cervical cancer
and Martina Feichter, medical editor and biologistFabian Dupont is a freelance writer in the medical department. The human medicine specialist is already doing scientific work in Belgium, Spain, Rwanda, the USA, Great Britain, South Africa, New Zealand and Switzerland, among others. The focus of his doctoral thesis was tropical neurology, but his special interest is international public health and the comprehensible communication of medical facts.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Women get cervical cancer on average at the age of 53. The trigger is usually a specific viral infection (HPV) in the genital area. In the early stages, cervical cancer is almost always curable. As the tumor spreads, the chances of recovery decrease. Read everything you need to know about the causes, symptoms, diagnosis, treatment, prognosis and prevention of cervical cancer!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. C53C57
Brief overview
- What is cervical cancer? A malignant growth of cells in the area of the cervix.
- Frequency: Around 4,300 new cases of cervical cancer are expected in Germany in 2018. This incidence rate has been largely stable since the late 1990s. The mean age of onset is 53 years. Women who develop a preliminary stage of cervical cancer (in-situ carcinoma) are on average 34 years old.
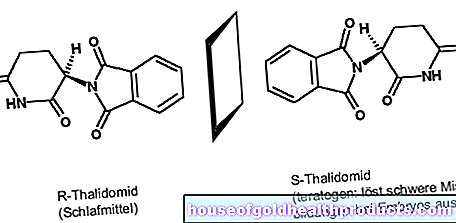
- Causes: primarily an infection with the sexually transmitted human papilloma virus (HPV). Other risk factors include smoking, frequently changing sexual partners, many births, poor genital hygiene and long-term use of the "pill".
- Symptoms: usually only in advanced stages of cancer, e.g. bleeding after sexual intercourse or after the menopause, heavy menstrual bleeding, intermenstrual bleeding or spotting, discharge (often smelly or bloody), pain in the lower abdomen, etc.
- Therapy: surgery, radiation and / or chemotherapy, targeted therapy (antibody therapy)
- Prognosis: The earlier cervical cancer is detected and treated, the higher the chances of a cure.
Cervical cancer: anatomy
The cervix (cervix) forms the transition between the body of the uterus (uterus) and the vagina (vagina). During sexual intercourse, sperm pass through it from the vagina into the uterine cavity inside the uterus.
The opening of the cervix towards the vagina is called the external cervix. The opening towards the body of the uterus is called the inner cervix.
The inside of the cervix is lined with a mucous membrane: it consists of a covering tissue (squamous epithelium) and mucous glands embedded in it. If the lining of the cervix changes malignantly, it is called cervical cancer (cervical cancer). In most cases it starts from the squamous epithelium and is then one of the so-called squamous cell carcinomas. Less often, cervical cancer develops from the glandular tissue of the mucous membrane. Then it is an adenocarcinoma
In most patients, cervical cancer develops in the area of the external cervix.
Anatomy of the internal female genital organs
Cervical cancer should not be confused with uterine cancer (uterine body cancer). The latter is also called "uterine carcinoma", endometrial carcinoma "or" body carcinoma "in medical jargon.
Cervical Cancer: Causes & Risk Factors
Cervical cancer is usually triggered by a chronic infection with the human papilloma virus (HPV). There are around 200 different types of this virus. Some of them are considered to be particularly aggressive and dangerous and are therefore called "high risk" types. These include HPV 16, 18, 31, 45, 51 and 52. Types 16 and 18 alone are responsible for more than 70 percent of all cervical cancer diseases.
The "low risk" HPV types are not involved in the development of cervical cancer. However, they can cause warts on both male and female genitals.
HPV is transmitted almost exclusively through sexual intercourse. Even condoms are not sufficient protection against the human papilloma virus. The pathogens can be transmitted through skin contact in the genital area.
Almost everyone comes into contact with HPV at least once in their life. In most cases, the immune system can handle the virus, even if it is a high risk type of virus. Less than 1 in 100 women infected with a high-risk type of HPV will actually develop cervical cancer.
