Takayasu arteritis
Tanja Unterberger studied journalism and communication science in Vienna. In 2015 she started her work as a medical editor at in Austria. In addition to writing specialist texts, magazine articles and news, the journalist also has experience in podcasting and video production.
More about the experts All content is checked by medical journalists.Takayasu arteritis (also Takayasu syndrome or Takayasu disease) is a rare autoimmune disease in which the main artery (aorta) and its main branches become inflamed. This causes the vessels to constrict and trigger symptoms such as circulatory disorders. The doctor usually treats this with medication (e.g. cortisone). Read more about causes, symptoms, diagnostics and therapy here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. M31

Brief overview
- Description: Takayasu arteritis is a rare immune system disorder in which the main artery and blood vessels become inflamed and narrow over time.
- Causes: The exact cause of Takayasu's arteritis is not yet known. A faulty reaction of the immune system leads to the body's own cells attacking the vessel walls.
- Treatment: With medication (e.g. cortisone, acetylsalicylic acid (ASA), antihypertensive drugs); an operation may be necessary.
- Forecast: Takayasu's disease has not yet been cured. If left untreated, the disease is usually fatal. With therapy, most of those affected are symptom-free in the long term.
- Diagnosis: Talk to the doctor, physical examination (including blood tests, ultrasound, MRI, CT)
- Symptoms: Mostly fever, night sweats, weight loss and body aches. Circulatory disorders of the arms and legs, dizziness, fainting, strokes or high blood pressure are also possible in the further course.
What is Takayasu Arteritis?
Takayasu arteritis (also Takayasu disease or Takayasu syndrome) is a rare autoimmune disease in which the walls of blood vessels become inflamed (vasculitis). The disease is named after the Japanese doctor Mikado Takayasu, who first described the disease in 2008.
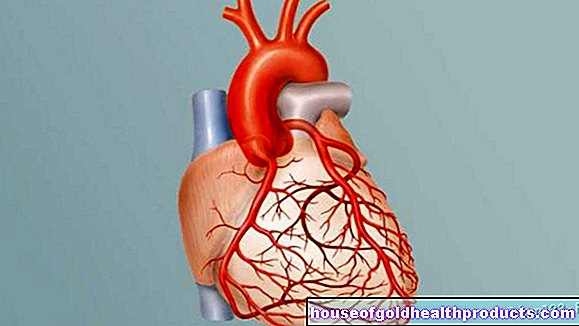
The inflammation occurs particularly in the large arteries (large vessel vasculitis) that carry blood from the heart to the body. These include, for example, the main artery (aorta) and its first vascular branches, which with their other branches supply the head, neck, arms and kidneys. In a few cases, the pulmonary artery, which transports blood from the heart to the lungs, also becomes inflamed.
Takayasu syndrome belongs to the group of so-called primary vasculitis. The collective term refers to inflammatory diseases of the blood vessels for which there is no known underlying disease. Vasculid diseases are rheumatic diseases because they are often associated with pain in the joints or muscles and sometimes with joint swelling.
Who is affected?
Takayasu's arteritis is a very rare disease. Mostly young women under 40 are affected. In the eastern Mediterranean and the Orient (e.g. China, India, Japan, Thailand, Africa, South America) the disease is more common than in western nations. The number of new cases of illness (incidence) in Western Europe is 1: 1,000,000 per year.
Takayasu syndrome usually begins between the ages of 20 and 30. After the age of 40, the disease occurs rather rarely.
How does Takayasu arteritis develop?
The cause of Takayasu's arteritis is not yet known. It is assumed that a hereditary predisposition in combination with an unknown trigger (e.g. environmental factors such as radiation, toxins, stress, hepatitis viruses, infection with the bacterium Staphylococcus aureus) trigger the disease.
