Drug-induced headache
Sophie Matzik is a freelance writer for the medical team.
More about the experts All content is checked by medical journalists.Drug-induced headache is a form of headache that results from overuse of pain relievers. The only treatment option is to stop taking the appropriate medication. After successful withdrawal, those affected have the chance to remain symptom-free in the future. Read everything you need to know about drug-induced headache here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. F55
Drug-induced headache: description
Drug-induced headache (MIKS) occurs when people take excessive pain medication due to a primary type of headache (such as tension headaches or migraines). Since drug-induced headache can be traced back to a specific cause, doctors classify it as one of the so-called secondary forms of headache.
How common drug-induced headache is can so far only be estimated due to insufficient studies. Scientists assume that around 0.2 to 1 percent of the population suffers from it, in Germany that would be 800,000 people. Women are about 4 times more likely to be affected than men. The reason for this is believed to be that women generally suffer from headaches more often than men and therefore resort to (headache) remedies more often. It is important that drug-induced headache is not a disease in the strict sense of the word. Rather, it is a result of incorrect medication intake.
Drug-induced headache: symptoms
A distinction is made between two forms: acute and chronic drug-induced headache. The acute variant usually occurs immediately or only a few hours after taking a certain drug. The classic symptom here is a pulsating, migraine-like headache in the forehead and temples. The symptoms are aggravated by physical activity.
When doctors speak of “drug-induced headache” they usually mean the chronic form. This becomes noticeable through a dull, oppressive feeling in the head. It is usually a constant headache, which means that it starts in the morning when you get up and is present throughout the day.
Chronic drug-induced headache occurs in those affected for at least 15 days a month and is sometimes accompanied by symptoms such as nausea or vomiting. Some patients also suffer from an increased sensitivity to noise. Others are irritable or feel defeated. Migraine attacks may continue to occur in people who primarily suffer from migraines and therefore take excessive pain medication.
Drug-induced headache and chronic tension headache are difficult to distinguish due to the similarity of symptoms. The most significant difference is that a drug-induced headache is always caused by the overuse of pain relievers.
Drug-induced headache: causes and risk factors
Drug-induced headache is caused by various drugs. A distinction is made between drugs that are known for their headache-causing side effects or that have an explicit pain-relieving effect. However, this effect can be lost with continuous use and trigger a drug-induced headache.
Side effect of medication
An acute drug-induced headache usually results from an adverse drug reaction ("side effect"). There are some substances that are known to cause headaches, for example drugs containing nitrates ("nitrate headaches"), antihypertensive drugs (calcium channel blockers), alcohol or caffeine.
Drug-induced headache as a result of pain medication
Many pain relievers are now available in pharmacies without a prescription. Some people are therefore not even aware that they can also be harmful. The cause of excessive use of pain relievers in most people is fear of renewed pain. Because of this, as a precaution, drugs are taken again and again, as a result of which a drug-induced headache slowly develops.
Drug-induced headache can in principle be triggered by all painkillers (analgesics) and in particular by drugs against migraines (triptans, ergotamines). How often the active ingredients are taken plays a decisive role. Examples of such drugs are:
- Non-steroidal anti-inflammatory drugs (NSAIDs) such as diclofenac, ibuprofen, paracetamol, acetylsalicylic acid, naproxen, ketoprofen, indomethacin, piroxicam and others
- Weakly effective opioids such as codeine, tilidine, tramadol, pentazocine and others
- Strongly effective opioids such as morphine, pethidine, hydromorphone, levomethadone, fentanyl and others
- Other drugs that are sometimes used for headaches such as benzodiazepines, barbiturates
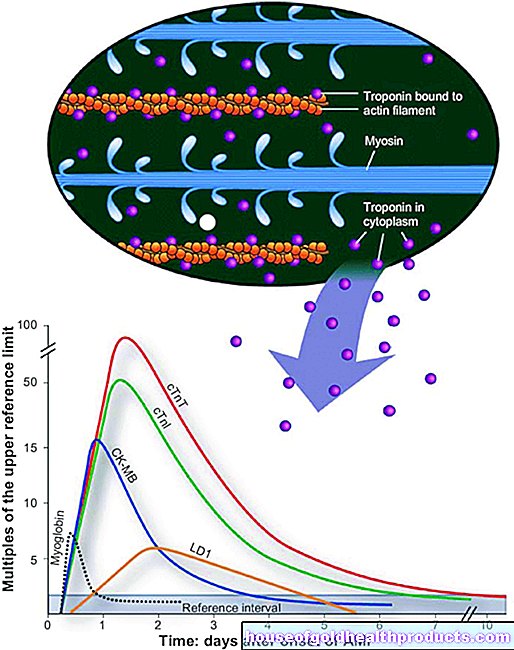
Researchers suspect that excessive use of pain relievers has effects on the metabolism of the brain. This lowers the limit from which pain is perceived. Those affected also perceive complaints that were previously considered normal by the body as painful. If this (head) pain is countered again with medication, the threshold is further reduced. This can create a vicious circle that patients can usually no longer break through on their own.
