Type 3 diabetes
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
The term type 3 diabetes covers various rare forms of diabetes that develop in a different way than type 1 and type 2 diabetes. LADA also occupies a special position. Read everything you need to know about type 3 diabetes and LADA diabetes here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. E13
What is type 3 diabetes?
The term type 3 diabetes (or “other specific types of diabetes”) encompasses several special forms of diabetes mellitus. They are all much rarer than the two main forms of type 1 and type 2 diabetes. Type 3 diabetes includes the following subgroups:
- Type 3a diabetes: caused by gene defects in the insulin-producing beta cells; also called MODY
- Type 3b diabetes: caused by genetic defects in the action of insulin
- Type 3c diabetes: caused by diseases of the pancreas (pancreopriver diabetes)
- Type 3d diabetes: caused by diseases / disorders of the endocrine system
- Type 3e diabetes: caused by chemicals or drugs
- Type 3f diabetes: caused by viruses
- Type 3g diabetes: caused by autoimmune diseases
- Type 3h diabetes: caused by genetic syndromes
By the way: Gestational diabetes is sometimes referred to as type 4 diabetes.
Type 3a diabetes (MODY)
It is estimated that one to two percent of all diabetics suffer from type 3a diabetes (also called MODY). The abbreviation MODY stands for "Maturity Onset Diabetes of the Young". So far, there are 13 different forms of adult diabetes (MODY1 to 13) that already occur in children and adolescents. They are caused by various genetic defects in the insulin-producing beta cells in the pancreas. The mutations cause abnormal development of the pancreas or islet cells (which include beta cells), or they cause insulin to be disrupted. All of them lead - like every form of diabetes - to abnormally high blood sugar levels (hyperglycaemia).
MODY is inheritable. Therefore, several members of a family are usually affected. The disease usually breaks out before the age of 25. Most of the patients are of normal weight, as are type 1 diabetics. In contrast to these, MODY patients do not have any diabetes-specific autoantibodies.
The different MODY variants show slightly different clinical pictures with different degrees of hyperglycaemia. MODY2, for example, is mild and stable for years. A diet and regular physical activity are usually sufficient treatment because the body still produces sufficient insulin. Diabetic secondary diseases (such as retinal damage, kidney disease, diabetic foot, etc.) are rare here.
The situation is completely different with MODY1: This form of type 3 diabetes is becoming increasingly difficult and often causes secondary diseases. Patients must use oral antidiabetic drugs (sulfonylureas) to lower their high blood sugar levels. Some also need insulin as they get older.
With MODY3 the course is initially quite mild. However, the disease continues to progress. Most of those affected need oral antidiabetic drugs, and later sometimes also insulin. Often there are complications that are typical of diabetes.
The other MODY variants are extremely rare.
By the way: MODY patients are often initially classified as type 1 diabetics. If you are very overweight (which is less common), type 2 diabetes can be mistakenly diagnosed.
Type 3b diabetes
This form of type 3 diabetes is based on genetic defects in the action of insulin. A distinction is made between different variants:
Insulin resistance type A is associated with a very pronounced insulin resistance: The patient's body cells hardly respond to insulin. Other symptoms include what is known as acanthosis nigricans. These are gray-brown-black skin changes with a velvety appearance. They form mainly in the flexion folds (armpits, neck, etc.). Acanthosis nigricans is not specific to this form of type 3 diabetes. It is often seen in many other diseases, such as stomach cancer.
In lipatrophic diabetes (Lawrence syndrome), the insulin resistance is very pronounced. In addition, the body fat is gradually reduced. This is indicated by the term lipatrophy (= shrinkage of the subcutaneous fatty tissue). So far there is no known effective therapy for lipatrophic diabetes.
Type 3c diabetes
This representative of type 3 diabetes is also called pancreatic diabetes. It is caused by diseases or injuries to the pancreas, which, among other things, impair the secretion of insulin. Examples:
- Chronic inflammation of the pancreas (chronic pancreatitis): It affects both the secretion of digestive enzymes (exocrine pancreatic function) and the secretion of insulin, glucagon and other pancreatic hormones (endocrine function). The main cause is chronic alcohol consumption.
- Injuries to the pancreas (such as in accidents)
- surgical removal of the pancreas (in whole or in part), for example due to a tumor
- Pancreatic neoplasms (neoplasm or neoplasm = increased formation of new tissue)
- Cystic fibrosis: incurable hereditary disease. About 30 percent of patients also develop type 3 diabetes because viscous secretions form in the pancreas. It clogs the ducts and damages the cells that produce insulin and other pancreatic hormones. Insulin therapy necessary.