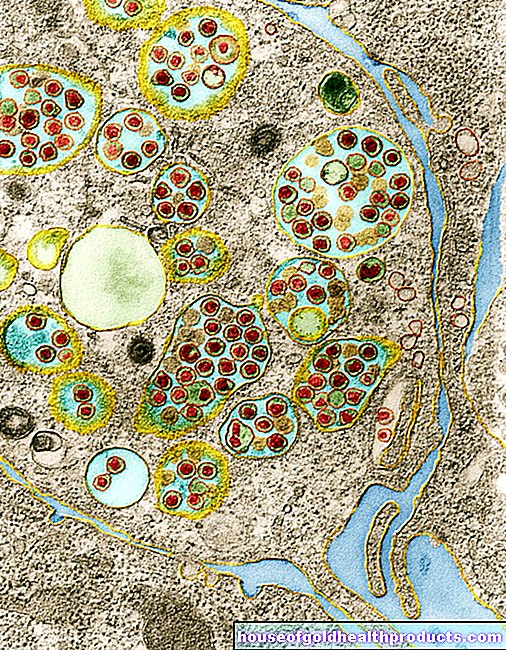
In Takayasu's disease, the body's own immune system attacks its own blood vessels. Nodular scavenger cells of the immune system (macrophages) accumulate on the vessel wall and destroy them (so-called granulomatous inflammation). As a result, the vessel wall scarred and thickened. The vessel narrows over time, which means that the blood no longer flows freely.
As a result, the organs and limbs are no longer adequately supplied with oxygen. Depending on which vessels are affected, Takayasu's disease causes different symptoms.
How do you treat Takayasu's arteritis?
At the beginning of the treatment of Takayasu's arteritis, it is important that the doctor brings the disease under control as quickly as possible in order to avoid short-term consequences of the disease, such as vascular occlusions. He first treats with cortisone and drugs that suppress the body's own defense system (immunosuppressants). This prevents the disease from progressing any further.
cortisone
According to the current guidelines of the German Society for Rheumatology, the doctor usually prescribes high-dose cortisone at the start of therapy. The affected person usually takes the cortisone in the form of a tablet. Doctors recommend 40 to 60 milligrams per day of the cortisone preparation prednisolone as a starting dose for Takayasu arteritis. This drug has anti-inflammatory and analgesic effects. It inhibits many of the processes that go on in the body when there is inflammation.
In the further course of treatment, it is also important to avoid damage caused by the therapy itself. For example, glucocorticoids such as cortisone are very effective and useful in the acute treatment of Takayasu's arteritis, but often lead to long-term effects such as osteoporosis.
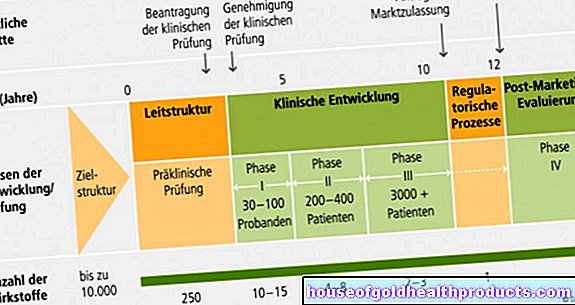
It is therefore important to find the right amount when using cortisone therapy. If the doctor reduces the dose too quickly, the disease threatens to relapse. If he reduces the dose too slowly, more undesirable effects occur than the person concerned should absolutely have to put up with. The target dose after the first twelve weeks of 15 to 20 mg per day is mainly based on experience. There is only limited data from clinical studies on this. In individual cases, the doctor must deviate from these recommendations.
Immunosuppressants
If the person concerned cannot tolerate the cortisone or if the cortisone is insufficient for treatment, the doctor may prescribe other immunosuppressants such as methotrexate or cyclophosphamide as an alternative. These substances inhibit the body's immune defense and prevent the inflammation in Takayasu's arteritis from progressing. They have a very strong effect and are also used in the treatment of cancer (cytostatics).
blood thinner
At the same time, the doctor prescribes “blood thinners” in order to prevent the risk of thrombosis and subsequent heart attacks and strokes. As a rule, the affected person receives so-called platelet aggregation inhibitors such as acetylsalicylic acid (ASA), which ensure that the blood platelets do not clump together. In some cases, the doctor prescribes phenprocoumon, an active ingredient that inhibits blood clotting. Or he gives injections with blood-thinning medication (e.g. heparin).
Antibody therapy
If the person concerned does not respond to therapy with immunosuppressants, the doctor may treat with a so-called TNF-alpha blocker. These active ingredients belong to the group of biologics, genetically engineered drugs (e.g. antibodies). They are specifically directed against certain messenger substances that cause the inflammation on the vessel walls.
surgery
If individual vessels are severely narrowed after years of illness, the doctor may recommend an operation. In the early stages of Takayasu's arteritis, the doctor usually only uses surgery if there is a threat of serious complications. This is the case, for example, if a bulging of the main artery (aortic aneurysm) threatens to tear or if an artery supplying the brain is severely narrowed.