-
"Protect vaccinations and condoms"
Three questions for
Dr. med. Christoph Bauer,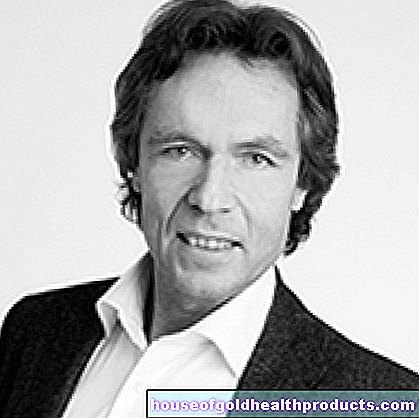
Specialist in Obstetrics and Gynecology -
1
Who is particularly at risk?
Dr. med. Christoph Bauer
Most cervical cancer is caused by HP viruses. Because of this, women who have become infected with HP virus type 16 or 18 are particularly at risk. Especially if you had a medical smear test. The monitoring should then be carried out more closely.
-
2
What protects against cervical cancer?
Dr. med. Christoph Bauer
Since HPV is predominantly sexually transmitted, vaccination and condoms are the best protective measures. The vaccination can also be carried out in adulthood if one is not already infected with HPV. Regular preventive examinations are useful, even if you have been vaccinated, possibly with additional testing for HPV.
-
3
Is the entire uterus always removed in cervical cancer?
Dr. med. Christoph Bauer
If you already have cervical cancer, the entire uterus is removed. In the case of preliminary stages, it is also sufficient to remove part of the cervix. This usually doesn't affect the hormones - the ovaries stay intact.
-
Dr. med. Christoph Bauer,
Specialist in Obstetrics and GynecologyDr. Christoph Bauer runs a private practice for gynecology in Munich, with a focus on preventive medicine and menopause, among other things.
Cervical cancer: other risk factors
Another big risk factor for cervical cancer is smoking. Certain toxins from tobacco are specifically deposited in the tissue of the cervix. This makes the tissue more vulnerable to viruses such as HPV.
Other risk factors for cervical cancer are:
- Large number of sex partners: The more sex partners a woman has in her life, the higher her risk of cervical cancer.
- Early onset of sexual activity: Girls who have sexual intercourse before the age of 14 have an increased risk of HPV infection - and thus also of developing cervical cancer (or its precursors).
- poor genital hygiene: it makes you more susceptible to HPV infections and many other sexually transmitted diseases. For example, the HPV infection rate is lower in circumcised men than in uncircumcised men.
- Low socioeconomic status: People on low incomes are more likely to be infected with HPV than people of higher social class.
- Many pregnancies and births: Every pregnancy that lasts for at least five to six months or every birth increases the risk of HPV infection and thus of cervical cancer. This is either due to tissue changes during pregnancy or because women with a low socioeconomic status in particular become pregnant several times.
- Long-term use of oral contraceptives ("Pills"): Women infected with a high-risk type of HPV who have been taking birth control pills with estrogen and progestin for five years or more have a slightly increased risk of cervical cancer.
- Other sexually transmitted diseases: In women who are infected with HPV, an additional sexually transmitted disease (such as genital herpes or chlamydia) can also contribute to the development of cervical cancer.
- Weakened immune system: A weak immune system can either be caused by an illness (such as AIDS) or by drugs that suppress the immune system (administered after transplants, for example). In any case, a weakened immune system is unlikely to be able to fight an HPV infection effectively.
According to the current state of knowledge, genetic factors play only a subordinate role in the development of cervical cancer.
Cervical cancer: symptoms
Cervical cancer usually does not cause symptoms in the early stages. Cervical cancer precursors also go unnoticed for a long time.
Only over time do the malignant cell changes become noticeable with symptoms such as vaginal discharge - it can be bloody or smelly. Bleeding after intercourse can also be a sign of cervical cancer. The same applies to bleeding after exertion such as cycling, riding or having a hard stool.
In women over 35 years of age, heavy menstrual periods, intermenstrual bleeding or spotting are also considered to be potentially cancerous. Postmenopausal bleeding can also be symptoms of cervical cancer.
The complaints mentioned are not clear signs of cervical cancer! They can have other causes as well. As a precaution, however, you should have it checked out by a doctor.