- Hemochromatosis: In iron storage disease, more iron is stored in the body, which damages the tissue in various organs. In the pancreas, the insulin-producing beta cells are destroyed. This form of type 3 diabetes is also called "bronze diabetes" because the iron deposits on the skin take on a bronze tint.
Diabetes type 3d
Type 3 diabetes can also occur in the context of other hormonal (endoctrine) diseases and disorders. They are then grouped under the term type 3d diabetes. The triggering hormonal diseases include:
- Acromegaly: There is excess growth hormone (mostly due to a benign tumor of the pituitary gland). As a result, more glucose is newly formed in the liver (gluconeogenesis). This increases the blood sugar levels. At the same time, the growth hormone promotes insulin resistance in the cells. Overall, this results in type 3 diabetes.
- Cushing's disease: This is where the body secretes more of the hormone ACTH, which in turn increases the release of the body's own cortisone. This causes increased blood sugar levels and thus type 3 diabetes. Further consequences of the ACTH excess are trunk obesity, osteoporosis and high blood pressure.
- Glucagonoma: Mostly malignant tumor of the glucagon-producing cells in the pancreas (A cells). It can produce excessive amounts of glucagon. Because this hormone is the antagonist of insulin, an excess can cause the blood sugar to rise abnormally - this leads to type 3 diabetes.
- Somatostatin: Malignant tumor of the pancreas or duodenum that produces an increased amount of the hormone somatostatin. Among other things, this inhibits the production of insulin. As a result, blood sugar can no longer be lowered sufficiently, so that type 3 diabetes develops.
- Pheochromocytoma: Mostly benign tumor of the adrenal medulla. It can stimulate the formation of new glucose (gluconeogenesis) so strongly that the blood sugar levels rise abnormally - type 3 diabetes develops.
- Aldosteronome: tumor of the adrenal cortex that produces a lot of aldosterone. It can also increase your risk of type 3 diabetes.
- Hyperthyroidism: Hyperthyroidism can also derail blood sugar levels, so that patients become diabetic.
Type 3e diabetes
Various chemicals and (rarely) drugs can cause type 3e diabetes. These include, for example:
- Pyrinuron: rodent poison (rodenticide) and part of the rat poison Vacor (was only on the market in the USA and is no longer approved)
- Pentamidine: active ingredient against protozoa; used in the treatment of infestations such as leishmaniasis
- Glucocorticoids ("cortisone"): They increase the blood sugar level via various mechanisms, for example by inhibiting the release of insulin and increasing the formation of new glucose (especially in the liver).
- Thyroid hormones: used to treat an underactive thyroid (hypothyroidism)
- Thiazide diuretics: water tablets that are prescribed for heart failure (heart failure) and high blood pressure
- Phenytoin: anticonvulsant used to treat epilepsy and irregular heartbeat
- Beta-sympathomimetics: among other things for the treatment of COPD, asthma and irritable bladder
- Diazoxide: used to treat low blood sugar (hypoglycaemia)
- Interferon-alpha: among other things for the treatment of hepatitis B and hepatitis C.
- Nicotinic acid: water-soluble vitamin from the group of B vitamins; can worsen glucose tolerance (i.e. the normal = healthy reaction of the body to a glucose supply)
Type 3f diabetes
In rare cases, certain viral infections can also trigger type 3 diabetes, such as rubella virus and cytomegalovirus. Unborn children are primarily at risk: the viruses can be transmitted to them by the expectant mother. Possible viral triggers of type 3 diabetes are, for example:
- Congenital rubella infection: A rubella infection after the first trimester of pregnancy can cause inflammation of the pancreas (pancreatitis) in the unborn child. This can lead to a lack of insulin and thus to type 3 diabetes.
- Congenital cytomegaly virus infection: The cytomegaly virus (CMV) belongs to the group of herpes viruses and is very common worldwide. It is mostly harmless to healthy adults. For unborn babies, however, a CMV infection can mean serious damage to health and even life. Among other things, the child can develop inflammation of the pancreas and subsequently diabetes.