Various surgical and minimally invasive procedures are available to make the blood vessels permeable again. These include balloon dilation, the insertion of a stent or a bypass operation.
Balloon dilation
During balloon dilation (percutaneous coronary intervention; PCTA for short), the doctor guides a very thin and flexible wire (guide wire) to the narrowed vascular site. Using this guide wire, he introduces a balloon catheter (a tube to which a folded, inflatable balloon is attached) and pushes it further to the affected area. There he inflates the balloon, which causes the blood vessel to expand and expand again. During the procedure, the person concerned is usually conscious, but the doctor first anaesthetizes the puncture site of the catheter.
Stent
To stabilize the vessel and keep it open, the doctor sometimes inserts a stent (wire tube made of metal or plastic) after balloon dilation. To do this, the doctor pushes a catheter with the stent into the affected vessel over the guide wire and places it there. Once the stent has been set, it remains in this form in the blood vessel and ensures that the blood flows again unhindered at the former constriction.
Bypass surgery
If the blocked or narrowed artery does not remain open despite balloon dilation and stent, bypass surgery is used. During this operation, the doctor "bypasses" the narrowed or blocked blood vessel with the help of a bypass. To do this, he uses healthy pieces of blood (mostly from the chest wall or from the veins of the lower or upper thighs) and sews them behind the affected blood vessel. This ensures that the tissue behind the blocked areas is again adequately supplied with blood and nutrients. In most cases, the operation takes place under general anesthesia.
Serious complications of Takayasu's arteritis such as a heart attack or a stroke can be largely avoided with the right therapy.
Is Takayasu Arteritis Curable?
Takayasu's arteritis has not yet been cured. If left untreated or recognized too late, the disease is usually fatal. In this case, those affected usually die of a stroke or a heart attack. However, if the doctors recognize the disease early on and carry out consistent treatment, almost all those affected are symptom-free in the long term.
According to a larger study from Japan, the disease does not get worse in two thirds of those affected with the right therapy. Serious complications (e.g. heart attack, stroke) occur in only a quarter.
A prognosis in the long term depends on how much the blood pressure rises due to the disease and how much the vessels near the heart (aorta, pulmonary artery, coronary vessels) are damaged. It is therefore not generally possible to predict whether Takayasu arteritis will reduce the life expectancy of those affected.
The earlier the doctor recognizes and treats the disease, the lower the risk of permanent damage.
How does the doctor make a diagnosis?
If Takayasu arteritis is suspected, it is important to have a doctor diagnose it as early as possible. Doctors recommend starting therapy quickly so that the disease does not progress and does not affect the person's everyday life. The first point of contact here is the family doctor. If he suspects that Takayasu arteritis is behind the symptoms, he refers the person affected to a specialist in internal medicine (internist) specializing in vascular diseases (angiologist or phlebologist) or rheumatology (rheumatologist).
Since the symptoms of Takayasu arteritis are usually quite unspecific at the beginning of the disease and the disease itself is very rare, it is important that the doctor examines the person concerned carefully. To do this, the doctor first conducts a detailed discussion (anamnesis) with the person concerned. He will then perform a physical exam on him.
Talk to the doctor
The doctor asks the person concerned, among other things:
- What symptoms do you have (e.g. unwanted weight loss, night sweats, visual disturbances, pain in the arms)?
- When did the complaints arise?
- Do you have any previous illnesses (e.g. rheumatism, arteriosclerosis, high blood pressure)?
- What are your lifestyle habits like? Do you exercise regularly? What is your diet like? Do you smoke?
Physical examination
The doctor will then do a physical exam. Among other things, he measures blood pressure and pulse, listens to the heart with a stethoscope and examines the blood. Imaging methods are often used to diagnose Takayasu's arteritis, for example an ultrasound examination (sonography), computed tomography (CT) or magnetic resonance imaging (MRI).
Ultrasonic
During an ultrasound examination of the blood vessels (color duplex sonography), the doctor can see whether the vessel wall is narrowed or inflamed. He also uses ultrasound to determine the direction in which the blood flows in the vessels and how fast the blood flows through the vessels (flow speed). The latter gives the doctor information about whether there are constrictions or obstructions in the vessels.