Some patients also report pain in the lower abdomen. Inexplicable weight loss is also common in women with cervical cancer.
Signs of involvement of other organs also appear in advanced stages of cancer. Some examples:
- Lymphedema (swelling of the legs with damp, distended skin) occurs when the lymphatic system is affected extensively.
- The urine may turn red if the cancer cells have invaded the urinary tract and bladder, causing bleeding into the bladder.
- Deep back pain, which often also radiates into the pelvis, are possible signs of cancer of the pelvis and spine.
- Severe abdominal pain with paralysis of the intestinal activity is possible if the abdominal intestines are affected by cancer. If the intestines are affected, bowel movements can also be disturbed.
In the last stage, the tumor spreads all over the body. Many vital organs then fail, which ultimately leads to death.
Cervical cancer: examinations and diagnosis
The most important examination is the regular check-up at the gynecologist (early cancer detection). This also applies to women who have been vaccinated against the most important HP viruses: A vaccination does not replace preventive care, but only complements the preventive program.
In Germany, every woman over the age of 20 can have a preventive / early diagnosis examination carried out by a gynecologist once a year. All health insurers assume the costs for this. More information can be obtained from any gynecologist.
Women should definitely take advantage of the free cancer screening test! The earlier malignant cell changes are discovered and treated, the better the prognosis.
The routine examination for the early detection of cervical cancer is the same as the examination that is carried out if there is a specific suspicion of cervical cancer (due to symptoms such as irregular bleeding):
Anamnesis interview
First of all, the doctor will collect the patient's medical history (anamnesis) in conversation with the woman. For example, he asks how regular and heavy the menstrual bleeding is and whether there is occasional intermenstrual bleeding or spotting. He also asks about any complaints and previous illnesses as well as the use of contraceptives.
Gynecological examination & PAP test
The conversation is followed by a gynecological examination: the gynecologist first examines the external genital organs such as the labia for any abnormalities. Then he spreads the vagina open with the help of a metal spatula (speculum). So he can take a look at the vaginal walls and the external cervix.
He also takes a cell sample from the surface of the mucous membrane on the cervix and in the cervical canal with a small brush or cotton swab. It is examined more closely under the microscope. In this way, the doctor can see whether there are changed cell shapes under the mucous membrane cells. This test is called a cervical swab or cervical swab (PAP test).
Sometimes the external cervix and its surroundings cannot be adequately assessed with the naked eye. Then a vaginal mirror (colposcopy) is necessary: The gynecologist examines the inside of the vagina and the cervix using an illuminated magnifying glass. He can also dab the tissue on the cervix with an iodine solution: healthy and diseased tissue will then show different colors. The gynecologist can then take a tissue sample (biopsy) from suspicious areas. Research in the laboratory shows whether it is actually cervical cancer.
Conization
If the suspicious tissue change is only small, the gynecologist usually carries out a so-called conization: A cone is cut out of the tissue, consisting of the pathologically changed cells and a border of healthy cells all around. The latter is to ensure that no changed cells remain. The removed tissue can be examined for cancer cells in the laboratory.
The conization is not only used to remove suspicious tissue so that it can be examined in detail in the laboratory. It can also be used as a therapy option: A small, demarcated tumor can be completely removed by means of a conization (see below).
HPV test
A test for human papilloma viruses (HPV test) can also be useful when clarifying a possible cervical cancer disease: A smear from the cervix is examined for the presence of HP viruses (more precisely: for their genetic material).
In women over the age of 30, the HPV test can routinely complement the preventive medical check-up for cervical cancer. Women have to bear the costs themselves.
The HPV test does not make sense in younger women because HPV is often found in them, but the infection usually subsides on its own.
Regardless of the woman's age, an HPV test is indicated if the PAP smear gives an unclear result. The cost of the test will then be covered by the health insurance companies.