Type 3g diabetes
In individual cases, certain autoimmune diseases result in type 3 diabetes:
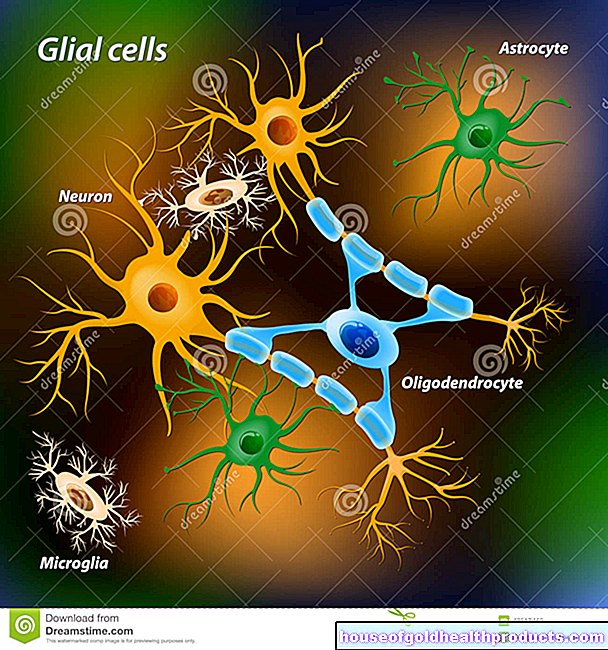
- "Stiff-man" syndrome: an autoimmune disease of the central nervous system (brain and spinal cord) and the endocrine system
- Anti-insulin receptor antibodies: They occupy the docking sites for insulin on the surface of body cells. The insulin can then no longer dock itself and ensure that blood sugar is absorbed into the cells.
Type 3h diabetes
This includes forms of type 3 diabetes, which occur in connection with various genetic syndromes. This includes:
- Trisomy 21 (Down syndrome): Those affected have three instead of two copies of chromosome 21.
- Klinefelter Syndrome: Affected boys / men have an extra X chromosome. This is why it is also called XXY syndrome.
- Turner syndrome: In affected girls / women, one of the two existing X chromosomes is missing or it is structurally defective.
- Wolfram syndrome: Neurodegenerative disease associated with neurological symptoms, atrophy of the optic nerve (optic atrophy), diabetes mellitus type 1 and diabetes insipidus. The latter is a disorder of the water balance that does not belong to diabetes mellitus.
- Huntington's disease: Hereditary neurological disease with abnormally increased mobility of the skeletal muscles.
- Porphyria: Hereditary or acquired metabolic disease in which the formation of the red blood pigment (heme) is disturbed.
- Friedreich's ataxia: Hereditary disease of the central nervous system that causes neurological deficits, malformations of the skeleton and diabetes, among other things.
- Dystrophia myotonica: Hereditary muscle disease with muscle wasting and weakness as well as other complaints such as cardiac arrhythmias, cataracts and diabetes mellitus.
- Prader-Willi syndrome (Prader-Willi-Labhart syndrome): genetic defect on chromosome 15, which is associated with physical and mental limitations and disabilities.
Between type 1 and 2: LADA
The abbreviation LADA stands for "Late autoimmune diabetes in adults". It is a special form of diabetes that stands between type 1 and type 2 diabetes:
In LADA patients, diabetes-specific autoantibodies are found in the blood as in type 1 diabetics. The latter, however, have at least two different types of such antibodies, for example autoantibodies against insulin (AAI), against islet cells (ICA) or against glutamic acid decarboxylase (GADA). In contrast, LADA patients only have GADA in their blood.
Another difference to the "classic" type 1 diabetes is that people with LADA are usually older than 35 years when they are diagnosed and usually do not have to inject any insulin in the first six months (their body usually still produces enough of its own insulin). Later, sometimes - but not always - insulin therapy may be necessary. Type 1 diabetes, on the other hand, usually affects children or adolescents, who then all need insulin therapy right from the start.
On the other hand, LADA shows overlaps with type 2 diabetes. Both forms of diabetes generally appear at about the same age. In addition, LADA patients such as type 2 diabetics often show evidence of a metabolic syndrome such as lipid metabolism disorders and high blood pressure. However, people with LADA are usually leaner than those with type 2 diabetes.
The causes for the LADA have not been conclusively clarified. This particular form of diabetes is sometimes referred to as mixed diabetes, a mixture of type 1 and type 2 diabetes. That's not right. Rather, LADA seems to be two symptoms that exist at the same time and that develop in parallel. However, the similarities and overlaps with other forms of diabetes do not make it easy for doctors: In everyday practice, LADA is often difficult to distinguish from type 1 and type 2 diabetes and also from type 3 diabetes.
Tags: teeth drugs organ systems