Benign prostatic hyperplasia
Marian Grosser studied human medicine in Munich. In addition, the doctor, who was interested in many things, dared to make some exciting detours: studying philosophy and art history, working on the radio and, finally, also for a Netdoctor.
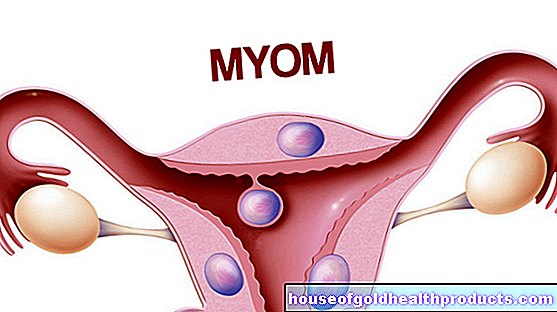
More about the experts All content is checked by medical journalists.Benign prostatic hyperplasia (BPH) refers to the benign enlargement of the prostate gland (prostate). Older men are particularly affected. With increasing prostate enlargement, there are usually unpleasant symptoms when urinating. Lighter stages of benign prostatic hyperplasia are first treated with medication, and if there are pronounced symptoms or complications, surgery is performed. Read more about benign prostatic hyperplasia here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. N40

Benign prostatic hyperplasia: description
Benign prostatic hyperplasia (BPH) describes a benign enlargement of the prostate. “Benign” means that although there is an increase in the number of cells in the prostate, it is not as aggressive and uncontrolled as with malignant growth (cancer). The increasing tissue in benign prostatic hyperplasia does not grow into other structures and does not spread. So there are no daughter tumors (metastases) as in prostate cancer.
Benign prostatic hyperplasia is neither a form of cancer nor a precursor to it. Nevertheless, the increase in volume of the organ results in increasing complaints for those affected.
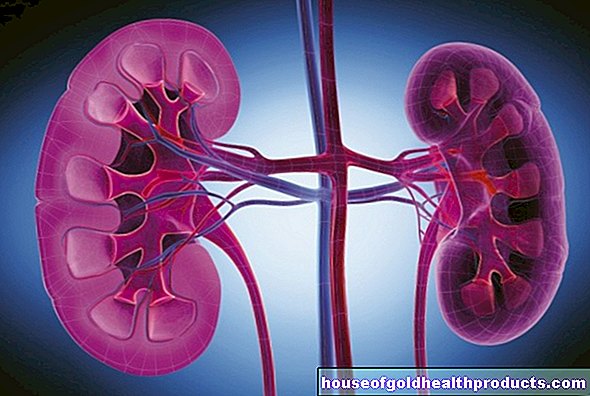
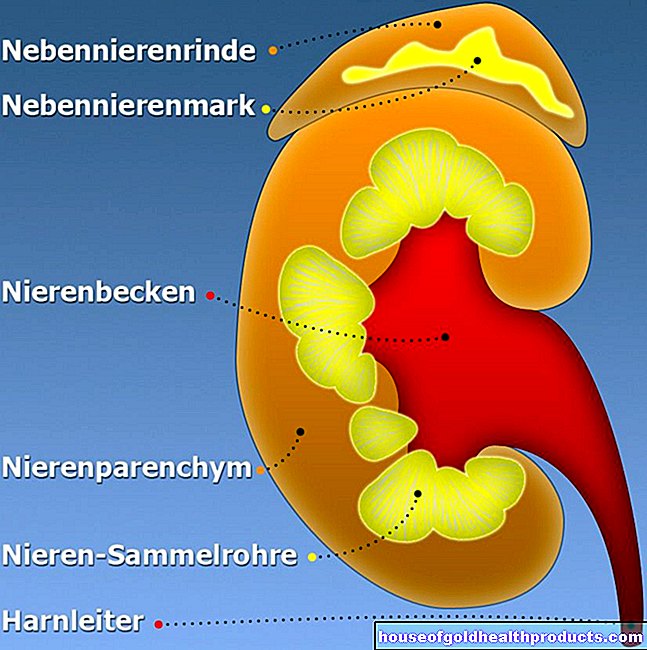
Location and anatomy of the prostate
The prostate gland resembles a chestnut in shape and size. It is located just below the urinary bladder and in front of the rectum. In the normal state it weighs between 20 and 25 grams, in contrast, in the case of pronounced benign prostatic hyperplasia, it weighs up to 150 grams.