Drug-induced headache: risk factors
There are several risk factors that make drug-induced headaches more likely. These include:
- Taking anti-anxiety, relaxing medication (tranquilizers)
- Chronic complaints of the musculoskeletal or digestive system
- Obesity
- Low social status
- depression
- Nicotine use
Drug-induced headache: examinations and diagnosis
Drug-induced headache is recognized as such for most of those affected only after many years. Because many do not even know what drug-induced headache is and that their symptoms could be due to the painkillers. In the event of a possible diagnosis of “drug-induced headache”, it is therefore important first of all that you observe yourself closely. Do you take pain medication more than 10 days a month, and often more than three days in a row? Then you should definitely talk to a doctor about it.
The first point of contact if you suspect a “drug-induced headache” can be your family doctor. A specialist in neurology or a doctor with the additional qualification “special pain therapy” are also particularly suitable. During the anamnesis interview, the doctor will ask you questions about the current symptoms and any previous illnesses.
You should explain exactly why you were using pain medication and how often it was actually taken. It is helpful if you make a list of all the medications you have taken for the doctor before you go to the doctor. For a diagnosis, he will ask questions such as:
- Approximately how often do the headaches occur per month?
- What medications are you taking?
- How often do you take these drugs?
- Have you had a headache or other pain before?
- Can you describe the headache to me in more detail (location, type of pain, frequency)?
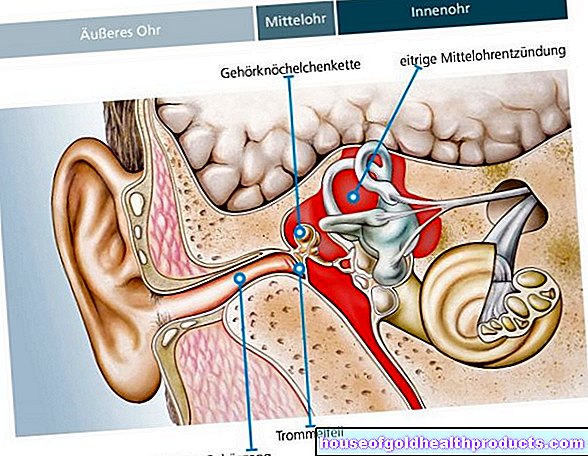
After the anamnesis, you will be examined neurologically. The doctor palpates the muscles in the shoulder, neck and head area. If the muscles are obviously tense in these areas, it may be an indication of a tension headache rather than a drug-induced headache. The doctor will also measure your blood pressure, as high blood pressure can also be a cause. Sometimes a blood sample is useful in order not to overlook abnormalities (e.g. increased inflammation values).
In the case of headaches of unknown cause, further examinations are usually necessary. These primarily include imaging procedures such as computed tomography (CT) or magnetic resonance imaging (MRT), which can be used to visualize the brain. In addition, special procedures are sometimes necessary, such as analyzing the nerve fluid (CSF puncture) and recording brain waves (electroencephalogram, EEG).
Drug-induced headache: making the diagnosis
To make a diagnosis, the doctor can rely on the diagnostic criteria developed by the International Headache Society (IHS). A drug-induced headache can be diagnosed if the following criteria are met:
- The headache is present for at least 15 days per month.
- Painkillers have been used for more than three months:
- on at least ten days per month (applies to ergotamine, triptans, opioids, combination pain relievers) or
- on at least 15 days / month (applies to all other painkillers - The headache developed or worsened significantly during the pain medication overuse.
- The headache subsides or returns to its previous pattern after the overuse of drugs is stopped.
A clear diagnosis is often only possible after drug withdrawal has been carried out. If the headache then subsides or becomes noticeably weaker, it is almost certainly a drug-induced headache.
Drug-induced headache: treatment
Since drug-induced headache is caused by drug intake, the most important treatment measure is to stop the triggering drug (drug withdrawal). However, it is not a withdrawal in the psychiatric sense, as it is used, for example, in drug addicts, since the headache medication (with the exception of the opioids) does not make you physically dependent.