The doctor usually uses an ultrasound device to examine the vessels in the neck, abdomen, arms, pelvis and / or legs. The ultrasound examination usually takes between ten and 30 minutes and is completely painless for the person concerned.
In some cases, the doctor inserts an ultrasound probe into the esophagus (transesophageal echocardiography, TEE) to examine the vessels near the heart.
Angiography
Angiography uses imaging techniques such as x-rays, magnetic resonance imaging (MR angiography), or computed tomography (CT angiography) to visualize blood vessels. In this way, the doctor can diagnose changes in the blood vessels caused by Takayasu's arteritis. To do this, he injects contrast agent into the blood vessel, which makes the interior of the vessel visible. The contrast medium is usually a water-clear, colorless liquid that contains iodine. The resulting image is called an angiogram or arteriogram. The doctor then recognizes whether there are any bulges and whether the arterial wall has changed (e.g. narrowed).
Blood test
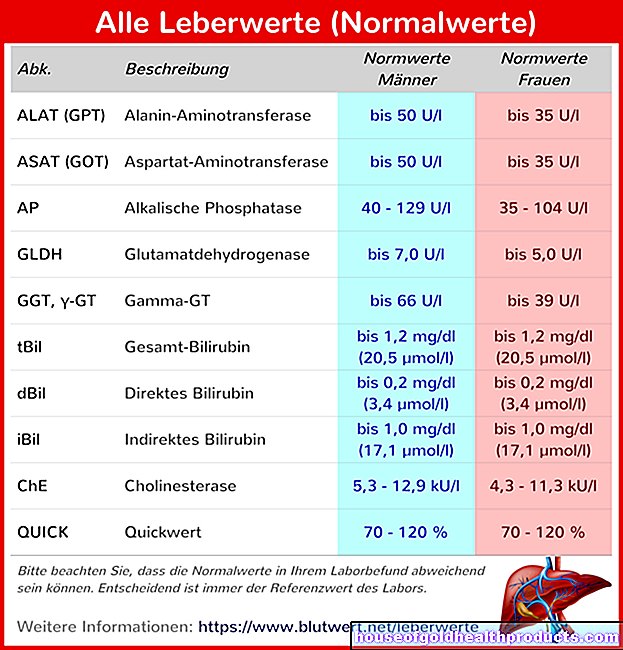
The doctor will also examine the person's blood.If, for example, the sedimentation rate (ESR) is greatly increased, this is an indication of an inflammatory disease such as Takayasu arteritis. The ESR indicates how quickly the red blood cells in a blood sample sink in a special tube within an hour.
Likewise, in Takayasu disease, the number of white blood cells increases (leukocytosis) while the number of red blood cells decreases (anemia). However, this is also the case with other inflammations and infections, so that the blood test alone does not allow a conclusive diagnosis to be made.
ACR criteria
The doctor makes the diagnosis based on the results of all examinations. This is usually done using the so-called ACR criteria (ACR stands for American College of Rheumatology). If at least three of the criteria are met, it is very likely Takayasu arteritis:
- The person concerned is under 40 years old.
- Circulatory disorders occur in the arms and / or legs, e.g. limping (claudication) or muscle pain when the person is moving.
- The person has a weak pulse (less than 60 beats per minute) in the main artery of the arm (brachial artery).
- The systolic blood pressure between the two arms differs by more than 10 mmHg (systolic = the blood pressure when the heart muscle contracts and oxygen-rich blood pumps into the vessels).
- There are flow noises of the blood above the main artery (aorta) or the artery under the collarbone (subclavian artery) audible with the stethoscope.
- Changes in the arteriogram (e.g. vascular changes in the main artery) can be determined.
What are the symptoms?
The symptoms arise at the beginning of the disease due to the inflammation itself. Later there are other symptoms, triggered by the narrowed blood vessels.
When Takayasu arteritis begins, general and unspecific inflammatory reactions of the body usually occur. Those affected usually feel very sick. They are exhausted and weak, have no appetite, and report joint and muscle pain. The most common symptoms are:
- Exhaustion
- Mild fever (around 38 degrees Celsius)
- Unintentional weight loss
- Night sweats
- Loss of appetite
- weakness
- Muscle and joint pain
These early symptoms do not occur in every person affected. It is possible that symptoms will not show up until years later, when the disease has already progressed.