The uppermost section of the urethra runs through the prostate. In addition, the vas deferens (transports the sperm from the testes) and the duct of the vesicle gland (produces secretion for the ejaculate) unite in the prostate to form the so-called injection canal. This also opens into the urethra within the prostate. The vas deferens, vesicle glands and tubules are created in pairs.
The prostate can be divided into three zones from the inside out:
The innermost zone (periurethral mantle zone or transition zone) directly surrounds the urethra. There are small secretory glands in it. The next layer is the “inner zone”. It makes up about a quarter of the total mass of the prostate. The two small spray ducts run in it. The outermost layer (outer zone or peripheral zone) also contains secretion-producing glands. They account for almost three quarters of the weight of the prostate. On the very outside, the prostate is enclosed by a tough layer of connective tissue (capsule).
Function of the prostate
The prostate gland consists of many smaller glands that produce a secretion that protects the sperm and stimulates movement. It makes up 30 percent of the ejaculate and is released into the urethra. In addition, the so-called prostate-specific antigen (PSA) is formed in the prostate - an enzyme that makes the sperm liquid.
Layers of connective tissue and smooth muscles lie between the glands of the prostate. With the help of the muscle cells, the prostate can rhythmically contract during orgasm and thus expel the ejaculate.
What happens with benign prostatic hyperplasia?
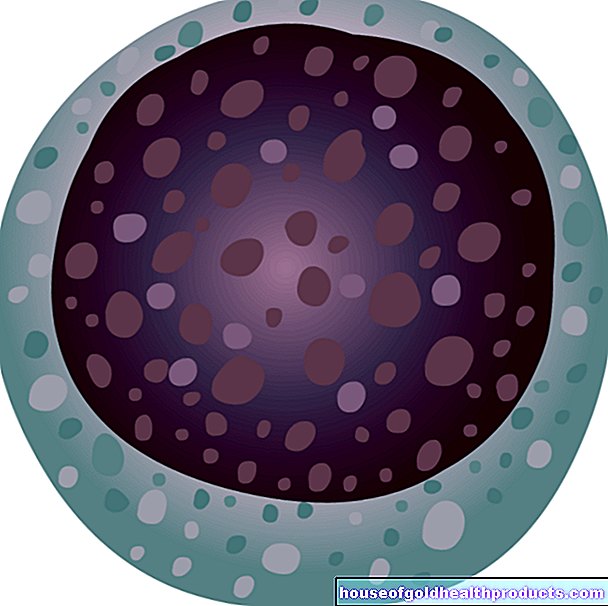
In medicine, the term “hyperplasia” describes the excessive increase in the number of cells in a tissue. In the case of prostate hyperplasia, this primarily affects the cells of the connective and muscle tissue located between the glands, but also the gland cells themselves. According to the current state of research, the increase in the number of cells is due to the fact that natural cell death (apoptosis) slows down (and not through an increased cell proliferation).
The increase in the number of cells in benign prostatic hyperplasia can only be seen in the periurethral mantle zone. The outer zone of the prostate gets more and more distressed by the growing transition zone until it only appears as a thin layer. Since there are many glands in the outer zone, this also explains why the prostate's secretory capacity decreases somewhat in benign prostatic hyperplasia, although there are more cells overall.
In contrast to benign prostate enlargement, prostate cancer has uncontrolled growth in the outer zone, while the transition zone is not affected.
BPO, LUTS, BPS, prostate adenoma - terms related to prostate hyperplasia
As described above, the term benign prostatic hyperplasia (BPH) only describes the pure increase in size or volume of the prostate, but not associated symptoms. Some terms that often appear in connection with benign prostate enlargement and should be briefly explained here therefore seem a bit confusing.