Withdrawal leads to more or less severe withdrawal symptoms. These should also be treated by a doctor, otherwise a relapse with repeated use of painkillers is likely. Not least because both drug-induced headache and withdrawal are psychologically stressful, the treatment should be supplemented with behavioral therapy.
Drug withdrawal
Drug withdrawal can be carried out on an outpatient, partial inpatient basis in a day clinic or as an inpatient. Some drugs may not be stopped immediately, including opioids, benzodiazepines, and barbiturates. This means that the dose is gradually reduced. This prevents serious complications. Triptans, ergotamines and all other pain relievers, on the other hand, are stopped abruptly.
Drug-induced headache can be done in outpatient withdrawal. This means that those affected carry out the withdrawal at home and are accompanied by a doctor or a specialized pain therapist. It demands a lot of self-discipline from the patient and is not easy. It should therefore only be attempted under certain conditions:
- Taking painkillers without taking codeine or sedatives (tranquilizers)
- Drug-induced headache for no more than five years
- The patient is highly motivated
- Support from family or friends
- Stable home environment
Drug-induced headache can also be treated as part of inpatient withdrawal. This takes place in a specialized headache clinic. Those affected stay here for several days and carry out the withdrawal under medical supervision. In addition, various options for alternative pain treatment, such as stress management training or progressive muscle relaxation, are shown and trained. Inpatient withdrawal should be performed if one or more of the following is true:
- Longstanding drug-induced headache
- Additional use of sleeping pills, sedatives (tranquilizers) or anti-anxiety drugs (anxiolytics)
- Regular use of migraine medicines that contain codeine
- Several unsuccessful attempts at self-withdrawal
- Fear of outpatient withdrawal
- High performance standards and fear of failure
- Little family support
- Pronounced accompanying depression
Treatment of withdrawal symptoms
The pain reliever must be completely avoided during withdrawal. This can lead to withdrawal symptoms (especially in the first two to six days). In the beginning there is usually an increase in headaches. Symptoms such as nausea, increased blood pressure, palpitations, anxiety, nervousness and sleep disorders can also occur.
The withdrawal symptoms of the drug-induced headache are easily treatable during inpatient therapy. For example, pronounced symptoms can also be treated with various infusions. Due to the constant monitoring, many affected persons also have more confidence and are (also inevitably) more consistent in carrying out the withdrawal. This is not possible on an outpatient basis. The quota of those who relapse after an inpatient withdrawal is probably a little lower than in the case of an outpatient withdrawal.
Headache prophylaxis
If a primary headache (migraine, tension headache) originally led to excessive drug intake, this headache should be prevented with special drug prophylaxis.Scientific studies have shown that the active ingredient topiramate is good for the prevention of migraine attacks in migraineurs and medication overuse at the same time. Such migraine sufferers should be treated with botulinum toxin (“botox”) injections in addition to topiramate. Prophylaxis drugs are usually not addictive.
Drug-induced headache: disease course and prognosis
An exact prognosis is not possible with this type of headache. Drug-induced headache is primarily a question of behavior. Withdrawal from medication is at least remotely comparable to drug withdrawal: not all those affected manage to do without it permanently.
In particular, people who suffer from chronic pain and therefore often resort to painkillers should always seek advice from a doctor who specializes in pain in order to prevent drug-induced headaches.
Lots of relapses
There is no precise information on how many people with drug-induced headache remain symptom-free after treatment. In a study by the University of Münster, a relapse rate of four to 49 percent is given. Most relapses occur within the first year of treatment despite successful withdrawal therapy. Taking painkillers again often means again quickly: drug-induced headache. The time it takes for the symptoms to set in again after repeated drug abuse is reduced each time.
There are certain factors that affect the likelihood of relapse. According to this, those affected who have only had drug-induced headache for a period of less than five years, as well as patients who have only taken one preparation and not several at the same time, have more favorable prognoses.
Physical consequences of excessive use of pain medication
In addition, drug-induced headache is not the only consequence of misuse of drugs. Excessive “drug consumption” can also cause severe organic damage such as kidney damage, gastric and duodenal ulcers or tumors of the urinary tract. In addition, those affected often suffer from symptoms of depression. These symptoms will improve after you stop taking the drug.
Sparing use of medication is recommended
It is important to note that drug-induced headache can in principle be caused by all types of pain relievers if they are taken too often. The best way to prevent this type of headache from occurring is to closely monitor your own medication intake. Basically, the recommendation is not to take pain medication for more than ten days per month and not more than three days in a row. You don't have to do without it in the case of severe pain. However, it is preferable to treat mild pain with non-drug methods, as this reduces the risk of being diagnosed with “drug-induced headache”.
Tags: healthy feet digital health medicinal herbal home remedies