If the disease is already advanced, chronic complaints arise. These develop because the vessels constrict over time and the organs and limbs no longer supply enough blood. The symptoms that arise depend on the artery affected. The most common symptoms of advanced Takayasu arteritis include:
- Circulatory problems in the arms and / or legs
- Dizziness (vertigo)
- Fainting spells
- Visual disturbances
- High blood pressure (hypertension)
- Stroke (cerebral insult)
- Heart attack (myocardial infarction)
- Aneurysm (balloon-like bulging of the vessels)
Circulatory disorders
In principle, with Takayasu arteritis it is possible that the entire main artery and all of its side branches from the heart to the groin area are inflamed. However, the most common damage is the arms, and secondarily the arteries that supply the brain with blood.
Circulatory disorders in the arms (e.g. if the artery under the collarbone is narrowed) become noticeable when pain in the arms occurs when lifting light objects. If arteries in the brain are affected, people with Takayasu arteritis often have headaches, visual disturbances, even fleeting visual field losses and difficulty concentrating.
Dizziness and fainting spells
Due to a vascular connection between the arm and the brain, it is also possible in Takayasu arteritis that blood is drained from the brain if the subclavian artery is narrowed if the person concerned puts a lot of strain on their arm (e.g. by lifting heavily). To compensate for this, the narrowed clavicle artery taps into the vertebral artery (arteria vertebralis), which actually conducts blood into the brain (subclavian steal syndrome). The collarbone artery thus draws blood from the vertebral artery and thus from the brain. Dizziness and fainting spells are often the result.
In addition, the pulse on the wrist is often weakened or can no longer be felt at all. The blood pressure is often different in both arms. If the arteries in the carotid artery are affected, people with Takayasu syndrome often also have pain on the side of the neck.
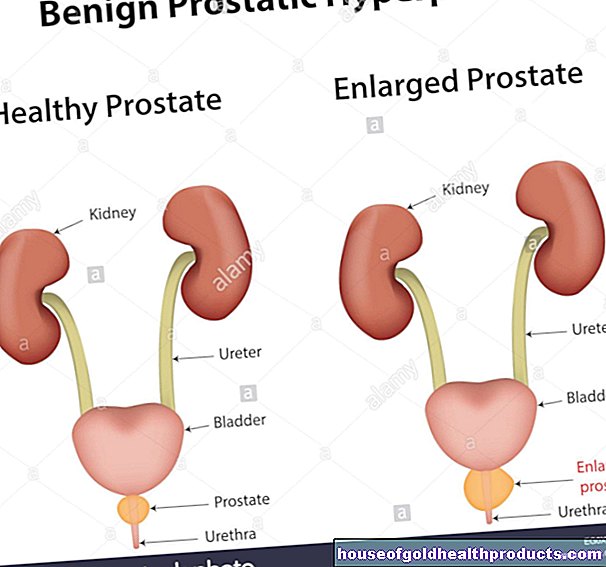
high blood pressure
If the kidney arteries become inflamed and narrow, blood pressure increases (hypertension). If the circulatory disorders persist for a long time or if the kidney vessels become completely blocked, this also restricts the function of the kidneys (renal insufficiency).
Strokes and heart attacks
If the vessels are inflamed, there is also the risk that they will narrow significantly over time and even close completely (arterial stenosis). The affected areas are then no longer adequately supplied with oxygen and nutrients, and the tissue in this area dies. As a result, if Takayasu arteritis is untreated, strokes (caused by narrowed blood vessels in the brain) or heart attacks (caused by narrowed blood vessels in the heart muscle) often occur.
Aneurysm
Since there is high blood pressure in the vessels near the heart, the vessels expand increasingly when the vessel walls are weakened as a result of the inflammation. Sometimes this causes bulges on the vessel wall (aneurysms). If such an aneurysm ruptures, life-threatening internal bleeding usually occurs. The dangerous thing about these dilated vessels is that they usually do not cause any symptoms.
More symptoms
People with Takayasu arteritis also report various changes to the skin. Often their subcutaneous fatty tissue is inflamed (panniculitis). This causes nodules to form under the skin on arms and legs, in the chest and stomach area, as well as on the face and buttocks. Patients with Takayasu arteritis sometimes have nettle-like rashes (urticaria).
If you find it difficult to breathe and have pain in your chest or arms, see a doctor immediately!
Tags: travel medicine pregnancy anatomy