Benign prostate obstruction (BPO): Benign prostatic hyperplasia can cause the so-called bladder outlet resistance to increase. This term describes the resistance that the bladder has to overcome in order to expel the urine that has collected in it out of the body via the urethra. A certain amount of resistance is normal and necessary to prevent the constant, uncontrolled dripping of urine. In the case of prostatic hyperplasia, the resistance can be abnormally increased because the urethra is narrowed by the enlarged prostate gland. The possible consequence is problems urinating. In this case, doctors speak of benign prostate obstruction, or BPO for short.
Lower Urinary Tract Symptoms (LUTS): Many symptoms of benign prostatic hyperplasia (such as frequent urination or a weakened urine stream) affect the lower urinary tract, i.e. the bladder and urethra. This is why these complaints are grouped under the term “lower urinary tract symptoms”. In English usage one says "Lower Urinary Tract Symptoms", the abbreviation for this is LUTS.
Benign prostate syndrome (BPS): If there is benign prostatic hyperplasia and there is also an obstruction (BPO) and symptoms in the lower urinary tract (LUTS), this overall complex is referred to as "benign prostatic hyperplasia" (BPS). In the case of BPH in need of treatment, it is ultimately always BPS, since the symptoms are decisive for therapy and not the mere enlargement of the prostate.
Prostate adenoma: The term prostate adenoma is sometimes used synonymously for benign prostatic hyperplasia, although that is actually incorrect. In medicine, an adenoma describes an excessive benign growth of cells in the mucous membrane or glandular tissue. In benign prostatic hyperplasia, it is not only the gland cells that are affected by the increase in the number of cells, but also connective tissue and muscle cells. Nevertheless, the term prostate adenoma is often used as a synonym for benign prostatic hyperplasia.
Benign prostatic hyperplasia: frequency
Benign prostatic hyperplasia is the most common urological disease in men. It is also a typical phenomenon of old age. While young men usually have no problems with their prostate gland, men over the age of 50 in particular see a urologist because they have difficulty urinating. The enlargement of the prostate, which is pathological in the medical sense, can occasionally be detected earlier (from around the age of 35), but then usually has no disease value because symptoms do not appear at first.
Benign prostatic hyperplasia is relatively common from a certain age, but only some of those affected experience the typical symptoms. About every second man between 50 and 60 has an enlarged prostate. However, only 10 to 20 percent of men in this age group show clinically relevant symptoms. In the 60 to 69 year olds, on the other hand, around 70 percent have an enlarged prostate and 25 to 35 percent have noticeable symptoms.
Benign prostatic hyperplasia: symptoms
You can read about the symptoms and complications a benign prostate enlargement can trigger in the article Benign Prostatic Hyperplasia - Symptoms.
Benign prostatic hyperplasia: causes and risk factors
Ultimately, the causes of benign prostatic hyperplasia have not yet been adequately clarified. It is clear that certain factors play a role. The exact relationships and processes that lead to benign prostate enlargement are still the subject of research.
Hormones
What is certain is that the male hormone balance plays an essential role in the development of benign prostatic hyperplasia. The presence of male sex hormones (androgens), especially testosterone, is necessary for BPH to develop at all. Accordingly, castrated men cannot develop benign prostatic hyperplasia: because they no longer have testicles (the main sites of testosterone production), they only have very small amounts of the hormone.
Testosterone seems to cause the transition zone of the prostate to grow in men with increasing age. The exact processes behind it have not yet been conclusively clarified. The testosterone does not work directly on the prostate, but is first converted into a more effective form - the so-called dihydrotestosterone (DHT) - in the cells within the prostate gland. The enzyme that enables this conversion is called 5α-reductase. Dihydrotestosterone is not only produced in the prostate and its effect is not limited to this organ, but it is essential for the development of benign prostatic hyperplasia.
It is assumed that not only testosterone (or dihydrotestosterone), but also female sex hormones (estrogens) play a certain role in the development of benign prostatic hyperplasia. You have to know that men also have estrogens, albeit in smaller amounts than women. Conversely, women also have low levels of testosterone and other androgens in their blood. With increasing age, the testosterone level decreases in men, while the estrogen level remains about the same or even increases. This leads to a (relative) increase in estrogens, which can obviously promote BPH.
