Spirometry
Updated on All content is checked by medical journalists.Spirometry (also: spirography) is a routine procedure for examining lung function. To do this, the doctor measures the amount and speed of air you breathe. He can use it to detect many lung diseases such as asthma or COPD or to check the success of therapy in such diseases. Read everything you need to know about performing spirometry, evaluation and possible risks here.

Spirometry: when is it necessary?
Reasons for a spirometric examination include:
- Clarification of the cause of chronic cough or shortness of breath (dyspnoea)
- Suspected respiratory, lung, or heart disease
- Suspected respiratory muscle disorders
- chronic tobacco use
- Pulmonary function test before operations
- general health care
- Occupational medical control for the prevention and diagnosis of occupational diseases
As a rule, the health insurance company bears the costs for the examination.
Spirometry: implementation
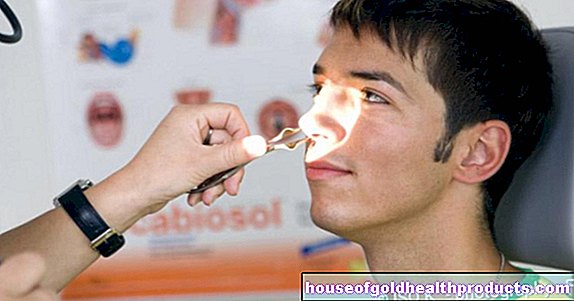
In the case of spirometry, the patient is given a mouthpiece that becomes a measuring device for and that he should firmly enclose with both lips. His nose is closed with a nose clip. On the instructions of the doctor, the patient now inhales and exhales through the mouthpiece for about five to ten minutes: After inhaling as deeply as possible, the patient should exhale as quickly and forcefully as possible.
The so-called spirometer, which is connected to the mouthpiece, records the force and volume of the breaths and shows the breaths in a graph. This allows the doctor to assess how strong the breath flow is and how large certain parameters are for lung function. These include, for example, the one-second capacity, FEV1 (= largest possible lung volume that can be exhaled within one second) and the vital capacity, FVC (= total lung volume that can be exhaled forcibly after deep inhalation).
In order for the findings to be meaningful, it is very important that the patient follows the doctor's instructions exactly during the examination and works well.
Bronchospasmolysis test
In some cases (e.g. to diagnose COPD or asthma) the doctor combines spirometry with another measurement:
First, the spirometry is performed as described above. Then the patient inhales a drug that can widen the airways (bronchodilator). The spirometry is then repeated.
The comparison of the measured values before and after the administration of the medication helps the doctor to narrow down the diagnosis of a breathing disorder. If the second measurement improved to a certain extent compared to the first measurement, then the bronchodilator has widened previously narrowed airways - the patient is likely to have asthma.
Spirometry: evaluation
The doctor can draw conclusions about the function of the lungs on the basis of the graphic representation of the breaths. Because different diseases result in specific changes in the shape of the breathing curve.
Diseases with narrowed airways, for example, show prolonged and decreased exhalation. The Tiffeneau index (= ratio between one-second capacity and vital capacity) is then reduced.
If the vital capacity is reduced, this can be due to a reduced elasticity of the lungs (restriction) or to an overinflation of the lungs (pulmonary emphysema). Further research is then needed to distinguish between these two possible causes.
The doctor cannot diagnose some lung diseases with spirometry. For example, patients with respiratory failure show almost normal spirometry parameters. Therefore, this pulmonary function test also includes other tests.
Spirometry: what are the risks?
Spirometry is a simple and practically risk-free procedure. Deep breathing can sometimes lead to an irritation of the throat and dry mouth or slight dizziness. But both quickly evaporate again.
Tags: drugs dental care diet