Further investigations
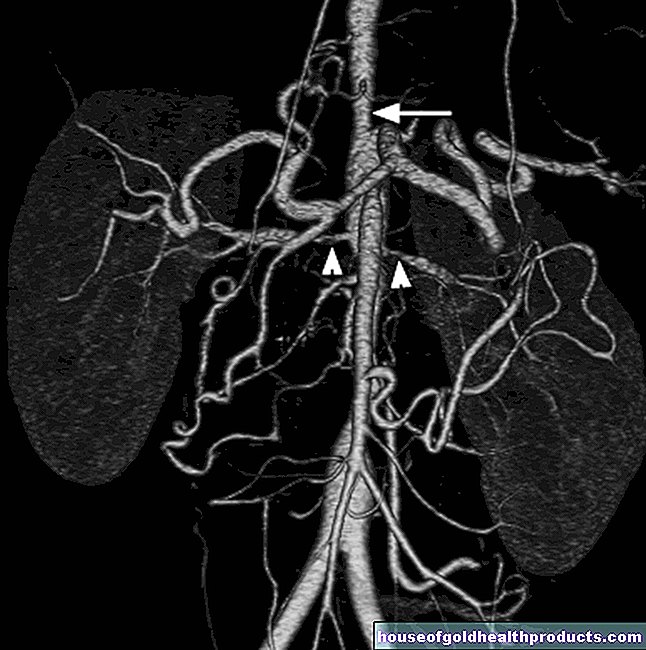
Once the diagnosis of cervical cancer has been made, further examinations are necessary. They should show whether the tumor has already spread to the surrounding tissue and has formed daughter tumors (metastases) in more distant places. For example, an ultrasound examination is suitable for this: On the one hand, the doctor does a transvaginal ultrasound by inserting the ultrasound probe into the vagina. On the other hand, a "normal" ultrasound examination (from the outside) is used to assess the kidneys for any noticeable changes.
Sometimes the doctor also orders a computed tomography (CT) and / or magnetic resonance imaging (magnetic resonance imaging, MRI) scan. This can be used to detect metastases in the pelvis, abdomen or chest. A chest x-ray (chest x-ray) can also reveal metastases in the chest.
If it is suspected that the cervical cancer has spread to the bladder or rectoscopy, a cystoscopy or rectoscopy is necessary. This can be used to detect a possible cancer infestation.
In the case of cervical cancer, so-called surgical staging may also be carried out: As part of an operation, the doctor takes a look at the organs in the pelvis and lower abdomen in order to better assess any possible spread of the tumor. He can take tissue samples from various organs and lymph nodes in order to have them examined for cancer cells in the laboratory.
Sometimes the surgical staging immediately follows the treatment. During the examination, the doctor can decide to cut out the cancerous tumor (usually including the entire uterus). The patient must of course have given her consent in advance.
Staging
Depending on how far the cervical cancer has already spread at the time of diagnosis, doctors differentiate between different stages of cancer. This is important for therapy planning. In addition, the doctor can better estimate the course and prognosis of the cancer based on the stage.
Cervical cancer: treatment
The type of treatment for cervical cancer depends largely on how advanced the disease is. But other factors also influence the therapy planning, for example the general condition of the patient and whether she would like to have children or is already in the menopause. Possible side effects and consequences of the individual therapy methods are also taken into account.
In principle, there are three treatment options for cervical cancer. They can be used individually or in combination:
- surgery
- Radiation therapy
- drug treatment (chemotherapy and targeted therapies)
Some women only have a preliminary stage of cervical cancer (dysplasia). If these cell changes are only slight, one usually waits for the time being because they often regress on their own. The doctor can check this during regular check-ups.
Cervical cancer: surgery
In the early stages of cervical cancer, surgery is the treatment of choice. The goal is to cut out the tumor completely - along with a border of healthy tissue to be on the safe side. The total amount of tissue to be removed depends on the size and spread of the cancerous tumor.
There are several techniques available for surgery for cervical cancer. There are also various access routes to remove the diseased tissue (via the vagina, an abdominal incision or a laparoscopy = laparoscopy).
Conization: The above-mentioned conization can be used for small tumors that can be easily differentiated from healthy tissue. Here, the diseased cells are cut out in a cone shape together with the surrounding healthy tissue. Pregnancy is then still possible, but associated with an increased risk of premature birth. The cervix is more or less unstable after the procedure - depending on how much tissue had to be removed. As a precaution, women should wait some time after conization to have children (more detailed information on this is available from the attending physician).