Because oestrogens are also partly formed in fat cells, being very overweight should be regarded as a risk factor for benign prostatic hyperplasia.
Changes in the extracellular matrix
In addition to hormones, there is another aspect that is suspected of contributing to the development of benign prostate enlargement: an altered effect of the so-called extracellular matrix (ECM) of the prostate on the cells of the organ. The area between the cells of a tissue is generally referred to as the extracellular matrix. If certain changes take place here, as a consequence, for example, more growth factors can be bound to the ECM and cause cells to multiply. Such growth factors can also be increasingly produced by the body and stimulate cell division in the prostate tissue or prevent the natural death of cells. This can promote benign prostatic hyperplasia.
Genetic factors
Genetic factors play a subordinate role in benign prostatic hyperplasia. The likelihood of a genetic component causing BPH is higher when prostate enlargement becomes clinically relevant at a relatively young age. If benign prostatic hyperplasia has to be operated on before the age of 60, for example, then 50 percent of the time it has familial, i.e. genetic causes. In men over the age of 60, on the other hand, only about 9 percent of cases with BPH requiring treatment are genetic.
Benign prostatic hyperplasia: examination and diagnosis
The different examination methods serve on the one hand to confirm the diagnosis of benign prostate enlargement. On the other hand, it is important to rule out other diseases that can cause symptoms (such as frequent urination or an interrupted urine stream) as benign prostatic hyperplasia.
In general, individual test results usually do not provide sufficient evidence of benign prostatic hyperplasia. The diagnosis can only be made when several findings are viewed together.
Collection of the medical history (anamnesis)
In a detailed discussion with the patient, the doctor asks about the exact complaints. He also asks about any previous illnesses and previous interventions that could be the cause of the complaints.
For example, a narrowing of the urethra can not only be due to prostatic hyperplasia, but also to a previous inflammation or a catheter. Diseases such as diabetes mellitus, Parkinson's disease or cardiac insufficiency (heart failure) can sometimes also resemble the symptoms of benign prostatic hyperplasia. In some cases, certain drugs (anticholinergics, antidepressants, neuroleptics) trigger the symptoms.
Assessment of the severity of the symptoms
In order to be able to evaluate the extent of the symptoms objectively, the doctor uses the "International Prostate Symptoms Score" (IPSS) as an aid. The patient is asked about a total of 7 typical symptoms of BPH (such as residual urine sensation, nocturnal urge to urinate, etc.): On a scale from 0 to 5, he should indicate how strongly he feels the individual complaints. The more pronounced a symptom, the higher the number of points awarded. The total result can therefore be a maximum of 35.
It should be noted that the IPSS is not a method for diagnosing benign prostatic hyperplasia. It only serves to determine the intensity of certain symptoms that can occur both with benign prostate enlargement and with other diseases.
The digital rectal exam (DRE)
The most important physical examination to clarify prostatic hyperplasia is the so-called digital rectal examination, or DRU for short. The doctor inserts his finger (lat. Digitus) into the patient's rectum and palpates the prostate, which is located directly in front of the rectum.
If there is benign prostatic hyperplasia, then this can be determined with the help of the DRE, provided that the prostate has already enlarged sufficiently. The prostate then usually feels plump, elastic and smooth. In contrast, if the prostate is enlarged due to cancer, it usually appears rock-hard and uneven.
The DRU is only used as a rough guide; its result always depends on the experience of the doctor. Under no circumstances can the diagnosis of benign prostatic hyperplasia be made based on the findings of DRE.
More physical exams
In addition to the DRU, certain reflexes, possible nerve failures and the function of the sphincter are also checked during the physical examination to clarify benign prostatic hyperplasia.
Urine and blood tests
Laboratory diagnostics can also provide important information for clarifying benign prostatic hyperplasia. On the one hand, the urine status is checked: The urine is checked for possible infections.
On the other hand, certain laboratory parameters are collected. This includes the prostate-specific antigen (PSA), which can often be elevated in prostate cancer and should therefore be determined to rule out malignant prostate enlargement.
