication and vitamin supplements when necessary. As the central metabolic organ, the liver has to break down and detoxify all foreign substances. Ask your doctor or pharmacist in advance how harmful a product is to the liver - there may be a better tolerated product that does not increase the risk of liver damage and cirrhosis.
Additional information
Guidelines:
S3_Leitlinie "Ascites, spontaneous bacterial peritonitis, hepatorenal syndrome" of the German Society for Digestive and Metabolic Diseases
Self-help groups:
- German Liver Aid e.V .: https://www.leberhilfe.org/




.jpg)