Trachelectomy: Sometimes conization cannot remove all of the cancerous tissue - a major operation is necessary. However, if the patient still wants to have children, a so-called trachelectomy may be performed: The surgeon removes part of the cervix (up to two thirds) and the inner straps of the uterus. The internal cervix and the body of the uterus remain intact (the internal cervix is connected to the vagina).
Pregnancy after a trachelectomy is associated with an increased risk of complications (such as premature birth). In addition, the child must be delivered by caesarean section. As soon as the woman has completed the family planning, the entire uterus is subsequently removed (hysterectomy).
Hysterectomy: When a woman with cervical cancer no longer wishes to have children, the entire uterus is often removed. The intervention is also necessary when the tumor has already grown deeper into the tissue. The woman is no longer able to conceive after this operation.
If the uterus is removed alone during the procedure, it is called a simple hysterectomy. If the surrounding tissue has to be cut out (neighboring lymph nodes, the upper part of the vagina, etc.), it is a radical hysterectomy. In cervical cancer patients after the menopause, both ovaries and fallopian tubes are usually removed at the same time. In younger women, this is avoided if possible in order to maintain the production of hormones in the ovaries.
The urinary bladder and rectum must also be removed if the cervical cancer has already spread to these organs.
Cervical cancer: radiation therapy
If extensive surgery is not possible (e.g. if the patient's general condition is poor) or if it is refused by the woman, the cervical cancer can alternatively be treated with radiation or a combination of radiation and chemotherapy (radiochemotherapy). Sometimes radiation therapy is also performed after an operation to kill any remaining cancer cells. Then doctors speak of adjuvant radiation.
Two methods are possible with radiation therapy: Either the tumor is irradiated through the skin (percutaneous irradiation). Or the doctor brings the radiation source through the vagina to the tumor. This radiation therapy from within is called brachytherapy.
Radiation treatment for cervical cancer can cause acute side effects. These include, for example, painful irritation of the mucous membrane in the vagina, bladder or intestine, as well as diarrhea and infections. Such symptoms disappear again within a few weeks after the irradiation. In addition, the treatment can cause long-term effects months or years later, some of which remain permanent, such as impaired bladder function, loss of control when defecating, inflammation of the mucous membranes with bleeding or a narrow, dry vagina.
Cervical cancer: chemotherapy
With chemotherapy, the patient is given infusions of medication at regular intervals to prevent the cervical cancer from growing. Because these chemotherapeutic agents (cytostatic agents) work throughout the body, they are also referred to as systemic treatment.
The rapidly dividing cancer cells are particularly sensitive to these drugs. However, the reproduction of rapidly growing healthy cells is also impaired, such as hair root cells, mucous membrane cells and blood-forming cells. This explains the possible side effects of chemotherapy such as hair loss, nausea and vomiting as well as changes in the blood count with an increased susceptibility to infections.
Chemotherapy is usually combined with radiation therapy for cervical cancer (as mentioned above). Sometimes, however, it is also used on its own, for example in the case of a relapse or in the case of daughter tumors far away from the primary tumor in the cervix (distant metastases).
Cervical Cancer: Targeted Therapy
Sometimes cervical cancer is treated with an artificially produced antibody (bevacizumab) that specifically fights the tumor: as soon as the cancerous tumor has reached a certain size, it needs its own, newly formed blood vessels to ensure the supply of oxygen and nutrients. The antibody bevacizumab inhibits a certain growth factor and thus the formation of new blood vessels. The tumor cannot grow any further.
Bevacizumab is given as an infusion. Targeted therapy is only possible in certain cases, namely when the cervical cancer:
- has already metastasized,
- cannot be suppressed with other therapies or
- returns after an initially successful therapy (relapse).
Complementary treatments
Malignant tumors such as cervical cancer can sometimes cause severe pain. Those affected then receive individually tailored pain therapy.
Many patients develop anemia - either from the cancer itself or from treatment (such as chemotherapy). The women affected may receive blood transfusions.