In addition, the blood concentrations of urinary substances (retention parameters) are measured in order to identify kidney damage and uremia in good time.
Ultrasound (sonography)
The ultrasound examination is an important method to clarify relevant questions about BPH. With their help, statements can be made about the amount of residual urine and the size of the prostate. In addition, the thickness of the detrusor can be determined using ultrasound and possible complications such as bladder stones or pseudodiverticula can be identified.
As a rule, the ultrasound examination is carried out transrectally, i.e. via an examination device (transrectal ultrasound, TRUS) inserted into the rectum. The remaining amount of urine can also be easily scanned through the abdomen (transabdominal ultrasound).
Urinary stream measurement (uroflowmetry)
The urine stream is determined with the help of so-called uroflowmetry. The patient urinates in a special funnel, which can use sensors to measure how much urine flows through it per unit of time. In order for this examination to be really meaningful, at least 150 milliliters should be urinated.
A normal urine flow is approximately 20 milliliters per second (ml / s). Anything below 10 ml / s, on the other hand, is highly suspicious of a narrowing of the urethra, for example due to benign prostatic hyperplasia. Uroflowmetry is relatively easy to perform and inexpensive.
Other apparatus-based examination procedures
There are other apparatus-based methods that are not necessarily used as standard, but only in certain cases.
Urethrocystometry (urodynamics), for example, allows statements to be made about the pressure that prevails in the urinary bladder during micturition. This helps to differentiate an obstruction caused by prostatic hyperplasia from a pure weakness of the bladder muscle (detrusor weakness).
In an excretory urogram (urography), contrast agent is administered to the patient through a vein and then an X-ray of the lower abdomen is made. The kidney excretion and the urinary drainage can be assessed.
In contrast, with a urethrogram, the contrast agent is injected through the urethra into the urinary bladder, which allows an assessment of the urethra.
Occasionally, a cystoscopy is used to clarify benign prostatic hyperplasia.
In order to be able to reliably differentiate a benign prostate enlargement from a malignant one, a small tissue sample must be taken from the prostate gland via the rectum and then carefully examined.
Benign prostatic hyperplasia: treatment
Benign prostatic hyperplasia does not necessarily require treatment. As long as it does not cause any symptoms, it is often sufficient to wait and see how the disease is progressing. With an IPSS above 7 or general distress in the patient, however, treatment of the benign prostate enlargement is usually started. “Treatment” usually means the use of medication. Surgical procedures are only considered if the symptoms increase or if there are complications from the enlarged prostate.
Drugs for benign prostatic hyperplasia
In the case of benign prostate enlargement in stage I and mild forms of BPH in stage II according to Alken (described in the article), drug treatment is usually sufficient. Various groups of drugs are available, some of which can also be combined with one another.
Herbal preparations (phytopharmaceuticals): There are a number of herbal medicines that can be used to treat benign prostatic hyperplasia with mild symptoms. These include, for example, preparations based on saw palmetto, rye, nettle root, African plum and pumpkin seeds. The way in which the various plant substances work is different: some inhibit the enzyme 5α-reductase or certain growth factors, for example, while others promote natural cell death. Many phytopharmaceuticals also contain so-called beta-sitosterones - substances that inhibit male sex hormones, i.e. have an anti-androgenic effect.
Herbal medicines are available without a prescription and are usually very low-risk. Many patients therefore prefer them to other drugs. The therapeutic effectiveness of pumpkin seeds and Co. has not yet been adequately proven by studies; especially the long-term effect is questionable. In the United States, phytopharmaceuticals for the treatment of benign prostatic hyperplasia have been banned for many years because there were concerns that they would discourage patients from further investigating BPH.
α-blockers: The α-blockers (more precisely: α1-adrenoceptor antagonists) ensure that the muscles in the prostate and urethra relax, which improves the flow of urine. This is possible because α-blockers prevent the accumulation of certain messenger substances on receptors in the muscles, which would otherwise trigger a contraction of the muscle cells. However, α-blockers have little influence on the size of the prostate, which is why the mechanical flow obstruction from the bladder is only slightly influenced.