Other side effects of cervical cancer therapy are also specifically treated if necessary. A few examples: Nausea and vomiting, which often occur during chemotherapy, can be relieved with medication. Diarrhea as a result of chemotherapy or radiation therapy can also be stopped with a suitable drug. Radiation therapy for cervical cancer can lead to a dry, narrowed vagina: Lubricants help against uncomfortable dryness during sexual intercourse. A narrowing can be prevented by regularly expanding the vagina with aids for a few minutes.
Diagnosing and treating cervical cancer (or other cancers) can be psychologically stressful. Therefore, patients should receive psycho-oncological care. Psycho-oncologists are specially trained doctors, psychologists or social pedagogues who mentally support cancer patients and their relatives in dealing with the disease.
Cervical cancer: rehab and aftercare
Rehabilitation after cervical cancer (or any other cancer) aims to enable patients to return to their social and professional lives. Various therapists and advisors (doctors, psychologists, physiotherapists, etc.) help the women affected to cope with possible consequences of the illness or treatment and to get physically fit again. Patients can obtain all important information about rehab from their treating doctor and from the social services in the clinic.
The cervical cancer treatment is followed by follow-up care: it includes regular check-ups. These are used to check the success of the treatment and to identify any relapses at an early stage. In addition, the women receive help in coping with the consequences of illness or therapy. Experts recommend the following schedule for follow-up visits:
- For the first three years after treatment, women should have a follow-up visit every three months.
- A follow-up examination every six months is recommended for the 4th and 5th years after completion of treatment.
- From the 6th year onwards, women should have a follow-up examination once a year.
The follow-up examination should consist of the following parts:
- Conversation and advice
- physical examination of the genital organs with palpation of the lymph nodes
- PAP test
In addition, an HPV test, an ultrasound examination of the vagina and kidney and a magnifying glass examination (colposcopy) can be carried out at certain intervals.
Cervical cancer: course and prognosis
The earlier the tumor is discovered and treated, the better the chances of cervical cancer cure:
Early stages can usually be cured. If the tumor is a little further advanced, but can be completely removed surgically, the prognosis is also favorable. In the very advanced stages of cervical cancer and if it relapses, it is much more difficult to cure, but it is still possible. If the cervical carcinoma has already formed daughter tumors (metastases) in other organs, the treatment usually only aims to alleviate the patient's symptoms and to extend the lifespan as much as possible.
Therapy that aims at healing is called curative. If the treatment only serves to make the remaining life of the patient as symptom-free as possible, it is a palliative treatment.
In the last few decades, the chances of recovery from cervical cancer have improved significantly: Today, around 1,540 women in Germany die each year from cervical cancer. 30 years ago there were more than twice as many.
Cervical cancer: prevention
Vaccination against human papillomavirus (HPV) can lower the risk of cervical cancer - after all, these viruses are responsible for most cases of the disease. The Standing Vaccination Commission (STIKO) at the Robert Koch Institute recommends vaccination for all girls between 9 and 14 years of age before their first sexual intercourse. The health insurance companies cover the costs.
Experts advise boys to get vaccinated against HPV too. If they are not infected, they cannot infect their sexual partners either - this protects them from cervical cancer. The vaccination also protects the boys themselves from genital warts and cell changes that can potentially lead to cancer (such as penile cancer).
You can read everything you need to know about the procedure, effects and side effects of the vaccination in the article HPV vaccination.
HPV infection can also be prevented to a certain extent by "safer sex": the use of condoms can prevent infection in about half of all cases. Apart from that, condoms also protect against other sexually transmitted diseases such as HIV or chlamydia.
Adequate genital hygiene and not smoking also help prevent cervical cancer.
Additional information
Books:
- Women and cancer: Help for those affected and their relatives, Christian Dadak and Sigrid Sohlmann, Maudrich, 2011
Guidelines:
Patient guideline "cervical cancer" of the working group of the scientific medical professional societies e. V., the German Cancer Society e. V. and the German Cancer Aid Foundation
Self help:
- German Cancer Research Center - Cancer Information Service: https://www.krebsinformationsdienst.de