Originally, α-blockers were not developed for the treatment of benign prostatic hyperplasia, but as antihypertensive drugs. This explains why they sometimes have cardiovascular side effects. In addition, dizziness, headaches, fatigue and swelling of the nasal mucosa sometimes occur. Classic active ingredients from the group of α-blockers are, for example, alfuzosin, doxazosin, tamsulosin and terazosin.
5-α-reductase inhibitors: The 5-α-reductase inhibitors block the function of the enzyme 5-α-reductase and thus the conversion of testosterone into dihydrotestosterone. In this way, the essential growth-stimulating factor in benign prostatic hyperplasia is inhibited - the prostate does not enlarge any further; it may even shrink again. However, it can take up to a year for the patient to notice a relevant improvement in symptoms.
The two active ingredients used that block 5-α-reductase are called finasteride and dutasteride. Their typical side effects include loss of libido, impotence, and a decrease in male body hair.
Phosphodiesterase inhibitors (PDE inhibitors): A blockade of the enzyme phosphodiesterase has a similar effect to the inhibition of α-reductase in benign porstatic hyperplasia: the muscles of the urinary bladder and urethra relax, which makes micturition easier. In addition, PDE inhibitors such as tadalafil have a positive influence on erectile dysfunction (impotence), which can occur as part of an enlarged prostate.
Anticholinergics: These active ingredients have a dampening effect on the bladder muscle (detrusor). They are used against the irritative symptoms of benign prostatic hyperplasia, such as the imperative to urinate. In the case of pronounced obstructive symptoms, the use of anticholinergics must be carefully considered, because a weak detrusor muscle can then even be counterproductive.
Surgical procedures for benign prostatic hyperplasia
Once the symptoms have reached a certain severity, the mere use of medication is no longer sufficient. Then surgery is the treatment of choice for benign prostate enlargement. Not all operations are the same: There are many different surgical procedures that can be used for BPH. The most important are described below. Which method is ultimately used always depends on the individual case.
TURP: The standard procedure in the surgical treatment of benign prostatic hyperplasia is "transurethral resection of the prostate" (TURP). Similar to a cystoscopy, a small tube is inserted into the urethra. It has a tiny camera and a metal loop through which electrical current flows. With the help of the loop, the enlarged prostate tissue is removed in layers. Thanks to recent developments in the area of TURP, side effects are rare.
TUIP: A modification of TURP is the “transurethral incision of the prostate” (TUIP). The technique is the same, except that no prostate tissue is removed, just incised, at the transition between the bladder neck and the prostate. This gives the urethra more space. The TUIP is mainly used in benign prostatic hyperplasia when the prostate gland is not yet too large.
TUMT: “Transurethral microwave therapy” (TUMT) also takes place via the urethra. Here microwaves heat the prostate tissue to 70 degrees Celsius and thereby destroy it. As a result, the organ shrinks. To prevent damage to the urethra, it is cooled by flushing in liquid during TUMT.
Laser procedures: Another possibility to treat benign prostatic hyperplasia are laser procedures (ILC, HoLEP). The prostate tissue is destroyed or cut out and ablated by laser beams. Above all, the HoLEP process is considered to be on a par with TURP. However, it is difficult to learn and therefore requires a lot of experience.
Open surgery: If the prostate is already very large or there are certain complications, it sometimes makes sense to openly operate on benign prostatic hyperplasia. One then speaks of a prostate enucleation. The surgeon opens the bladder and removes the prostate through it.
Benign prostatic hyperplasia: disease course and prognosis
Unless treated, benign prostatic hyperplasia usually progresses slowly. With the help of medication, however, the process can often be stopped and in some cases the size of the prostate gland can even be reduced.
If the medication does not work sufficiently or if the prostate hyperplasia is too pronounced at the time of diagnosis, surgery usually helps.
The biggest risk factors for benign prostate enlargement include being overweight and smoking. Regular exercise and sport, on the other hand, have a positive effect.A healthy lifestyle is the best way to prevent benign prostatic hyperplasia.
Tags: laboratory values magazine pregnancy birth